Abstract
Purpose
Based on the success of deep brain stimulation (DBS) in the treatment of adult disorders, it is reasonable to assume that the application of DBS in the pediatric population is an emerging area worthy of study. The purpose of this paper is to outline the current movement disorder indications for DBS in the pediatric population, and to describe areas of investigation, including possible medically refractory psychiatric indications.
Methods
We performed a structured review of the English language literature from 1990 to 2011 related to studies of DBS in pediatrics using Medline and PubMed search results.
Results
Twenty-four reports of DBS in the pediatric population were found. Based on published data on the use of DBS for pediatric indications, there is a spectrum of clinical evidence for the use of DBS to treat different disorders. Dystonia, a disease associated with a low rate of remission and significant disability, is routinely treated with DBS and is currently the most promising pediatric application of DBS. We caution the application of DBS to conditions associated with a high remission rate later in adulthood, like obsessive-compulsive disorder and Tourette’s syndrome. Moreover, epilepsy and obesity are currently being investigated as indications for DBS in the adult population; however, both are associated with significant morbidity in pediatrics.
Conclusion
While currently dystonia is the most promising application of DBS in the pediatric population, multiple conditions currently being investigated in adults also afflict children and adolescents, and thus warrant further research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of pediatric neurological disorders often arises from modifications of treatments of similar conditions in adult patients. The use of neurostimulator devices, such as deep brain stimulators, in pediatric patients has an interesting but limited history. Deep brain stimulation (DBS) is the surgical treatment of choice for many adult patients with advanced Parkinson’s disease (PD) and other movement disorders and is under investigation for use in the treatment of psychiatric conditions like depression, obsessive compulsive disorder, obesity, and addiction [53, 58, 77, 92, 95]. The clinical, therapeutic effects of high frequency DBS appear to mimic those of stereotactic ablations, although modification (both activating and inhibitory) of neuronal activity and circuits may be the mechanism of action of DBS at varying frequencies [17, 32]. While DBS can produce effects similar to ablation, it also provides added safety and flexibility due to its reversibility and titratability [64, 122]. Based on results obtained in adult patients, it is reasonable to assume that the application of DBS in children is an emerging area worthy of further study.
While the application of DBS in adults continues to expand, pediatric indications for DBS have been more limited. Some have advised that this application in pediatric populations needs to be approached carefully [42], while others posit that DBS may be particularly suited to use in the developing brain. For example, its reversibility and titratability allow adjustment of the treatment throughout development and its relative preservation of anatomy without inducing significant tissue damage may allow for future treatment modalities even after DBS intervention [30]. Importantly, many of the adult patients who do not fare as well after DBS surgery for PD are elderly and have mild cognitive impairment prior to surgery [56]. This would not be as much of a concern in the pediatric population. Furthermore, as our understanding of the mechanism of DBS improves combined with the ability to dissect neural circuitry using novel techniques such as optogenetics [51, 75, 175], the applications of DBS in pediatrics will no doubt expand. Nevertheless, careful attention will need to be paid to the ethical and medical issues that apply to the pediatric community. Moreover, the purpose of this paper is to outline the current movement disorder indications for DBS in the pediatric population, and to describe areas of investigation, including possible medically refractory psychiatric indications
Deep brain stimulation for pediatric movement disorders
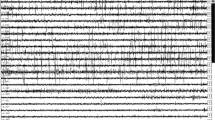
We performed a structured review of the English language literature from 1990 to 2011 related to studies of DBS in pediatrics using Medline and PubMed search engines. The search employed various combinations of key words, including “deep brain stimulation,” “pediatrics,” and “children,” and we expanded the search to include the terms “movement disorders,” “neuropsychiatric,” “psychiatric,” “basal ganglia,” “nucleus accumbens,” and “hypothalamus”. The search was expanded using the “Find Similar” and “Find Citing Articles” features of Medline and the “Related Articles” feature of PubMed, as well as the bibliographies of selected publications. We only included studies of DBS performed in the pediatric population (<21 years of age) or studies which clearly delineated the data obtained from adult and pediatric populations. Twenty-four reports of DBS in this age group were found and are summarized in Table 1. We excluded studies of DBS performed in adults.
Dystonia
The most common indication of DBS in the pediatric population to date is dystonia. Dystonia is defined as a syndrome of sustained muscle contractions, frequently causing twisting and repetitive movements or abnormal postures [38]. Prevalence estimates for primary dystonia fall between 111 and 3,000 per million, depending on the population and age of onset [31]. Dystonias can be classified as primary, where dystonia is the only clinical sign of disease, or secondary, where dystonia is secondary to another disease process such as traumatic brain injury [18, 74, 110]. Primary dystonias can be generalized (primary generalized dystonia), segmental (affecting adjoining parts of the body), or focal (affecting one muscle or a group of muscles). Many primary dystonias have been found to be associated with genetic mutations and deletions [110]. Medical management includes levodopa, anticholinergics, baclofen, botulinum toxin injections, and others, but these options do not relieve symptoms in all patients [135].
Intrathecal baclofen (ITB) administration has emerged as a surgical treatment option for both dystonia and spasticity in the pediatric population [126]. Baclofen is a GABA agonist that, in the case of dystonia and spasticity, is thought to exert its therapeutic effects on neurons in the spinal nerve roots and cortex. Baclofen can be administered orally, directly into the thecal sac, or intraventricularly. When administered orally, baclofen does not adequately cross the blood–brain barrier to impart its therapeutic effects. Thus, it is often administered directly into CSF, either as a bolus or as a continuous infusion, via a pump [7]. As a treatment for dystonia, both intraventricular and intrathecal baclofen (ITB) have been found to be associated with clinical improvement, although intrathecal administration has been more thoroughly examined [6, 8, 112]. In a trial of ITB for pediatric patients with dystonia, families of patients who received the treatment reported an increase in quality of life and ease of care of 86 %; reduced dystonia scores were also observed at follow-up of as long as 24 months [8]. Another study of patients receiving intraventricular baclofen for the treatment of generalized dystonia reported a reduction of mean Barry–Albright dystonia scores from 23 to 8 [6]. Secondary dystonias, such as those arising from cerebral palsy, tend to respond especially well to ITB therapy, while primary dystonias do not. Especially severe cases of dystonia, such as those associated with neurodegeneration with brain iron accumulation (NBIA), can respond suboptimally both to medical management and ITB. Risks associated with this treatment include surgical complications and baclofen withdrawal as a result of equipment malfunction, a potentially fatal event [7]. The incomplete efficacy of ITB therapy and pharmacotherapy in the treatment of dystonia has motivated the development of novel and more aggressive treatments such as DBS.
