Abstract
Purpose
Low-grade glioma is the most common brain tumor among children and adolescents. When these tumors arise in the temporal lobe, patients frequently present with seizures that are poorly controlled with antiepileptic drugs. Here we summarize the clinical features, pathophysiology, preoperative evaluation, surgical treatment, and outcomes of pediatric patients with low-grade gliomas in the temporal lobe.
Methods
We reviewed the literature on pediatric low-grade gliomas in the temporal lobe, focusing on cohort studies and systematic reviews that described surgical treatment strategies and reported both oncologic and epilepsy outcomes.
Results
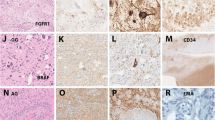
The differential diagnoses of pediatric low-grade gliomas in the temporal lobe include ganglioglioma, dysembryoplastic neuroepithelial tumor, desmoplastic infantile ganglioglioma, papillary glioneuronal tumor, pilocytic astrocytoma, pleomorphic xanthoastrocytoma, angiocentric glioma, and polymorphous low-grade neuroepithelial tumor of the young. There is no consensus on the optimal surgical approach for these tumors: lesionectomy alone, or extended lesionectomy with anterior temporal lobectomy, with or without removal of mesial temporal structures. Gross total resection and shorter preoperative duration of epilepsy are strongly associated with favorable seizure outcomes, defined as Engel Class I or Class II, approaching 90% in most series. The risk of surgical complications ranges from 4 to 17%, outweighing the lifetime risks of medically refractory epilepsy.
Conclusion
Pediatric patients with temporal low-grade glioma and tumor-related epilepsy are best managed by a multidisciplinary epilepsy surgery team. Early and appropriate surgery leads to prolonged survival and a greater likelihood of seizure freedom, improving their overall quality of life.



Similar content being viewed by others
Data availability
No datasets were generated or analyzed during the current study.
Abbreviations
- ATL:
-
Anterior temporal lobectomy
- DIG:
-
Desmoplastic infantile ganglioglioma
- DNET:
-
Dysembryoplastic neuroepithelial tumor
- ECoG:
-
Electrocorticography
- EEG:
-
Electroencephalography
- FCD:
-
Focal cortical dysplasia
- ILAE:
-
International League Against Epilepsy
- LEAT:
-
Long-term epilepsy associated tumor/low-grade developmental and epilepsy associated brain tumor
- LGG:
-
Low-grade glioma
- PGNT:
-
Papillary glioneuronal tumor
- PLNTY:
-
Polymorphous low-grade neuroepithelial tumor of the young
- PXA:
-
Pleomorphic xanthoastrocytoma
- WHO:
-
World Health Organization
References
Ostrom QT, Price M, Ryan K, Edelson J, Neff C, Cioffi G, Waite KA, Kruchko C, Barnholtz-Sloan JS (2022) CBTRUS statistical report: pediatric brain tumor foundation childhood and adolescent primary brain and other central nervous system tumors diagnosed in the United States in 2014–2018. Neuro-Oncol 24:iii1–iii38. https://doi.org/10.1093/neuonc/noac161
Ryall S, Zapotocky M, Fukuoka K, Nobre L, Stucklin AG, Bennett J, Siddaway R, Li C, Pajovic S, Arnoldo A, Kowalski PE, Johnson M, Sheth J, Lassaletta A, Tatevossian RG, Orisme W, Qaddoumi I, Surrey LF, Li MM, Waanders AJ, Gilheeney S, Rosenblum M, Bale T, Tsang DS, Laperriere N, Kulkarni A, Ibrahim GM, Drake J, Dirks P, Taylor MD, Rutka JT, Laughlin S, Shroff M, Shago M, Hazrati L-N, D’Arcy C, Ramaswamy V, Bartels U, Huang A, Bouffet E, Karajannis MA, Santi M, Ellison DW, Tabori U, Hawkins C (2020) Integrated molecular and clinical analysis of 1,000 pediatric low-grade gliomas. Cancer Cell 37:569-583.e5. https://doi.org/10.1016/j.ccell.2020.03.011
Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM, Reifenberger G, Soffietti R, von Deimling A, Ellison DW (2021) The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol 23:1231–1251. https://doi.org/10.1093/neuonc/noab106
Slegers RJ, Blumcke I (2020) Low-grade developmental and epilepsy associated brain tumors: a critical update 2020. Acta Neuropathol Commun 8:27. https://doi.org/10.1186/s40478-020-00904-x
Sievert AJ, Fisher MJ (2009) Pediatric Low-Grade Gliomas. J Child Neurol 24:1397–1408. https://doi.org/10.1177/0883073809342005
Jones DTW, Kieran MW, Bouffet E, Alexandrescu S, Bandopadhayay P, Bornhorst M, Ellison D, Fangusaro J, Fisher MJ, Foreman N, Fouladi M, Hargrave D, Hawkins C, Jabado N, Massimino M, Mueller S, Perilongo G, van Meeteren AYNS, Tabori U, Warren K, Waanders AJ, Walker D, Weiss W, Witt O, Wright K, Zhu Y, Bowers DC, Pfister SM, Packer RJ (2018) Pediatric low-grade gliomas: next biologically driven steps. Neuro-Oncol 20:160–173. https://doi.org/10.1093/neuonc/nox141
Qaddoumi I, Orisme W, Wen J, Santiago T, Gupta K, Dalton JD, Tang B, Haupfear K, Punchihewa C, Easton J, Mulder H, Boggs K, Shao Y, Rusch M, Becksfort J, Gupta P, Wang S, Lee RP, Brat D, Collins VP, Dahiya S, George D, Konomos W, Kurian KM, McFadden K, Serafini LN, Nickols H, Perry A, Shurtleff S, Gajjar A, Boop FA, Klimo PD, Mardis ER, Wilson RK, Baker SJ, Zhang J, Wu G, Downing JR, Tatevossian RG, Ellison DW (2016) Genetic alterations in uncommon low-grade neuroepithelial tumors: BRAF, FGFR1, and MYB mutations occur at high frequency and align with morphology. Acta Neuropathol 131:833–845. https://doi.org/10.1007/s00401-016-1539-z
Çataltepe O, Turanli G, Yalnizoglu D, Topçu M, Akalan N (2005) Surgical management of temporal lobe tumor—related epilepsy in children. J Neurosurg: Pediatr 102:280–287. https://doi.org/10.3171/ped.2005.102.3.0280
Iannelli A, Guzzetta F, Battaglia D, Iuvone L, Rocco CD (2000) Surgical treatment of temporal tumors associated with epilepsy in children. Pediatr Neurosurg 32:248–254. https://doi.org/10.1159/000028946
Uliel-Sibony S, Kramer U, Fried I, Fattal-Valevski A, Constantini S (2011) Pediatric temporal low-grade glial tumors: epilepsy outcome following resection in 48 children. Child’s Nerv Syst 27:1413. https://doi.org/10.1007/s00381-011-1454-5
Babini M, Giulioni M, Galassi E, Marucci G, Martinoni M, Rubboli G, Volpi L, Zucchelli M, Nicolini F, Marliani AF, Michelucci R, Calbucci F (2013) Seizure outcome of surgical treatment of focal epilepsy associated with low-grade tumors in children: clinical article. J Neurosurg: Pediatr 11:214–223. https://doi.org/10.3171/2012.11.peds12137
Bauer R, Ortler M, Seiz-Rosenhagen M, Maier R, Anton JV, Unterberger I (2014) Treatment of epileptic seizures in brain tumors: a critical review. Neurosurg Rev 37:381–388. https://doi.org/10.1007/s10143-014-0538-6
Pan I, LoPresti MA, Clarke DF, Lam S (2020) The effectiveness of medical and surgical treatment for children with refractory epilepsy. Neurosurgery 88:E73–E82. https://doi.org/10.1093/neuros/nyaa307
Widjaja E, Puka K, Speechley KN, Ferro MA, Connolly MB, Major P, Gallagher A, Almubarak S, Hasal S, Ramachandrannair R, Andrade A, Xu Q, Leung E, Snead OC, Smith ML (2023) Trajectory of health-related quality of life after pediatric epilepsy surgery. JAMA Netw Open 6. https://doi.org/10.1001/jamanetworkopen.2023.4858
