Abstract
Toxoplasma gondii is a parasite that is estimated to infect one-third of the world’s population. It is acquired by ingesting contaminated water and food specially undercooked meat, contact with domestic or wild feline feces, and during pregnancy by transplacental transmission.
Immunocompetent hosts are usually asymptomatic, and infection will be self-limited, while those patients whose immune system is debilitated by HIV infection, immunosuppressive therapy, long-term steroid treatment, and fetuses infected during gestation will show evidence of systemic activity which is more severe in the central nervous system and eyes due to insufficient immune response caused by their respective blood barriers. Congenital toxoplasmosis has an estimated incidence of 8% in mothers who were seronegative at the beginning of their pregnancy. Infection in the first trimester may result in spontaneous abortion or stillbirth; however, it is estimated that the highest risk for vertical transmission is during the second and third trimesters when blood flow and placenta thickness favor parasitic transmission.
Congenital toxoplasmosis can be detected with periodic surveillance in endemic areas, and with appropriate treatment, the risk of vertical transmission can be reduced, and the severity of the disease can be reversed in infected fetuses.
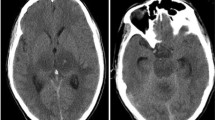
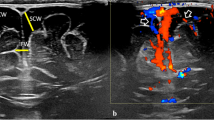
While most infected newborns will show no evidence of the disease, those who suffer active intrauterine complications will present with cerebral calcifications in 8–12% of cases, hydrocephalus in 4–30%, and chorioretinitis in 12–15%. Also, seizure disorders, spasticity, and varying degrees of neurocognitive deficits can be found in 12%.
Four distinct patterns of hydrocephalus have been described: aqueductal stenosis with lateral and third ventricle dilatation, periforaminal calcifications leading to foramen of Monro stenosis with associated asymmetrical ventricle dilatation, a mix of aqueductal and foramen of Monro stenosis, and overt hydrocephalus without clear evidence of obstruction with predominant dilatation of occipital horns (colpocephaly).
While all patients diagnosed with congenital toxoplasmosis should undergo pharmacological treatment, those presenting with hydrocephalus have traditionally been managed with CSF shunting; however, there are reports of at least 50% success when selected cases are treated with endoscopic third ventriculostomy. Successful hydrocephalus management with appropriate treatment leads to better intellectual outcomes.


Similar content being viewed by others
Availability of data and material
Not applicable.
References
Bollani L, Auriti C, Achille C et al (2022) Congenital toxoplasmosis: the state of the art. Front Pediatr 10:894573. https://doi.org/10.3389/FPED.2022.894573
Martin S (2001) Congenital toxoplasmosis. Neonatal Netw 20:23–30. https://doi.org/10.1891/0730-0832.20.4.23
Robert-Gangneux F, Dardé ML (2012) Epidemiology of and diagnostic strategies for toxoplasmosis. Clin Microbiol Rev 25:264–296. https://doi.org/10.1128/CMR.05013-11
Maldonado YA, Read JS, Byington CL et al (2017) Diagnosis, treatment, and prevention of congenital toxoplasmosis in the United States. Pediatrics 139. https://doi.org/10.1542/PEDS.2016-3860
Hampton MM (2015) Congenital toxoplasmosis: a review. Neonatal Netw 34:274–278. https://doi.org/10.1891/0730-0832.34.5.274
Curcio AM, Shekhawat P, Reynolds AS, Thakur KT (2020) Neurologic infections during pregnancy. Handb Clin Neurol 172:79–104. https://doi.org/10.1016/B978-0-444-64240-0.00005-2
Mc Auley J, Boyer KM, Patel D et al (1994) Early and longitudinal evaluations of treated infants and children and untreated historical patients with congenital toxoplasmosis: the Chicago Collaborative Treatment Trial. Clin Infect Dis 18:38–72. https://doi.org/10.1093/CLINIDS/18.1.38
Cabral CM, Tuladhar S, Dietrich HK et al (2016) Neurons are the primary target cell for the brain-tropic intracellular parasite Toxoplasma gondii. PLoS Pathog 12. https://doi.org/10.1371/JOURNAL.PPAT.1005447
Arora N, Sadovsky Y, Dermody TS, Coyne CB (2017) Microbial vertical transmission during human pregnancy. Cell Host Microbe 21:561–567. https://doi.org/10.1016/J.CHOM.2017.04.007
Campos FA, de Andrade GMQ, de Pádua Santos Lanna A et al (2014) Incidence of congenital toxoplasmosis among infants born to HIV-coinfected mothers: case series and literature review. Braz J Infect Dis 18:609–617. https://doi.org/10.1016/J.BJID.2014.05.008