DBS has been approved under a humanitarian device exemption for use in the treatment of dystonias in both adults and children [98]. DBS of the globus pallidus internus (GPi) has been established as an effective, safe treatment for medically refractive dystonia in adults [166]. Choice of this target stems from the success of GPi pallidotomy in the treatment of patients with PD and generalized dystonia [54, 91]. Additionally, functional neuroimaging studies have revealed that GPi-DBS decreases activation of cortical areas that are normally hyperactivated in patients with dystonia [79]. In a randomized, controlled clinical trial with a sham stimulation arm, primary generalized dystonia (PGD) and segmental dystonias responded well to bilateral pallidal DBS, with significant improvements in disability, movement, and physical quality-of-life scores [80]. In addition to adults, this trial included a large proportion of pediatric subjects. Improvements in the Burke–Fahn–Marsden Dystonia Rating Scale (BFMDRS) movement score has been shown to last 36 months after the start of GPi-DBS [104]. GPi-DBS may also be effective for the treatment of focal cervical dystonia, as evidenced by two small series (n = 2 and n = 3) where decreased dystonia scores were seen up to 15 months after the start of DBS [73, 78]. Although dystonia is the most common pediatric indication for DBS, its effectiveness and safety in this population are not well established. Nevertheless, studies have reported favorable outcomes of GPi-DBS in pediatric patients with PGD as a result of the DYT1 mutation [30], which, according to a recent meta-analysis, appears to confer an advantage for symptomatic improvement compared with those without the mutation [21].
The durability of DBS has been supported by long-term trials [60]. In fact, one group has reported 10-year follow-up of a PGD patient who, at age 28, continues to enjoy the benefits of symptom reduction attributable to DBS [9]. General observations of these patients with ongoing stimulation include an increased effect in patients of a younger age and a maximum effect occurring about 3 years after implantation. One anecdotal report of improvement after DBS in a younger population suggests that intervention with DBS early in the course of PGD is advisable to prevent major disability and the suffering that goes with it [103].
DBS for secondary dystonias may not be as effective, given the variability in symptoms, comorbidities, and the fixed neurologic deficit associated with underlying structural abnormalities of the brain in these patients [37, 159, 166]. Secondary dystonias can arise as a consequence of trauma or neurological diseases like cerebral palsy (CP), NBIA, and Wilson’s disease. In a small, uncontrolled series of patients with dystonia secondary to CP, DBS of the GPi was found to offer significant improvements in disability and movement scores [97]. However, lead placement and targeting were variable, which the authors attributed to inconsistencies in clinical manifestations and neuroanatomical abnormalities in the patients. Dystonia secondary to NBIA can be treated with GPi-DBS, but reductions in dystonia severity are generally not as durable or dramatic in degenerative conditions as for primary dystonias [159].
Tourette’s syndrome
Tourette’s syndrome (TS) is a neuropsychiatric disorder characterized by chronic motor and vocal tics that usually presents in childhood, often in combination with concomitant behavioral disorders including obsessive compulsive disorder (OCD) and attention deficit hyperactivity disorder [81]. Tics are brief movements or sounds that occur intermittently and unpredictably. They can arise from direct brain injury, but more often are associated with TS or other idiopathic tic disorders [157]. The tics associated with TS give relief of a premonitory sensation that is often localizable to the region of the tic and described as an itching, urge, or otherwise uncomfortable sensation [65, 82]. Tics can be vocal or motor, are commonly suppressible (under voluntary control), and are often mixed, occurring with varying frequency and intensity in any given patient, depending on environmental factors like stress, concentration, and social awareness [81]. Tic onset occurs at around 4–6 years of age followed by progressive increase in tic severity until an average of 10–12 years of age, followed by a decrease in intensity such that 50 % at age 18 were free of tics [19, 84]. The prevalence of TS in school-aged children ranges from 0.5 % to 3 % depending on the population studied and the clinical criteria employed [132].
Current management strategies for TS include behavioral and medical interventions. Medical therapy includes, in order of priority, use of alpha-adrenergic agonists (e.g., clonidine, guanfacine), neuroleptics (e.g., haloperidol, risperidone), and the catecholamine blocking agent tetrabenazine, depending on severity of the tic disorder. The effectiveness of traditional and atypical neuroleptics has been confirmed in placebo-controlled trials [35, 134, 139, 144], but the side effects of these classes of D2 antagonists are significant and include sedation, parkinsonism, dystonia, tardive dyskinesia, weight gain, metabolic disorders, and others [130]. These side effects are important to consider when treating TS since chronic use of these drugs begins at such a young age and side effects like sedation may interfere with school work and metabolic effects may have a larger lifetime impact on health. Due to its localized effects, botulinum toxin (BTX) injection may be particularly effective in patients who report a prominent premonitory sensation and an isolated motor tic. The toxin is injected into a muscle group associated with the tic and has been shown to reduce motor tic severity by 39 % in a placebo-controlled study, but benefit from BTX in reducing vocal tics has not been established [83, 99, 147]. The side effects and varying efficacy of current medical management of tics in TS have motivated the development of surgical interventions like ablative surgery and DBS.
Ablative surgery has been under investigation for the treatment of intractable TS since at least 1961. Targets for ablation have included the thalamus, cingulate gyrus, frontal, and pre-frontal cortex, and others [156]. Side effects include cognitive deficits, hemiparesis, confusion, dysarthria, dystonia, temporary loss of speech, and hemiballism [15, 156]. While some of these side effects were transient, others were permanently disabling, motivating the investigation of DBS as an alternative.