Luyken C, Blümcke I, Fimmers R, Urbach H, Elger CE, Wiestler OD, Schramm J (2003) The spectrum of long-term epilepsy–associated tumors: long-term seizure and tumor outcome and neurosurgical aspects. Epilepsia 44:822–830. https://doi.org/10.1046/j.1528-1157.2003.56102.x
Thom M, Blümcke I, Aronica E (2012) Long-term epilepsy-associated tumors. Brain Pathol 22:350–379. https://doi.org/10.1111/j.1750-3639.2012.00582.x
Blumcke I, Spreafico R, Haaker G, Coras R, Kobow K, Bien CG, Pfäfflin M, Elger C, Widman G, Schramm J, Becker A, Braun KP, Leijten F, Baayen JC, Aronica E, Chassoux F, Hamer H, Stefan H, Rössler K, Thom M, Walker MC, Sisodiya SM, Duncan JS, McEvoy AW, Pieper T, Holthausen H, Kudernatsch M, Meencke HJ, Kahane P, Schulze-Bonhage A, Zentner J, Heiland DH, Urbach H, Steinhoff BJ, Bast T, Tassi L, Russo GL, Özkara C, Oz B, Krsek P, Vogelgesang S, Runge U, Lerche H, Weber Y, Honavar M, Pimentel J, Arzimanoglou A, Ulate-Campos A, Noachtar S, Hartl E, Schijns O, Guerrini R, Barba C, Jacques TS, Cross JH, Feucht M, Mühlebner A, Grunwald T, Trinka E, Winkler PA, Gil-Nagel A, Delgado RT, Mayer T, Lutz M, Zountsas B, Garganis K, Rosenow F, Hermsen A, Oertzen TJ von, Diepgen TL, Avanzini G, Consortium E (2017) Histopathological findings in brain tissue obtained during epilepsy surgery. N Engl J Med 377:1648–1656. https://doi.org/10.1056/nejmoa1703784
Fernández IS, Loddenkemper T (2017) Seizures caused by brain tumors in children. Seizure 44:98–107. https://doi.org/10.1016/j.seizure.2016.11.028
Rudà R, Bello L, Duffau H, Soffietti R (2012) Seizures in low-grade gliomas: natural history, pathogenesis, and outcome after treatments. Neuro-Oncol 14:iv55–iv64. https://doi.org/10.1093/neuonc/nos199
Ferrier CH, Aronica E, Leijten FSS, Spliet WGM, Huffelen ACV, Rijen PCV, Binnie CD (2006) Electrocorticographic discharge patterns in glioneuronal tumors and focal cortical dysplasia. Epilepsia 47:1477–1486. https://doi.org/10.1111/j.1528-1167.2006.00619.x
Zaatreh MM, Firlik KS, Spencer DD, Spencer SS (2003) Temporal lobe tumoral epilepsy. Neurology 61:636–641. https://doi.org/10.1212/01.wnl.0000079374.78589.1b
Harvey AS, Berkovic SF, Wrennall JA, Hopkins IJ (1997) Temporal lobe epilepsy in childhood; clinical, EEG, and neuroimaging findings and syndrome classification in a cohort with new-onset seizures. Neurology 49:960–968. https://doi.org/10.1212/wnl.49.4.960
Ray A, Kotagal P (2005) Temporal lobe epilepsy in children: overview of clinical semiology. Epileptic Disord 7:299–307. https://doi.org/10.1684/j.1950-6945.2005.tb00131.x
Spencer S, Huh L (2008) Outcomes of epilepsy surgery in adults and children. Lancet Neurol 7:525–537. https://doi.org/10.1016/s1474-4422(08)70109-1
Gruber MD, Pindrik J, Damante M, Schulz L, Shaikhouni A, Leonard JR (2023) Epileptic versus neuro-oncological focus of management in pediatric patients with concurrent primary brain lesion and seizures: a systematic review. J Neurosurg: Pediatr 32:1–8. https://doi.org/10.3171/2023.6.peds22440
Ranger A, Diosy D (2015) Seizures in children with dysembryoplastic neuroepithelial tumors of the brain—a review of surgical outcomes across several studies. Child’s Nerv Syst 31:847–855. https://doi.org/10.1007/s00381-015-2675-9
Fontana E, Negrini F, Francione S, Mai R, Osanni E, Menna E, Offredi F, Darra F, Bernardina BD (2006) Temporal lobe epilepsy in children: electroclinical study of 77 cases. Epilepsia 47:26–30. https://doi.org/10.1111/j.1528-1167.2006.00873.x
Oller-Daurella L, Oiler LFV (1989) Partial epilepsy with seizures appearing in the first three years of life. Epilepsia 30:820–826. https://doi.org/10.1111/j.1528-1157.1989.tb05345.x
