Abstract
Background
Diffuse neonatal hemangiomatosis (DNH) is a rare disorder typically recognized at birth or during the neonatal period. DNH involves three or more organ systems, including the central nervous system (CNS). In these cases, serious complications such as hemorrhages and obstructive hydrocephalus can develop.
Case report
We present a case of DNH with intracranial hypertension and CNS hemorrhagic lesions on the mesencephalic aqueduct, resulting in triventricular hydrocephalus, treated with endoscopic ventriculocisternostomy (ETV) and medical therapy.
Discussion
DNH is a rare condition that can involve the CNS with serious complications. From a review of the literature, we highlighted only two cases of DNH with brain involvement treated surgically. We report the successful outcome of ETV, along with surgical considerations, imaging findings, and the complete resolution of cerebral and skin lesions following medical therapy.
Conclusions
Medical therapy is not standardized and must be individualized. In patients who develop severe neurological symptoms such as obstructive hydrocephalus, surgery may be considered to avoid neurological sequelae.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diffuse neonatal hemangiomatosis (DNH) is a rare and often fatal condition that presents during the neonatal period [1]. It is characterized by numerous cutaneous and visceral hemangiomas with no evidence of malignancy, involving three or more organ systems, including the central nervous system (CNS) [1, 2]. We present a case of DNH with multiple cutaneous hemangiomas and the onset of cerebral hemorrhagic lesions and triventricular hydrocephalus. We describe the successful neurosurgical and medical combination therapy with a favorable outcome.
Patient presentation
A 9-week-old male infant presented multiple diffuse red skin lesions. These swellings gradually increased in number and size and were associated with subcutaneous harder blue lesions (Fig. 1). Neurological examination revealed progressive macrocrania associated with irritability and vomiting. A total body angio-MR study showed multiple diffuse vascular lesions in the brain, spinal cord, bones, muscles, and viscera. Brain lesions were disseminated, involving both supra- and infratentorial regions, with intense and homogeneous contrast enhancement. The largest lesions were deep within the cerebral and cerebellar hemispheres, particularly the one located in the right lenticular nucleus, which showed acute hemorrhage with vasogenic edema, leading to compression of the mesencephalic aqueduct and resulting in triventricular hydrocephalus (Fig. 2). An endoscopic ventriculocisternostomy (ETV) was performed on the same day. Surgical approach had included a transfontanellar access on the right, with navigation references to select the entry point and define the route for the 0° Gaab rigid endoscope. Fenestration was achieved between the mammillary bodies and the infundibulum of the pituitary gland using only a Fogarty balloon. During the procedure, we noted that the ventricular ependyma had a petechial appearance, but no significant hemorrhage occurred, and only minor bleeding was controlled with continuous irrigation. A post-operative MRI showed adequate flow signal through the stoma (Fig. 3). A biopsy was performed during hospitalization to study some ulcerated and bleeding lesions, which revealed papillary endothelial hyperplasia with no pathognomonic features of a specific entity. Genetic mutations (EIF2AK4, ACVRL1, BMPR1B, BMPR2, CAV1, ENG, KCNK3, SMAD9, NOTCH3, and WES sequences) were investigated with no evidence found. Therapy was initiated with Prednisone (2 mg/kg/day) and Propranolol (1 mg/kg/day). However, due to further massive epistaxis requiring a blood transfusion and no improvement, the therapeutic scheme was modified to combine Prednisone and Vincristine. After 3 weeks of therapy with no improvement, Vincristine was replaced by Rapamycin (0.8 ml/day) with ethical committee consent. The therapy was effective, with no more bleeding observed, and the lesions gradually became smaller and clearer with some desquamative features. The patient was discharged, and therapy continued at home, with Rapamycin doses adjusted based on blood levels, while corticosteroids were gradually decreased. Follow-up over 5 years confirmed the absence of new lesions (Fig. 3).
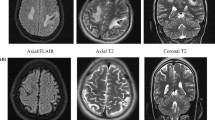
A, B At initial presentation in sagittal and axial T2-weighted images (T2WI) showing acute and multiple (nucleo-capsular right and tectal mesencephalic) ICH (intracerebral hemorrhages) with periventricular brain vasogenic edema of white matter. C, D DSA venous phase excluded arteriovenous malformation (AVM) and arteriovenous fistulas (AVFs)
A, B After 48 h of diagnosis: coronal and sagittal T2-weighted images (T2WI) showed a tectal mesencephalic hemorrhage with obstructive hydrocephalus due to aqueductal stenosis associated enlargement of the recesses of the third ventricle as finding of increased intracranial pressure. C After 24 h of surgery, a sagittal T2WI showed the cerebrospinal fluid flow artefact in the third ventricle sign of successful ETV. D After 10 years, a coronal MRI (T2WI) showed residual lacunar sequelae right nucleo-capsual and the regression of vascular lesions
Discussion
DNH is a rare but significant medical condition characterized by excessive growth and proliferation of hemangiomas [1, 2]. While the exact causes of DNH are not yet fully understood, it is believed to result from a combination of genetic and environmental factors, with some studies suggesting certain genetic predispositions may increase the risk of this condition [1]. The disease may present with various symptoms, but the presence of numerous cutaneous hemangiomas is a distinctive sign. Hemangiomas can also develop in internal organs such as the liver, brain, or intestines, leading to pain or discomfort in newborns, although sometimes this condition can be asymptomatic [2]. Rare associations of DNH with hemangioblastomas (HBLs) have been reported, contributing to the development of hydrocephalus [2, 3]. Diagnosis requires a thorough medical evaluation, including radiological imaging. Holden and Alexander proposed three minimal diagnostic criteria for DNH: onset in the neonatal period, no evidence of malignancy, and involvement of three or more organ systems [4]. In cases with extensive lesions present at birth, unusual cutaneous morphologies, or widespread internal organ involvement, a skin biopsy should be obtained for a precise histopathologic diagnosis of the vascular tumor.