Reports of DBS for TS have largely been limited to the adult population, with the exception of case reports in adolescents. Targets of stimulation vary and include the anteromedial and posteroventral GPi [100], the centromedian–parafascicular (Cm–PoF) nuclear complex of the thalamus, the ventralis–oralis (Voa) complex of the thalamus [5, 128], the subthalamic nucleus (STN) [101], ventral capsule/ventral striatum (VC/VS), and nucleus accumbens (NAc) [174]. Reports of stimulation at these sites show improvement in tic symptoms and in many associated, non-tic symptoms of TS, like self injurious behavior and compulsions, depending on the target [24]. The thalamus is the most common target, as reported in one observational series of 18 patients, whereby tic severity was reduced by 64 % after Cm–PoF/Voa stimulation [142]. No adverse behavioral side effects were seen and improvements in comorbid obsessive compulsive behavior, OCD, SIB, and anxiety symptoms were substantial. A clinical trial of thalamic Cm–PoF/Voa–DBS for TS in which patients were blindly and randomly assigned to stimulation or non-stimulation arms showed a reduction in tic severity of 49 % at 1 year [5]. Side effects of DBS included gaze disturbances and reduced energy levels.
The NAc, with its central role in dopaminergic transmission, is a particularly interesting target for the treatment of TS because of the putative implication of dopamine in the pathogenesis of the disease (as evidenced by the effectiveness of D2 antagonists for treatment of tics) [123, 138, 152]. Stimulation of NAc in a single patient with intractable TS and comorbid OCD was reported to have substantially mitigated the motor and vocal tics as well as concomitant symptoms of OCD, evidenced by a decrease in the Yale Global Tic Severity Scale (YGTSS) and increase in global assessment of functioning [77]. In another single case report, a 38-year-old man with intractable TS and comorbid OCD showed a marked reduction in YGTSS total score, Yale–Brown Obsessive Compulsive Scale (YBOCS), and Rush Video Rating Scale, for 36 months after bilateral DBS of the NAc. Self-injurious behavior and smoking also resolved after the procedure [115]. In contrast to these positive reports, a patient with mild TS but severe OCD was more symptomatic after DBS of VC/VS [23].
DBS for TS in children has not been widely evaluated and case reports have been limited to adolescents, including a 16-year-old with intractable TS who improved substantially after bilateral GPi-DBS. Scores for tic severity decreased by 76 % (motor) and 68 % (vocal), and the impairment score decreased by 100 % at 6 months’ follow-up with improvement in comorbid OCD symptoms and quality of life (SF-36) [143]. However, in another report of a 16-year-old with a similar clinical story, DBS of GPi was ineffective. The authors of this second case attribute the difference in outcome a variety of factors, including differences in drug treatment, the presence of an intellectual impairment, and the natural heterogeneity of TS [36]. In a larger series of mostly adult patients undergoing DBS for TS, two patients, ages 17 and 19, underwent Cm–PoF–DBS and, according to the YGTSS, experienced a reduction in tic severity of 69 % (the 17-year-old) and 45 % (the 19-year-old) [142]. No adverse outcomes were seen in these two patients. Anti-tic medication was still required after surgery in both. Long-term outcomes of more than a year have not yet been reported for this age group, and it is not known whether any of the operated patients may have had a reduction in symptoms as would be expected given the natural history of TS. Procedures and outcomes for DBS of these novel targets have not been well established, and thus, many of the side effects are unpredictable. The possibility of unintended psychiatric effects should not prevent the application of DBS to diseases like TS because patients in these situations gain significant symptomatic relief once the psychiatric problems are addressed. The range of these effects and procedures for avoiding and addressing them need to be well established as the field carves a largely cautious path to the application of DBS for TS in a wider pediatric population. In addition to these concerns about the side effects of DBS and the wide variety of targets available for stimulation, application of DBS for TS in young patients is complicated by the variability of disease course. It is reported that 33–50 % of children see a resolution of their tic symptoms at age 18, and about 75 % will see a marked reduction in tic symptoms at the same age [19, 84]. Given the likelihood that symptoms of TS will subside as those affected grow into adulthood, it may be inappropriate to extend DBS treatment for TS to children under a certain age before which it is impossible to determine a probability for symptomatic reduction as a part of the course of the illness.
Juvenile parkinsonism
Idiopathic Parkinson’s disease (PD), a progressive neurodegenerative disorder, is characterized by bradykinesia, resting tremor, rigidity, and postural reflex impairment most often with an onset of symptoms at about 60 years of age [85, 172]. At autopsy, neuronal degeneration can be found in a number of subcortical sites, especially the dopamine producing cells of substantia nigra in the mesencephalon, and throughout the brain there is an abundance of abnormal deposits in neuronal cytoplasm of the presynaptic protein alpha-synuclein in the form of immunostain-positive Lewy bodies. Juvenile parkinsonism (JP) is defined as the development of parkinsonian symptoms or signs before the age of 21, while young-onset PD is defined as onset between the ages of 21 and 40 [131, 141]. Patients with JP experience many of the same symptoms as older-onset PD patients, including tremor, bradykinesia, and focal dystonia [140]. Although JP usually resembles adult-onset PD clinically, including a variable natural history and levodopa responsiveness, the etiology of JP is more likely to be genetic. For example, mutations in the parkin and PTEN-induced putative kinase 1 (PINK1) genes have been found in these patients and their families. Additional etiologic factors, such as exposure to possible environmental toxins, have been postulated [158]. Pharmacotherapy of PD and JP includes a variety of dopamine replacement or dopamine enhancing strategies, using the dopamine precursor levodopa and other drugs. Unfortunately, as seen in adults with advanced PD, l-dopa treatment is associated with adverse motor effects such as dyskinesias, focal dystonia, and motor fluctuations. These adverse effects emerge within only a few years of treatment initiation in adult-onset PD [65], and in one group of JP patients, adverse effects were observed after a median time of only 6 months [140]. Given the early onset of JP, this brevity of treatment efficacy with l-dopa is potentially a more significant problem than in the treatment of adult onset PD. Thus, alternative treatments to reduce or delay the development of these motor side effects would be important in the treatment of JP.