Gelabert-Gonzalez M, Serramito-García R, Arcos-Algaba A (2011) Desmoplastic infantile and non-infantile ganglioglioma. Review of the literature. Neurosurg Rev 34:151–158. https://doi.org/10.1007/s10143-010-0303-4
Aronica E, Leenstra S, van Veelen CWM, van Rijen PC, Hulsebos TJ, Tersmette AC, Yankaya B, Troost D (2001) Glioneuronal tumors and medically intractable epilepsy: a clinical study with long-term follow-up of seizure outcome after surgery. Epilepsy Res 43:179–191. https://doi.org/10.1016/s0920-1211(00)00208-4
Nickels KC, Wong-Kisiel LC, Moseley BD, Wirrell EC (2012) Temporal lobe epilepsy in children. Epilepsy Res Treat 2012. https://doi.org/10.1155/2012/849540
Tomita T, Volk JM, Shen W, Pundy T (2016) Glioneuronal tumors of cerebral hemisphere in children: correlation of surgical resection with seizure outcomes and tumor recurrences. Child’s Nerv Syst 32:1839–1848. https://doi.org/10.1007/s00381-016-3140-0
Wolf HK, Müller MB, Spänle M, Zenther J, Schramm J, Wiestler OD (1994) Ganglioglioma: a detailed histopathological and immunohistochemical analysis of 61 cases. Acta Neuropathol 88:166–173. https://doi.org/10.1007/bf00294510
Park YW, Vollmuth P, Foltyn-Dumitru M, Sahm F, Choi KS, Park JE, Ahn SS, Chang JH, Kim SH (2023) The 2021 WHO classification for gliomas and implications on imaging diagnosis: part 3—summary of imaging findings on glioneuronal and neuronal tumors. J Magn Reson Imaging 58:1680–1702. https://doi.org/10.1002/jmri.29016
Chang EF, Christie C, Sullivan JE, Garcia PA, Tihan T, Gupta N, Berger MS, Barbaro NM (2010) Seizure control outcomes after resection of dysembryoplastic neuroepithelial tumor in 50 patients: clinical article. J Neurosurg Pediatr 5:123–130. https://doi.org/10.3171/2009.8.peds09368
Takahashi A, Hong S-C, Seo DW, Hong SB, Lee M, Suh Y-L (2005) Frequent association of cortical dysplasia in dysembryoplastic neuroepithelial tumor treated by epilepsy surgery. Surg Neurol 64:419–427. https://doi.org/10.1016/j.surneu.2005.02.005
VandenBerg SR, May EE, Rubinstein LJ, Herman MM, Perentes E, Vinores SA, Collins VP, Park TS (1987) Desmoplastic supratentorial neuroepithelial tumors of infancy with divergent differentiation potential (“desmoplastic infantile gangliogliomas”): report on 11 cases of a distinctive embryonal tumor with favorable prognosis. J Neurosurg 66:58–71. https://doi.org/10.3171/jns.1987.66.1.0058
Xiao H, Ma L, Lou X, Gui Q (2011) Papillary glioneuronal tumor: radiological evidence of a newly established tumor entity. J Neuroimaging 21:297–302. https://doi.org/10.1111/j.1552-6569.2010.00478.x
Pages M, Lacroix L, Tauziede-Espariat A, Castel D, Daudigeos-Dubus E, Ridola V, Gilles S, Fina F, Andreiuolo F, Polivka M, Lechapt-Zalcman E, Puget S, Boddaert N, Liu X, Bridge JA, Grill J, Chretien F, Varlet P (2015) Papillary glioneuronal tumors: histological and molecular characteristics and diagnostic value of SLC44A1-PRKCA fusion. Acta Neuropathol Commun 3:85. https://doi.org/10.1186/s40478-015-0264-5
Clark GB, Henry JM, McKeever PE (1985) Cerebral pilocytic astrocytoma. Cancer 56:1128–1133. https://doi.org/10.1002/1097-0142(19850901)56:5<1128::aid-cncr2820560529>3.0.co;2-j
Koeller KK, Rushing EJ (2004) Pilocytic astrocytoma: radiologic-pathologic correlation. Radiographics 24:1693–1708. https://doi.org/10.1148/rg.246045146
Kepes JJ, Rubinstein LJ, Eng LF (1979) Pleomorphic xanthoastrocytoma: a distinctive meningocerebral glioma of young subjects with relatively favorable prognosis A study of 12 cases. Cancer 44:1839–1852. https://doi.org/10.1002/1097-0142(197911)44:5<1839::aid-cncr2820440543>3.0.co;2-0