Kieffer F, Wallon M (2013) Congenital toxoplasmosis. Handb Clin Neurol 112:1099–1101. https://doi.org/10.1016/B978-0-444-52910-7.00028-3
Lazarte-Rantes C, Rodríguez-Anccasi R, Rivas-Campos C, Silva E (2021) Congenital toxoplasmosis: findings in fetal MRI. Cureus 13. https://doi.org/10.7759/CUREUS.16894
McAuley J, Boyer K, Remington J, McLeod R (2014) Toxoplasmosis. In: Cherry J, Harrison G, Kaplan S (eds) Feigin and Cherry’s Textbook of Pediatric Infectious Diseases, 7th edn. Elsevier Saunders, Philadelphia, p 2897
Gonçalves FG, Caschera L, Teixeira SR et al (2020) Intracranial calcifications in childhood: part 1. Pediatr Radiol 50:1424–1447. https://doi.org/10.1007/S00247-020-04721-1
McLone D, Frim D, Penn R et al (2019) Outcomes of hydrocephalus secondary to congenital toxoplasmosis. J Neurosurg Pediatr 24:601–608. https://doi.org/10.3171/2019.6.PEDS18684
Serranti D, Buonsenso D, Valentini P (2011) Congenital toxoplasmosis treatment. Eur Rev Med Pharmacol Sci 15:193–198
McLeod R, Boyer K, Karrison T et al (2006) Outcome of treatment for congenital toxoplasmosis, 1981–2004: the National Collaborative Chicago-Based, Congenital Toxoplasmosis Study. Clin Infect Dis 42:1383–1394. https://doi.org/10.1086/501360
Hutson SL, Wheeler KM, McLone D et al (2015) Patterns of hydrocephalus caused by congenital toxoplasma gondii infection associate with parasite genetics. Clin Infect Dis 61:1831–1834. https://doi.org/10.1093/CID/CIV720
Khosla A, Singhal S, Jotwani P, Kleyman R (2022) Cerebral toxoplasmosis as the initial presentation of HIV: a case series. Cureus 14:e23359. https://doi.org/10.7759/cureus.23359
Dunphy L, Palmer B, Chen F, Kitchen J (2021) Fulminant diffuse cerebral toxoplasmosis as the first manifestation of HIV infection. BMJ Case Rep 14. https://doi.org/10.1136/bcr-2020-237120
Fard SA, Khajeh A, Khosravi A et al (2020) Fulminant and diffuse cerebral toxoplasmosis as the first manifestation of HIV infection: a case presentation and review of the literature. Am J Case Rep 21. https://doi.org/10.12659/AJCR.919624
Štajner T, Vujić D, Srbljanović J et al (2022) Risk of reactivated toxoplasmosis in haematopoietic stem cell transplant recipients: a prospective cohort study in a setting withholding prophylaxis. Clin Microbiol Infect 28:733.e1–733.e5. https://doi.org/10.1016/j.cmi.2021.09.012
Orang E, Sayyahfar S, Mahdavi M et al (2020) Comparison of serologic status of Toxoplasma gondii infection in pre- and post-heart transplantation in a pediatric population: a preliminary study. Transpl Infect Dis 22. https://doi.org/10.1111/tid.13339
Schwenk HT, Khan A, Kohlman K et al (2021) Toxoplasmosis in pediatric hematopoietic stem cell transplantation patients. Transplant Cell Ther 27:292–300. https://doi.org/10.1016/J.JTCT.2020.11.003
Mitchell W (2001) Neurological and developmental effects of HIV and AIDS in children and adolescents. Ment Retard Dev Disabil Res Rev 7:211–216. https://doi.org/10.1002/MRDD.1029
Cinalli G, Spennato P, Nastro A et al (2011) Hydrocephalus in aqueductal stenosis. Childs Nerv Syst 27:1621–1642. https://doi.org/10.1007/S00381-011-1546-2
Kaiser G (1985) Hydrocephalus following toxoplasmosis. Z Kinderchir 40(Suppl 1):10–11. https://doi.org/10.1055/S-2008-1059757
Cinalli G, Sainte-Rose C, Kollar EM et al (1998) Hydrocephalus and craniosynostosis. J Neurosurg 88:209–214. https://doi.org/10.3171/jns.1998.88.2.0209
Kulkarni AV, Sgouros S, Constantini S (2017) Outcome of treatment after failed endoscopic third ventriculostomy (ETV) in infants with aqueductal stenosis: results from the International Infant Hydrocephalus Study (IIHS). Childs Nerv Syst 33:747–752. https://doi.org/10.1007/S00381-017-3382-5
Koch D, Wagner W (2004) Endoscopic third ventriculostomy in infants of less than 1 year of age: which factors influence the outcome? Childs Nerv Syst 20:405–411. https://doi.org/10.1007/S00381-004-0958-7
Javadpour M, Mallucci C, Brodbelt A et al (2001) The impact of endoscopic third ventriculostomy on the management of newly diagnosed hydrocephalus in infants. Pediatr Neurosurg 35:131–135. https://doi.org/10.1159/000050406
Acknowledgements
The authors would like to thank Fabiola Caceres-Alan for creating the illustrations used in this article.
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Caceres, A., Caceres-Alan, A. & Caceres-Alan, T. Toxoplasma gondii infections in pediatric neurosurgery. Childs Nerv Syst 40, 295–301 (2024). https://doi.org/10.1007/s00381-023-05915-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-05915-2