DBS of the STN and GPi has been highly successful in the treatment of a subpopulation of patients with adult onset PD [43]. DBS has not been reported for pediatric treatment of JP, but has shown some success in limited reports in adults with PD secondary to mutations that are often implicated in JP. In one series, seven adult patients with two parkin mutations responded well to STN-DBS and after 12 months required lower doses of l-dopa than a control group of PD patients medically managed without surgery [90]. In another series of early onset PD patients undergoing bilateral STN-DBS, those with mutations in the parkin or PINK1 gene were found at 3-year follow-up to respond similarly to historical controls with idiopathic PD [111]. Given that such mutations—and others yet to be identified—are increasingly being found in patients with JP, DBS may be an appropriate therapeutic approach in carefully selected cases. Of course, application of DBS to pediatric JP patients will hinge on determining the underlying disease process in each case. While DBS may offer symptomatic relief in pediatric patients with parkin and/or PINK1 mutations, it may not have the same effectiveness in patients with JP secondary to other causes like mitochondrial disease, environmental exposure, or other neurodegenerative conditions. If DBS is found to be effective in cases of parkin- or PINK1-associated JP, genetic analyses and assessment of family history will be important in the routine evaluation of potential DBS candidates to ensure proper patient selection.
Deep brain stimulation for pediatric psychiatric disorders
OCD
Obsessive-compulsive disorder (OCD) is a heterogeneous neuropsychiatric disease characterized by obsessional symptoms and compulsive acts that cause distress and interfere with daily activities [1, 4]. The cognitive behavioral model of OCD states, roughly, that obsessions cause significant distress while the associated compulsions reduce this distress. The DSM-IV certifies the diagnosis of OCD in children even without insight into the unreasonableness of their obsessions, as is normally required for diagnosis in adults [1]. Comorbidities, including anxiety, depression, and eating disorders, are common with a diagnosis of OCD, occurring in nearly 70 % of OCD patients over a lifetime [66]. OCD has a significant impact on the pediatric population, with an age of onset commonly at about 10 years and a prevalence in children and adolescents of up to 3 %, with subclinical rates of OCD at about 19 % [151, 162]. While 40 % of individuals experience a remission of symptoms, those with early-onset and high severity are at increased risk for persistent disability [148, 151].
OCD is purported to arise from a disturbance of cortico-striato-thalamo-cortical circuits as evidenced by numerous functional and structural imaging studies, including diffusion-tensor imaging of the white matter tracts and measurements of metabolic activity in various regions in these circuits [26, 61, 136, 137]. A meta-analysis of functional imaging of OCD abnormalities has suggested that there are reliable increases in the apparent activity of the head of the caudate nucleus in subjects with OCD but that this difference does not directly provide evidence of involvement of this region in the pathogenesis of the disease. Many brain structures purportedly involved have not been found to be consistently hypo- or hyper-activated in OCD subjects when compared with controls [170]. In addition to abnormal functional anatomy in the pathogenesis of OCD, genetic influences have also been identified. Twin studies have found monozygotic and dizygotic concordance rates that suggest a substantial genetic determinant in the development of obsessive compulsive symptoms [124]. Biochemical dysregulation of serotonin is suggested by the therapeutic effectiveness of selective serotonin reuptake inhibitors (SSRIs), but the results of SSRI therapy in this setting have not been consistent [63, 121].
In a meta-analysis of randomized, controlled treatment trials for OCD, cognitive behavioral therapy (CBT) was found to have a large effect size of 1.45, while pharmacotherapy was associated with a more modest, but still significant, effect size of 0.48 [169]. As such, first line treatment for OCD is always CBT with an emphasis on exposure-response prevention [45, 47]. Pharmacotherapy is often administered in conjunction with psychotherapy, and includes the SSRIs fluoxetine, fluvoxamine, paroxetine, and sertraline, the non-selective serotonin reuptake inhibitor, clomipramine, and as second-line drug therapy, atypical antipsychotics [70, 96]. The effect size of pharmacotherapy, although modest, has been found to be significantly higher than placebo, and response rates, defined as at least a 25 % reduction in YBOCS scores, range from 42 % to 53 % for the SSRIs used in OCD treatment [47, 96]. Thus, since approximately 50 % of patients with OCD do not respond to accepted pharmacologic treatments, more aggressive therapies for OCD are clearly needed.
Stereotactic ablation has been applied for the treatment of OCD in both the pediatric and adult population. Procedures have included anterior capsulotomy, cingulotomy, frontal leucotomy, and subcaudate tractotomy [87]. There have been no controlled trials. According several case reports and to a 2010 review of stereotactic psychosurgery in adults, anterior capsulotomy was, in general, the most effective of the procedures, with cingulotomy second [67, 71, 87, 88]. The use of the anterior capsule as a target for ablation treatment stems from both structural and functional imaging demonstrating its putative involvement in OCD pathophysiology [62]. The data on successful anterior capsulotomies in the pediatric population are limited to single case reports. In one of these, anterior capsulotomy abolished all obsessions and compulsions in an 18-year-old with 8-year history of OCD [29]. Although much less evidence is available regarding the potential for neurosurgical intervention for treatment of aggressive behavioral disorders, the role of stereotactic amygdalotomy is under investigation in some centers [113].
As with many applications of ablative neurosurgery, the benefits of DBS in OCD as a reversible, adjustable, and safer alternative have become attractive. The use of DBS for the treatment of OCD has been reviewed elsewhere, and its application to the pediatric population has been limited [62, 105]. DBS has been applied to the treatment of OCD in adults and received a humanitarian device exemption from the FDA in 2009 for the treatment of OCD [105]. Neuroanatomical targets have included the anterior capsule and the NAc [46, 49, 52, 53, 59, 116], the STN [93], and the inferior thalamic peduncle (ITP) [68]. Improvement of symptoms after implanting DBS ranges from 38 % (YBOCS score at follow-up) [46] to complete remission [44, 94] depending on the anatomic target and patient population.
A four-center open trial of VC/VS-DBS for OCD reported significant reduction in symptoms along with functional improvements in over 60 % of patients in the trial [52]. An encouraging outcome of the trial was the improvement in results as the study progressed and which may have been due to increased experience with targeting, patient selection, and post-surgical management. Target selection is still under investigation. The rationale of targeting the NAc in DBS for OCD is the implication of reward-system dysfunction in OCD. The results of a functional imaging study assessing NAc activity in OCD patients suggested that patients with OCD may not be able to make beneficial choices because of altered NAc activity during reward anticipation [39]. Additionally, bilateral stimulation of the NAc in a rat model has exhibited a reduction in the firing rate of the orbitofrontal cortex, a region where hyperactivity has been implicated in the pathogenesis of OCD [22, 102]. This involvement of the reward system in obsessive behavior, along with the results of animal studies, has motivated the exploration of NAc-DBS for OCD. Results of small uncontrolled studies of bilateral NAc-DBS for OCD have shown response (defined as a Y-BOCS decrease of 35 % or more) rates ranging from 50 % to 100 % [13, 33, 46, 153]. In a 10-month, double-blind study of STN-DBS for OCD, stimulation was shown to confer a significant reduction in Y-BOCS scores and a significant increase in Global Assessment of Functioning scale when compared to sham stimulation [93].