Mallick S, Benson R, Melgandi W, Giridhar P, Rath GK (2018) Grade II pleomorphic xanthoastrocytoma; a meta-analysis of data from previously reported 167 cases. J Clin Neurosci 54:57–62. https://doi.org/10.1016/j.jocn.2018.05.003
Park YW, Vollmuth P, Foltyn-Dumitru M, Sahm F, Ahn SS, Chang JH, Kim SH (2023) The 2021 WHO classification for gliomas and implications on imaging diagnosis: part 2—summary of imaging findings on pediatric-type diffuse high-grade gliomas, pediatric-type diffuse low-grade gliomas, and circumscribed astrocytic gliomas. J Magn Reson Imaging 58:690–708. https://doi.org/10.1002/jmri.28740
Ida CM, Rodriguez FJ, Burger PC, Caron AA, Jenkins SM, Spears GM, Aranguren DL, Lachance DH, Giannini C (2015) Pleomorphic xanthoastrocytoma and long-term follow-up. Brain Pathol 25:575–586. https://doi.org/10.1111/bpa.12217
Shakur SF, McGirt MJ, Johnson MW, Burger PC, Ahn E, Carson BS, Jallo GI (2009) Angiocentric glioma: a case series: clinical article. J Neurosurg Pediatr 3:197–202. https://doi.org/10.3171/2008.11.peds0858
Huse JT, Snuderl M, Jones DTW, Brathwaite CD, Altman N, Lavi E, Saffery R, Sexton-Oates A, Blumcke I, Capper D, Karajannis MA, Benayed R, Chavez L, Thomas C, Serrano J, Borsu L, Ladanyi M, Rosenblum MK (2017) Polymorphous low-grade neuroepithelial tumor of the young (PLNTY): an epileptogenic neoplasm with oligodendroglioma-like components, aberrant CD34 expression, and genetic alterations involving the MAP kinase pathway. Acta Neuropathol 133:417–429. https://doi.org/10.1007/s00401-016-1639-9
Bale TA, Rosenblum MK (2022) The 2021 WHO classification of tumors of the central nervous system: an update on pediatric low-grade gliomas and glioneuronal tumors. Brain Pathol. https://doi.org/10.1111/bpa.13060
Brown MT, Boop FA (2016) Epilepsy surgery for pediatric low-grade gliomas of the cerebral hemispheres: neurosurgical considerations and outcomes. Child’s Nerv Syst 32:1923–1930. https://doi.org/10.1007/s00381-016-3162-7
Englot DJ, Berger MS, Barbaro NM, Chang EF (2012) Factors associated with seizure freedom in the surgical resection of glioneuronal tumors. Epilepsia 53:51–57. https://doi.org/10.1111/j.1528-1167.2011.03269.x
Jay V, Becker LE (1995) Surgical pathology of epilepsy resections in childhood. Semin Pediatr Neurol 2:227–236. https://doi.org/10.1016/s1071-9091(05)80034-8
Liu CQ, Zhou J, Qi X, Luan GM (2012) Refractory temporal lobe epilepsy caused by angiocentric glioma complicated with focal cortical dysplasia: a surgical case series. J Neuro-Oncol 110:375–380. https://doi.org/10.1007/s11060-012-0975-4
Najm I, Lal D, Vanegas MA, Cendes F, Lopes-Cendes I, Palmini A, Paglioli E, Sarnat HB, Walsh CA, Wiebe S, Aronica E, Baulac S, Coras R, Kobow K, Cross JH, Garbelli R, Holthausen H, Rössler K, Thom M, El-Osta A, Lee JH, Miyata H, Guerrini R, Piao Y, Zhou D, Blümcke I (2022) The ILAE consensus classification of focal cortical dysplasia: an update proposed by an ad hoc task force of the ILAE diagnostic methods commission. Epilepsia 63:1899–1919. https://doi.org/10.1111/epi.17301
Luyken C, Blümcke I, Fimmers R, Urbach H, Wiestler OD, Schramm J (2004) Supratentorial gangliogliomas: histopathologic grading and tumor recurrence in 184 patients with a median follow-up of 8 years. Cancer 101:146–155. https://doi.org/10.1002/cncr.20332
Marton E, Feletti A, Orvieto E, Longatti P (2007) Malignant progression in pleomorphic xanthoastrocytoma: personal experience and review of the literature. J Neurol Sci 252:144–153. https://doi.org/10.1016/j.jns.2006.11.008