Treatment for DNH depends on the severity and location of hemangiomas. In many cases, cutaneous hemangiomas may resolve spontaneously over time, making careful observation sufficient in some situations. [1] Steroids can be used to reduce the size of hemangiomas and prevent potential complications [1, 2, 5, 6]. Approximately 16% of hemangiomas do not respond to steroid therapy, and b-blockers are considered the first-line systemic therapy [1]. Storch et al. proposed several possible molecular targets for Propranolol treatment, depending on the timing of treatment [1, 7]. Vincristine has been described for the treatment of life-threatening or corticosteroid-resistant hemangiomas. Furthermore, treatment with Rapamycin has been proven effective in managing large and rapidly proliferating hemangiomas [1].
From a literature review, five cases of DNH with MRI findings of brain and/or spinal lesions were identified. Hydrocephalus was described in three cases [2, 3, 5]. Four of these cases utilized medical treatment, leading to a regression in the size and number of cutaneous and visceral hemangiomas [2, 5,6,7]. In two cases, a surgical approach was used for the treatment of hydrocephalus [2, 3] (Table 1).
In cases where hemangiomas cause significant problems or pose a risk to the patient’s life, surgical intervention may be necessary to remove or treat them. [1] In cases with diffuse skin lesions, invasive procedures such as tunneling for ventriculoperitoneal (VP) shunts carry a high risk of visceral or cutaneous and subcutaneous soft tissue injury. Thus, such procedures should be discouraged. Other alternatives can be temporary, such as the placement of a reservoir or an external ventricular drain. In rare cases like our patient’s, where acute obstructive hydrocephalus appeared in the presence of multiple cutaneous and visceral lesions, early endoscopic ventriculocisternostomy (ETV) can be performed.
Conclusions
In conclusion, DNH is a rare and complex clinical condition that requires timely and appropriate treatment [1]. Medical therapy is not standardized and must be individualized. In patients who develop severe neurological symptoms such as obstructive hydrocephalus, surgery may be considered to avoid neurological sequelae. In our case, the execution of an ETV associated with medical therapy made it possible to obtain complete resolution of the clinical. A study of the endoscopic trajectory and the floor of the third ventricle could be performed to improve the surgical technique.
References
Chen TS, Eichenfield LF, Friedlander SF (2013) Infantile hemangiomas: an update on pathogenesis and therapy. Pediatrics 131(1):99–108. https://doi.org/10.1542/peds.2012-1128. Epub 2012 Dec 24 PMID: 23266916
Patiroglu T, Sarici D, Unal E, Yikilmaz A, Tucer B, Karakukcu M, Ozdemir MA, Canoz O, Akcakus M (2012) Cerebellar hemangioblastoma associated with diffuse neonatal hemangiomatosis in an infant. Childs Nerv Syst 28(10):1801–1805. https://doi.org/10.1007/s00381-012-1858-x. Epub 2012 Jul 22 PMID: 22820755
Young RS, Zalneraitis EL, Bauman ML (1981) Disseminated neonatal hemangiomatosis: successful hepatic resection with subsequent development of hydrocephalus. J Pediatr Surg 16(5):752–753. https://doi.org/10.1016/s0022-3468(81)80572-6. PMID: 7310614
Holden KR, Alexander F (1970) Diffuse neonatal hemangiomatosis. Pediatrics 46(3):411–421. PMID: 5465931
Balaci E, Sumner TE, Auringer ST, Cox TD (1999) Diffuse neonatal hemangiomatosis with extensive involvement of the brain and cervical spinal cord. Pediatr Radiol 29:441–443
Al-Kaabi A, Yanofsky R, Bunge M, Hyman J, Rafay MF (2009) Diffuse hemangiomatosis with predominant central nervous system involvement. Pediatr Neurol 40(1):54–57. https://doi.org/10.1016/j.pediatrneurol.2008.09.022. PMID: 19068256
Okuno T, Tokuriki S, Yoshino T, Tanaka N, Ohshima Y (2015) Diffuse neonatal hemangiomatosis in a very low-birthweight infant treated with erythropoietin. Pediatr Int 57:e34–e36. https://doi.org/10.1111/ped.12517
Funding
Open access funding provided by Università degli Studi di Genova within the CRUI-CARE Agreement. No funds, grants or other support was received.
Author information
Authors and Affiliations
Contributions
All authors have contributed significantly to the content of the article and have read and have approved the submission of the manuscript
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The corresponding author accepts the responsibility for the integrity of the submitted work and attests that no undisclosed authors contributed to the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pavanello, M., Piro, L., Roggero, A. et al. A case report of hemorrhagic presentation of diffuse neonatal hemangiomatosis (DNH) associated to obstructive hydrocephalus: Medical and neurosurgical considerations. Childs Nerv Syst 40, 953–956 (2024). https://doi.org/10.1007/s00381-023-06226-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06226-2