Despite some promising evidence, the use of DBS to treat OCD, even in an adult population, is still in its infancy. Application of DBS to the pediatric population has not been widely reported since many children remit spontaneously as they grow up. Furthermore, the combination of cognitive behavioral therapy and pharmacotherapy for OCD achieves approximately a 50 % remission rate [125], thereby setting a high standard for comparison with other, more innovative and invasive treatments. Therefore, DBS could play a role as an alternative therapy in carefully selected adults and even children who are refractory to the best medical and psychological treatments up [10, 151].
Deep brain stimulation for treatment of pediatric obesity
Obesity
With over 17 % of American children overweight, and an additional 16 % at risk for becoming overweight, pediatric obesity is a significant public health problem [119]. Moreover, obesity in childhood is associated with a multitude of comorbidities, including type 2 diabetes, heart disease, and an overall increased all-cause mortality [114]. A landmark article in 2005 put the effects of obesity in perspective: because of the obesity epidemic in the USA, the life expectancy of Americans may for the first time decrease in the twenty-first century [120]. In response to this epidemic and to the ineffectiveness of lifestyle changes and other conservative measures, bariatric surgery has become an attractive option for the treatment of adolescent obesity [20, 160]. The criteria for treatment with bariatric surgery are roughly the same for adolescents as for adults: BMI >35 with a serious comorbidity, or a BMI >40 with only mild comorbidities [129]. In adolescents, Roux-en-y gastric bypass has exhibited a mean 35 % reduction in BMI and almost complete resolution of complications of obesity, such as hypertension and sleep apnea [20]. Despite the benefits of bariatric surgery in this population, peri- and post-operative complications have been reported, and depending on the specific procedure, the complication rate may outweigh possible benefits, particularly for laparoscopic gastric bands [127]. Gastric banding was associated with a high revision rate of 33 % in adolescents in one study [117]. Nutritional deficiencies especially after malabsorptive procedures such as gastric bypass are concerning [11]. These nutritional problems can be prevented with strict compliance and treatment with vitamins. However, the long-term effects of this are unknown in pediatric subjects.
DBS for the treatment of obesity has been explored as an alternative to bariatric surgery. Targets under investigation have included nuclei of the lateral and ventromedial hypothalamus, as well as the NAc [58, 171]. Exploration of these targets has been motivated by findings of changes in functional activity in the hypothalamus and the ventral striatum (where the NAc is located) in obese patients when compared to lean subjects [118, 164]. A detailed discussion of these target choices has been published elsewhere [58]. While the rationale for targeting hypothalamic regions is based on hypothalamic involvement in homeostasis, feeding behavior, and energy expenditure, the rationale for targeting the NAc is based on the reinforcing properties of high-calorie food [58, 154].
Deep brain stimulation for the treatment of epilepsy
Epilepsy
Epilepsy, defined as two or more unprovoked seizures more than 24 h apart in a child over 1 month of age [2], affects about 1 % of all children up to age 16, with children under the age of 1 at the highest risk [145]. Children with developmental disabilities like cerebral palsy, autism, and mental retardation are at a much higher risk for developing epilepsy [14, 34, 50, 76, 161]. Of children that develop epilepsy, about half will have persistent, lifelong illness [146]. The seizures associated with epilepsy, if not controlled, impact negatively on quality of life, employment, martial relationships, and socioeconomic status [145]. Patients with epilepsy report significant concern regarding their independence, ability to drive, and maintain employment [48]. Current treatment modalities for epilepsy in adults include pharmacotherapy with anti-epileptic drugs (AEDs), surgical resection of a seizure-producing brain region, vagal nerve stimulation (VNS), and DBS. AEDs function to decrease neuronal excitability by increasing GABAergic neurotransmission, decreasing glutamatergic neurotransmission, and modulating ion channel behavior and signaling pathways [69, 133]. Unfortunately, while these drugs offer relief to many patients with epilepsy, up to a third of patients undergoing AED treatment will continue having seizures, and for many patients who do remit, achieving remission can take more than 10 years [146]. Even if AEDs effectively suppress all seizure activity, most cause adverse effects, including cognitive impairment, loss of bone density, gum hyperplasia, risk of fetal maldevelopment during pregnancy, and disruption of sleep architecture, among other problems [72].
In patients whose epilepsy is refractory to pharmacotherapy, surgical procedures to resect or disconnect regions of the brain implicated in seizure production are established forms of therapy. Commonly resected regions include the anteromedial temporal lobe and focal regions of the neocortex; disconnection procedures include corpus callosotomy and multiple subpial hemispherectomy [149]. In a large multicenter study of epilepsy surgery, resection procedures were associated with a 75 % remission rate within a year and an increase in overall quality of life [150]. A meta-analysis of epilepsy surgery found that resective surgeries effect a 27–66 % rate of seizure remission, while callosotomies resulted in only a 35 % seizure-free rate [155]. Unfortunately, many refractory epilepsy patients are not surgical candidates and these procedures are associated with a risk of permanent neurologic deficits or death in nearly 4 % of cases [2]. VNS was approved as an adjunct to pharmacotherapy for adults and adolescents age 12 and over with refractory partial onset seizures [106]. The procedure is associated with up to a 50 % reduction in seizure frequency [3], but many patients will not be seizure free.
Because of the ineffectiveness of many of the treatment options currently available, DBS has been investigated as a treatment option for epilepsy [57, 86]. The Papez neural circuit has been described as a route that links hippocampal output via the fornix and mammillary nuclei to the anterior thalamic nucleus. Projections from the anterior thalamic nucleus then travel through the cingulum bundle to the parahippocampal cortex and complete the circuit by returning to the hippocampus. Animal studies have supported the role of this circuit in seizure occurrence [107–109]. Alterations in the Papez circuit have been observed in multiple forms of epilepsy, and its components have become the targets of investigation of DBS for epilepsy, including hippocampus, anterior thalamic nucleus, and mammillary bodies in the Papez circuit, as well as the centromedian nucleus of the thalamus, STN, caudate nucleus, and cerebellum [12, 16, 25, 27, 28, 41, 89, 163, 165, 167, 168, 173].