Nadi M, Ahmad T, Huang A, Hawkins C, Bouffet E, Kulkarni AV (2016) Atypical teratoid rhabdoid tumor diagnosis after partial resection of dysembryoplastic neuroepithelial tumor: case report and review of the literature. Pediatr Neurosurg 51:191–198. https://doi.org/10.1159/000443405
Rumana CS, Valadka AB (1998) Radiation therapy and malignant degeneration of benign supratentorial gangliogliomas. Neurosurgery 42:1038–1043. https://doi.org/10.1097/00006123-199805000-00049
Gorbachuk M, Machetanz K, Weinbrenner E, Grimm F, Wuttke TV, Wang S, Ethofer S, Tatagiba M, Rona S, Honegger J, Naros G (2023) Robot-assisted stereoencephalography vs subdural electrodes in the evaluation of temporal lobe epilepsy. Epilepsia Open 8:888–897. https://doi.org/10.1002/epi4.12756
Ozlen F, Gunduz A, Asan Z, Tanriverdi T, Ozkara C, Yeni N, Yalcinkaya C, Ozyurt E, Uzan M (2010) Dysembryoplastic neuroepithelial tumors and gangliogliomas: clinical results of 52 patients. Acta Neurochir 152:1661–1671. https://doi.org/10.1007/s00701-010-0696-4
Robertson FC, Ullrich NJ, Manley PE, Al-Sayegh H, Ma C, Goumnerova LC (2018) The impact of intraoperative electrocorticography on seizure outcome after resection of pediatric brain tumors: a cohort study. Neurosurgery 85:375–383. https://doi.org/10.1093/neuros/nyy342
Englot DJ, Han SJ, Berger MS, Barbaro NM, Chang EF (2012) Extent of surgical resection predicts seizure freedom in low-grade temporal lobe brain tumors. Neurosurgery 70:921–928. https://doi.org/10.1227/neu.0b013e31823c3a30
Kirkpatrick PJ, Honavar M, Janota I, Polkey CE (1993) Control of temporal lobe epilepsy following en bloc resection of low-grade tumors. J Neurosurg 78:19–25. https://doi.org/10.3171/jns.1993.78.1.0019
Rosenow F, Lüders H (2001) Presurgical evaluation of epilepsy. Brain 124:1683–1700. https://doi.org/10.1093/brain/124.9.1683
Lombardi D, Marsh R, de Tribolet N (1997) Advances in stereotactic and functional neurosurgery 12, Proceedings of the 12th Meeting of the European Society for Stereotactic and Functional Neurosurgery, Milan 1996. Acta Neurochir Suppl 68:70–74. https://doi.org/10.1007/978-3-7091-6513-3_13
Sindou M, Guenot M (2003) Advances and technical standards in neurosurgery. Adv Tech Stand Neurosurg 28:315–343. https://doi.org/10.1007/978-3-7091-0641-9_6
Spencer DD, Spencer SS, Mattson RH, Williamson PD, Novelly RA (1984) Access to the posterior medial temporal lobe structures in the surgical treatment of temporal lobe epilepsy. Neurosurgery 15:667. https://doi.org/10.1097/00006123-198411000-00005
Jooma R, Yeh H, Privitera MD, Gartner M (1995) Lesionectomy versus electrophysiologically guided resection for temporal lobe tumors manifesting with complex partial seizures. J Neurosurg 83:231–236. https://doi.org/10.3171/jns.1995.83.2.0231
Wray CD, McDaniel SS, Saneto RP, Novotny EJ, Ojemann JG (2012) Is postresective intraoperative electrocorticography predictive of seizure outcomes in children? Clinical article. J Neurosurg: Pediatr 9:546–551. https://doi.org/10.3171/2012.1.peds11441
Engel J Jr, Ness PV, Rasmussen T, Ojemann L (1993) Outcome with respect to epileptic seizures. In: Engel J Jr (ed) Surgical treatment of the epilepsies. Raven Press, New York, pp 609–21
Ward R, Jones HM, Witt D, Boop F, Bouffet E, Rodriguez-Galindo C, Qaddoumi I, Moreira DC (2022) Outcomes of children with low-grade gliomas in low- and middle-income countries: a systematic review. JCO Glob Oncol 8. https://doi.org/10.1200/go.22.00199
