Abstract
Purpose
The neonatal period is the most vulnerable period for a child. There is a paucity of data on the burden of neonatal surgical disease in our setting. The aim of this study was to describe the frequency with which index neonatal surgical conditions are seen within our setting and to document the 30-day outcome of these patients.
Methods
This was a single-centre prospective observational study in which all neonates with paediatric surgical pathology referred to the paediatric surgical unit with a corrected gestational age of 28 days were included.
Results
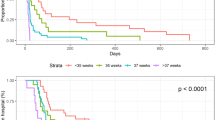
Necrotising enterocolitis was the most frequent reason for referral to the paediatric surgical unit (n = 68, 34.34%). Gastroschisis was the most frequent congenital anomaly referred (n = 20, 10.10%). The overall morbidity was 57.58%. Surgical complications contributed to 18.51% of morbidities. The development of gram negative nosocomial sepsis was the most frequent cause of morbidity (n = 98, 50.78%). Mortality at 30 days was 21.74% (n = 40). Sepsis contributed to mortality in 35 patients (87.5%), 16 of which had gram negative sepsis.
Conclusion
Gram-negative sepsis was a major contributing factor in the development of morbidity and mortality in our cohort. Prevention and improvement in infection control are imperative if we are to improve outcomes in our surgical neonates.


Similar content being viewed by others
References
UNICEF (2020) Neonatal mortality 2020 [22/01/2020]. https://data.unicef.org/topic/child-survival/neonatal-mortality/
World Health Organisation. Neonatal mortality https://www.who.int/gho/child_health/mortality/neonatal_text/en/
World Health Organisation (2018) Sustainable Development Goal 3: Health 2018. https://www.who.int/topics/sustainable-development-goals/targets/en/
Ameh EA, Seyi-Olajide JO, Sholadoye TT (2015) Neonatal surgical care: a review of the burden, progress and challenges in sub-Saharan Africa. Paediatr Int Child Health 35(3):243–251
Burstein R, Henry NJ, Collison ML, Marczak LB, Sligar A, Watson S et al (2019) Mapping 123 million neonatal, infant and child deaths between 2000 and 2017. Nature 574(7778):353–358
Lawn JE, Cousens S, Zupan J (2005) 4 million neonatal deaths: when? where? why? Lancet 365(9462):891–900
Ekenze SO, Ajuzieogu OV, Nwomeh BC (2016) Challenges of management and outcome of neonatal surgery in Africa: a systematic review. Pediatr Surg Int 32(3):291–299
World Health Organisation (2020) Children: improving survival and well being 2020. https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality
Ozgediz D, Jamison D, Cherian M, McQueen K (2008) The burden of surgical conditions and access to surgical care in low- and middle-income countries. Bull World Health Organ 86(8):646–647
Hyder AA, Wali SA, McGuckin J (2003) The burden of disease from neonatal mortality: a review of South Asia and Sub-Saharan Africa. Br J Obstet Gynaecol 110:894–901
UNICEF (2018) Child mortality estimates 2018 [updated 22 February 2018]
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Ugwu RO, Okoro PE (2013) Pattern, outcome and challenges of neonatal surgical cases in a tertiary teaching hospital. Afr J Paediatr Surg 10(3):226–230
Catre D, Lopes MF, Madrigal A, Oiveiros B, Viana JS, Cabrita AS (2013) Early mortality after neonatal surgery: analysis of risk factors in an optimized health care system for the surgical newborn. Rev Bras Epidemiol 16(4):943–952
Önder Özden İK, Çiftçi AÖ, Tanyel FC, Şenocak ME (2016) Factors affecting survival in neonatal surgery unit in a tertiary care university hospital during 26 years. Turk J Pediatr 58:457–463
Saggers RT, Ballot DE, Grieve A (2020) An analysis of neonates with surgical diagnoses admitted to the neonatal intensive care unit at Charlotte Maxeke Johannesburg Academic Hospital, South Africa. S Afr Med J 110(6):497–501
Romanelli RM, Anchieta LM, Carvalho EA, Gloria e Silva LF, Nunes RV, Mourao PH et al (2014) Risk factors for laboratory-confirmed bloodstream infection in neonates undergoing surgical procedures. Braz J Infect Dis 18(4):400–405
Segal I, Kang C, Albersheim SG, Skarsgard ED, Lavoie PM (2014) Surgical site infections in infants admitted to the neonatal intensive care unit. J Pediatr Surg 49(3):381–384
Olivier C, Kunneke H, O’Connell N, Von Delft E, Wates M, Dramowski A (2018) Healthcare-associated infections in paediatric and neonatal wards: a point prevalence survey at four South African hospitals. S Afr Med J 108(5):418–422
Dramowski A, Aucamp M, Bekker A, Mehtar S (2017) Infectious disease exposures and outbreaks at a South African neonatal unit with review of neonatal outbreak epidemiology in Africa. Int J Infect Dis 57:79–85
Dramowski A, Madide A, Bekker A (2015) Neonatal nosocomial bloodstream infections at a referral hospital in a middle-income country: burden, pathogens, antimicrobial resistance and mortality. Paediatr Int Child Health 35(3):265–272
Cristina ML, Sartini M, Spagnolo AM (2019) Serratia marcescens infections in neonatal intensive care units (NICUs). Int J Environ Res Public Health 16(4):610
Otake K, Uchida K, Kubo M, Yamamoto A, Nagano Y, Uratani R et al (2018) Clinical factors associated with in-hospital death in pediatric surgical patients admitted to the neonatal intensive care unit: a 15-year single tertiary center experience. J Pediatr Surg 53(3):499–502
Arnold M, Moore SW, Sidler D, Kirsten GF (2010) Long-term outcome of surgically managed necrotizing enterocolitis in a developing country. Pediatr Surg Int 26(4):355–360
Cotten CM (2019) Modifiable risk factors in necrotizing enterocolitis. Clin Perinatol 46(1):129–143
Gephart SM, Effken JA, McGrath JM, Reed PG (2013) Expert consensus building using e-Delphi for necrotizing enterocolitis risk assessment. J Obstet Gynecol Neonatal Nurs 42(3):332–347
Brindle ME, McDiarmid C, Short K, Miller K, MacRobie A, Lam JYK et al (2020) Consensus guidelines for perioperative care in neonatal intestinal surgery: enhanced recovery after surgery (ERAS((R))) society recommendations. World J Surg 44(8):2482–2492
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Withers, A., Cronin, K., Mabaso, M. et al. Neonatal surgical outcomes: a prospective observational study at a Tertiary Academic Hospital in Johannesburg, South Africa. Pediatr Surg Int 37, 1061–1068 (2021). https://doi.org/10.1007/s00383-021-04881-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04881-7