DBS of the anterior nucleus of the thalamus (ANT) has been the most widely investigated target. A recent multi-center, randomized, controlled clinical trial of DBS of the anterior thalamic nucleus in adults with medically refractory epilepsy (SANTE) showed a significant 29 % greater reduction in a group stimulated than in a control group with stimulation turned off, while over 12 % of patients became seizure free for at least 6 months [40]. Adverse events from the stimulator implant included implant site parasthesias, pain, and infection; five deaths were reported in the study—none was found to be device related. Although the low rate of remission in this study was disappointing, these patients had failed medical treatment with at least three AEDs and were completely disabled from their illness.
While such results are promising, they are not readily generalizable to a pediatric population. Aside from a few small studies in which an adolescent was included, no data have been published on the use of DBS to treat epilepsy in children. A slight consensus favors ANT as the preferred anatomic target, but other targets need to be explored.
Discussion
Published information covered in this review of the uses of DBS in treating neurologic disorders in children shows promise across a broad clinical spectrum. Medically intractable and severe dystonia is now routinely treated with DBS, and newer applications of DBS in the pediatric population is sure to expand in the near future as evidence from empirical observation and clinical trials I accumulates. A case can be made for early surgical intervention in progressive dystonia as a way of preventing long-term musculoskeletal deformities and functional disability [103]. Furthermore, appropriately early intervention in levodopa responsive juvenile PD is a legitimate therapeutic option to enhance quality of life in young patients facing an uncertain future. However, more evidence is required before DBS can be widely recommended in treating this rare disorder.
Clinical trials of DBS in patients with primary dystonia, especially those with the DYT1 mutation, have been generally positive and have strengthened the rationale for considering DBS when medical therapy is unsatisfactory. Safety is always an issue with surgical intervention, but complication rates have been lowered acceptably with steady advances in surgical technology and the use of sophisticated computerized devices for target identification. With information from such trials, the full scope of outcome and safety data can be weighed by clinicians debating the use of DBS for pediatric dystonia. The relief of symptoms and potential prevention of irreversible motor impairment have made dystonia the most accepted application for DBS in the pediatric population.
OCD and TS, unlike primary progressive dystonia, are associated with a fairly high remission rate by early adulthood [84, 151]. Arguments for the use of DBS in children for diseases that will eventually decrease in severity will need to include a rationale for possible persistence and for marked disability during symptomatic periods. For example, severe OCD or TS (or TS with comorbid obsessive-compulsive symptoms) can cause significant disability as children go through school-age years particularly due to social isolation [151]. If medical therapies are ineffective, it is probable that uncontrolled OCD and TS may markedly hinder a child’s social and educational development, irrespective of the possibility of remission late in childhood. DBS offers the possibility of significant relief during a critical transitional time in the life of an affected child, and thus clinical trials should be considered to investigate the role of DBS in treating severely symptomatic TS. Future research on the use of DBS for neuropsychiatric disease in children will need to include the development of reliable methods of assessing disability and the probability of persistent disease.
Neither epilepsy nor obesity are indications for which DBS has been well established in the adult population, and thus they are not yet ready for application in the pediatric population. Despite the fact that randomized clinical trial data have been published for the use of DBS to treat epilepsy, its value is currently unclear. The results of the SANTE trial of using ANT-DBS for epilepsy in adults showed that the treatment is safe, but that it does not result in full remission in 88 % of patients. Challenges that this DBS application faces are wide and range from the choice of an appropriate target (of which there are many proposed) to the types of epilepsy syndromes best treated with DBS. The value of DBS for treating obesity in adults and children is likewise speculative at this time. With a paucity of human data for this application and the lack of consensus on a target for stimulation, research at the level of adult treatment and animal models will need to be performed before pediatric application is pursued.
In addition to the concerns about the effectiveness and safety of DBS in children, the battery life of the internal pulse generator (IPG) portion of a DBS device is of considerable concern for this young population. In a recent analysis, the battery life of a non-rechargeable IPG in treating PD in adults can vary from 9 to 44 months, depending on the neurologic condition, settings, type of device, intensity of use, and number of previous IPG replacements the patient has had [55]. A battery change involves a brief surgical procedure to change the replace the IPG. The young age of pediatric patients would require a considerable number of such battery changes over a lifetime, and as such, these patients will be exposed to a higher risk of surgical complications than adults. As the use of DBS in the pediatric population expands, minimizing exposure to surgery will be important as the IPGs of these patients are maintained. The development of transdermally rechargeable IPGs will be an important step forward for patients who stand to endure many battery changes over the course of treatment of their chronic disease.