Takeshima H, Kawahara Y, Hirano H, Obara S, Niiro M, Kuratsu J (2003) Postoperative regression of desmoplastic infantile gangliogliomas: report of two cases. Neurosurgery 53:979–984. https://doi.org/10.1227/01.neu.0000084165.60662.6d
Manoharan N, Liu KX, Mueller S, Haas-Kogan DA, Bandopadhayay P (2023) Pediatric low-grade glioma: targeted therapeutics and clinical trials in the molecular era. Neoplasia 36. https://doi.org/10.1016/j.neo.2022.100857
Jones-Gotman M, Zatorre RJ, Olivier A, Andermann F, Cendes F, Staunton H, McMackin D, Siegel AM, Wieser H-G (1997) Learning and retention of words and designs following excision from medial or lateral temporal-lobe structures. Neuropsychologia 35:963–973. https://doi.org/10.1016/s0028-3932(97)00024-9
Sîrbu C-A (2011) Dysembryoplastic neuroepithelial tumor and probable sudden unexplained death in epilepsy: a case report. J Méd Case Rep 5:441. https://doi.org/10.1186/1752-1947-5-441
Thurman DJ, Hesdorffer DC, French JA (2014) Sudden unexpected death in epilepsy: assessing the public health burden. Epilepsia 55:1479–1485. https://doi.org/10.1111/epi.12666
Jain P, Smith ML, Speechley K, Ferro M, Connolly M, Ramachandrannair R, Almubarak S, Andrade A, Widjaja E, Team PS (2020) Seizure freedom improves health-related quality of life after epilepsy surgery in children. Dev Med Child Neurol 62:600–608. https://doi.org/10.1111/dmcn.14390
Arocho-Quinones EV, Lew SM, Handler MH, Tovar-Spinoza Z, Smyth M, Bollo R, Donahue D, Perry MS, Levy ML, Gonda D, Mangano FT, Storm PB, Price AV, Couture DE, Oluigbo C, Duhaime A-C, Barnett GH, Muh CR, Sather MD, Fallah A, Wang AC, Bhatia S, Patel K, Tarima S, Graber S, Huckins S, Hafez DM, Rumalla K, Bailey L, Shandley S, Roach A, Alexander E, Jenkins W, Tsering D, Price G, Meola A, Evanoff W, Thompson EM, Brandmeir N, Workgroup PSLA (2020) Magnetic resonance–guided stereotactic laser ablation therapy for the treatment of pediatric brain tumors: a multiinstitutional retrospective study. J Neurosurg: Pediatr 26:13–21. https://doi.org/10.3171/2020.1.peds19496
Wang M, Tihan T, Rojiani AM, Bodhireddy SR, Prayson RA, Iacuone JJ, Alles AJ, Donahue DJ, Hessler RB, Kim JH, Haas M, Rosenblum MK, Burger PC (2005) Monomorphous angiocentric glioma: a distinctive epileptogenic neoplasm with features of infiltrating astrocytoma and ependymoma. J Neuropathol Exp Neurol 64:875–881. https://doi.org/10.1097/01.jnen.0000182981.02355.10
Wicks RT, Jermakowicz WJ, Jagid JR, Couture DE, Willie JT, Laxton AW, Gross RE (2016) Laser interstitial thermal therapy for mesial temporal lobe epilepsy. Neurosurgery 79:S83–S91. https://doi.org/10.1227/neu.0000000000001439
Acknowledgements
The authors would like to acknowledge the assistance of Dr. John Carlo B. Reyes and Dr. Edwin L. Muñoz of the Department of Laboratories, Philippine General Hospital, for interpreting the pathology slides and providing representative photomicrographs used in this manuscript.
Funding
No funding was obtained for this review article.
Author information
Authors and Affiliations
Contributions
REB conceptualized the article, performed the literature review, and drafted the manuscript. NW and WM critically reviewed the manuscript and provided supervision. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baticulon, R.E., Wittayanakorn, N. & Maixner, W. Low-grade glioma of the temporal lobe and tumor-related epilepsy in children. Childs Nerv Syst (2024). https://doi.org/10.1007/s00381-024-06468-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00381-024-06468-8