References
(2000) Diagnostic and statistical manual of mental disorders (DSM-IV-TR). American Psychiatric Association
(1997 Feb) A global survey on epilepsy surgery, 1980–1990: a report by the commission on neurosurgery of epilepsy, the international league against epilepsy. Epilepsia 38(2):249–55
(1995 Feb) A randomized controlled trial of chronic vagus nerve stimulation for treatment of medically intractable seizures. the vagus nerve stimulation study group. Neurology 45(2):224–30
ICD-10 version: 2010 [Internet]: World Health Organization. Available from: http://apps.who.int/classifications/icd10/browse/2010/en#/F42
Ackermans L, Duits A, van der Linden C, Tijssen M, Schruers K, Temel Y et al (2011) Double-blind clinical trial of thalamic stimulation in patients with Tourette syndrome. Brain 134(Pt 3):832–844
Albright AL, Ferson SS (2009) Intraventricular baclofen for dystonia: techniques and outcomes. Clinical article. J Neurosurg Pediatr 3(1):11–14
Albright AL, Ferson SS (2006) Intrathecal baclofen therapy in children. Neurosurg Focus 21(2):e3
Albright AL, Barry MJ, Shafton DH, Ferson SS (2001) Intrathecal baclofen for generalized dystonia. Dev Med Child Neurol 43(10):652–657
Alcindor D, Oh MY, Baser S, Angle C, Cheng BC, Whiting D (2010) Stimulation of the globus pallidus internus in a patient with DYT1-positive primary generalized dystonia: a 10-year follow-up. Neurosurg Focus 29(2):E16
Allsopp M, Verduyn C (1989) A follow-up of adolescents with obsessive-compulsive disorder. Br J Psychiatry 154:829–834
Alvarez-Leite JI (2004) Nutrient deficiencies secondary to bariatric surgery. Curr Opin Clin Nutr Metab Care 7(5):569–575
Andrade DM, Zumsteg D, Hamani C, Hodaie M, Sarkissian S, Lozano AM et al (2006) Long-term follow-up of patients with thalamic deep brain stimulation for epilepsy. Neurology 66(3):1571–1573
Aouizerate B, Cuny E, Martin-Guehl C, Guehl D, Amieva H, Benazzouz A et al (2004) Deep brain stimulation of the ventral caudate nucleus in the treatment of obsessive-compulsive disorder and major depression. Case report. J Neurosurg 101(4):682–686
Arya R, Kabra M, Gulati S (2011) Epilepsy in children with Down syndrome. Epileptic Disord 13(1):1–7
Babel T, Warnke P, Ostertag C (2001) Immediate and long term outcome after infrathalamic and thalamic lesioning for intractable Tourette’s syndrome. J Neurol Neurosurg Psychiatry 70:666–671
Benabid AL, Koudsie A, Benazzouz A, Vercueil L, Fraix V, Chabardes S et al (2001) Deep brain stimulation of the corpus luysi (subthalamic nucleus) and other targets in Parkinson’s disease. Extension to new indications such as dystonia and epilepsy. J Neurol 248(Suppl 3):III37–III47
Benazzouz A, Piallat B, Pollak P, Benabid AL (1995) Responses of substantia nigra pars reticulata and globus pallidus complex to high frequency stimulation of the subthalamic nucleus in rats: electrophysiological data. Neurosci Lett 189(2):77–80
Bhatia KP, Marsden CD (1994) The behavioural and motor consequences of focal lesions of the basal ganglia in man. Brain 117(4):859–876
Bloch MH, Leckman JF (2009) Clinical course of Tourette syndrome. J Psychosom Res 67(6):497–501
Bondada S, Jen HC, Deugarte DA (2011) Outcomes of bariatric surgery in adolescents. Curr Opin Pediatr 23(5):552–556
Borggraefe I, Mehrkens JH, Telegravciska M, Berweck S, Botzel K, Heinen F (2010) Bilateral pallidal stimulation in children and adolescents with primary generalized dystonia—report of six patients and literature-based analysis of predictive outcomes variables. Brain Dev 32(3):223–228
Breiter HC, Rauch SL (1996) Functional MRI and the study of OCD: from symptom provocation to cognitive-behavioral probes of cortico-striatal systems and the amygdala. NeuroImage 4(3 Pt 3):S127–S138
Burdick A, Foote KD, Goodman W, Ward HE, Ricciuti N, Murphy T et al (2010) Lack of benefit of accumbens/capsular deep brain stimulation in a patient with both tics and obsessive-compulsive disorder. Neurocase 16(4):321–330
Cavanna AE, Eddy CM, Mitchell R, Pall H, Mitchell I, Zrinzo L et al (2011) An approach to deep brain stimulation for severe treatment-refractory Tourette syndrome: the UK perspective. Br J Neurosurg 25(1):38–44
Chabardes S, Kahane P, Minotti L, Koudsie A, Hirsch E, Benabid AL (2002) Deep brain stimulation in epilepsy with particular reference to the subthalamic nucleus. Epileptic Disord 4(Suppl 3):S83–S93
Chiu CH, Lo YC, Tang HS, Liu IC, Chiang WY, Yeh FC et al (2011) White matter abnormalities of fronto-striato-thalamic circuitry in obsessive-compulsive disorder: a study using diffusion spectrum imaging tractography. Psychiatry Res 192(3):176–182
Chkhenkeli SA, Sramka M, Lortkipanidze GS, Rakviashvili TN, Bregvadze ES, Magalashvili GE et al (2004) Electrophysiological effects and clinical results of direct brain stimulation for intractable epilepsy. Clin Neurol Neurosurg 106(4):318–329
Chkhenkeli SA, Chkhenkeli IS (1997) Effects of therapeutic stimulation of nucleus caudatus on epileptic electrical activity of brain in patients with intractable epilepsy. Stereotact Funct Neurosurg 69(1–4 Pt 2):221–224
Christensen DD, Laitinen LV, Schmidt LJ, Hariz MI (2002) Anterior capsulotomy for treatment of refractory obsessive-compulsive disorder: results in a young and an old patient. Stereotact Funct Neurosurg 79(3–4):234–244
Coubes P, Roubertie A, Vayssiere N, Hemm S, Echenne B (2000) Treatment of DYT1-generalised dystonia by stimulation of the internal globus pallidus. Lancet 355(9222):2220–2221
Defazio G, Abbruzzese G, Livrea P, Berardelli A (2004) Epidemiology of primary dystonia. Lancet Neurol 3(11):673–678
Deniau JM, Degos B, Bosch C, Maurice N (2010) Deep brain stimulation mechanisms: beyond the concept of local functional inhibition. Eur J Neurosci 32(7):1080–1091
Denys D, Mantione M, Figee M, van den Munckhof P, Koerselman F, Westenberg H et al (2010) Deep brain stimulation of the nucleus accumbens for treatment-refractory obsessive-compulsive disorder. Arch Gen Psychiatry 67(10):1061–1068
Depositario-Cabacar DF, Zelleke TG (2010) Treatment of epilepsy in children with developmental disabilities. Dev Disabil Res Rev 16(3):239–247
Dion Y, Annable L, Sandor P, Chouinard G (2002) Risperidone in the treatment of Tourette syndrome: a double-blind, placebo-controlled trial. J Clin Psychopharmacol 22(1):31–39
Dueck A, Wolters A, Wunsch K, Bohne-Suraj S, Mueller JU, Haessler F et al (2009) Deep brain stimulation of globus pallidus internus in a 16-year-old boy with severe Tourette syndrome and mental retardation. Neuropediatrics 40(5):239–242
Eltahawy HA, Saint-Cyr J, Giladi N, Lang AE, Lozano A (2004) Primary dystonia is more responsive than secondary dystonia to pallidal interventions: outcome after pallidotomy or pallidal deep brain stimulation. Neurosurgery 54(3):613–621
Fahn S (2011) Classification of movement disorders. Mov Disord 26(6):947–957
Figee M, Vink M, de Geus F, Vulink N, Veltman DJ, Westenberg H et al (2011) Dysfunctional reward circuitry in obsessive-compulsive disorder. Biol Psychiatry 69(9):867–874
Fisher R, Salanova V, Witt T, Worth R, Henry T, Gross R et al (2010) Electrical stimulation of the anterior nucleus of thalamus for treatment of refractory epilepsy. Epilepsia 51(5):899–908
Fisher RS, Uematsu S, Krauss GL, Cysyk BJ, McPherson R, Lesser RP et al (1992) Placebo-controlled pilot study of centromedian thalamic stimulation in treatment of intractable seizures. Epilepsia 33(5):841–851
Focquaert F (2011) Pediatric deep brain stimulation: a cautionary approach. Front Integr Neurosci 5:9
Follett KA, Weaver FM, Stern M, Hur K, Harris CL, Luo P et al (2010) Pallidal versus subthalamic deep-brain stimulation for Parkinson’s disease. N Engl J Med 362(22):2077–2091
Fontaine D, Mattei V, Borg M, von Langsdorff D, Magnie MN, Chanalet S et al (2004) Effect of subthalamic nucleus stimulation on obsessive-compulsive disorder in a patient with Parkinson disease. Case report. J Neurosurg 100(6):1084–1086
Franklin ME, Foa EB (2011) Treatment of obsessive compulsive disorder. Annu Rev Clin Psychol 7:229–243
Franzini A, Messina G, Gambini O, Muffatti R, Scarone S, Cordella R et al (2010) Deep-brain stimulation of the nucleus accumbens in obsessive compulsive disorder: clinical, surgical and electrophysiological considerations in two consecutive patients. Neurol Sci 31(3):353–359
Geller DA, Biederman J, Stewart SE, Mullin B, Martin A, Spencer T et al (2003) Which SSRI? A meta-analysis of pharmacotherapy trials in pediatric obsessive-compulsive disorder. Am J Psychiatry 160(11):1919–1928
Gilliam F, Kuzniecky R, Faught E, Black L, Carpenter G, Schrodt R (1997) Patient-validated content of epilepsy-specific quality-of-life measurement. Epilepsia 38(2):233–236
Goodman WK, Foote KD, Greenberg BD, Ricciuti N, Bauer R, Ward H et al (2010) Deep brain stimulation for intractable obsessive compulsive disorder: pilot study using a blinded, staggered-onset design. Biol Psychiatry 67(6):535–542
Goulden KJ, Shinnar S, Koller H, Katz M, Richardson SA (1991) Epilepsy in children with mental retardation: a cohort study. Epilepsia 32(5):690–697
Gradinaru V, Mogri M, Thompson KR, Henderson JM, Deisseroth K (2009) Optical deconstruction of parkinsonian neural circuitry. Science 324(5925):354–359
Greenberg BD, Gabriels LA, Malone DA Jr, Rezai AR, Friehs GM, Okun MS et al (2010) Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: worldwide experience. Mol Psychiatry 15(1):64–79
Greenberg BD, Malone DA, Friehs GM, Rezai AR, Kubu CS, Malloy PF et al (2006) Three-year outcomes in deep brain stimulation for highly resistant obsessive-compulsive disorder. Neuropsychopharmacology 31(11):2384–2393
Gross RE (2008) What happened to posteroventral pallidotomy for Parkinson’s disease and dystonia? Neurotherapeutics 5(2):281–293
Halpern CH, McGill KR, Baltuch GH, Jaggi JL (2011) Longevity analysis of currently available deep brain stimulation devices. Stereotact Funct Neurosurg 89(1):1–5
Halpern CH, Rick JH, Danish SF, Grossman M, Baltuch GH (2009) Cognition following bilateral deep brain stimulation surgery of the subthalamic nucleus for Parkinson’s disease. Int J Geriatr Psychiatry 24(5):443–451
Halpern CH, Samadani U, Litt B, Jaggi JL, Baltuch GH (2008) Deep brain stimulation for epilepsy. Neurotherapeutics 5(1):59–67
Halpern CH, Wolf JA, Bale TL, Stunkard AJ, Danish SF, Grossman M et al (2008) Deep brain stimulation in the treatment of obesity. J Neurosurg 109(4):625–634
Haq IU, Foote KD, Goodman WK, Ricciuti N, Ward H, Sudhyadhom A et al (2010) A case of mania following deep brain stimulation for obsessive compulsive disorder. Stereotact Funct Neurosurg 88(5):322–328
Haridas AM, Tagliati MM, Osborn IM, Isaias IM, Gologorsky YM, Bressman SBM et al (2011) Pallidal deep brain stimulation for primary dystonia in children. Neurosurgery 68(3):738–743
Harrison BJ, Soriano-Mas C, Pujol J, Ortiz H, Lopez-Sola M, Hernandez-Ribas R et al (2009) Altered corticostriatal functional connectivity in obsessive-compulsive disorder. Arch Gen Psychiatry 66(11):1189–1200
Haynes WI, Mallet L (2010) High-frequency stimulation of deep brain structures in obsessive-compulsive disorder: the search for a valid circuit. Eur J Neurosci 32(7):1118–1127
Hu XZ, Lipsky RH, Zhu G, Akhtar LA, Taubman J, Greenberg BD et al (2006) Serotonin transporter promoter gain-of-function genotypes are linked to obsessive-compulsive disorder. Am J Hum Genet 78(5):815–826
Hubble JP, Busenbark KL, Wilkinson S, Penn RD, Lyons K, Koller WC (1996) Deep brain stimulation for essential tremor. Neurology 46(4):1150–1153
Jankovic J (2005) Motor fluctuations and dyskinesias in parkinson’s disease: clinical manifestations. Mov Disord 20(Suppl 11):S11–S16
Jans T, Wewetzer C, Klampfl K, Schulz E, Herpertz-Dahlmann B, Remschmidt H et al (2007) Phenomenology and co-morbidity of childhood onset obsessive compulsive disorder. Z Kinder Jugendpsychiatr Psychother 35(1):41–50
Jenike MA, Baer L, Ballantine T, Martuza RL, Tynes S, Giriunas I et al (1991) Cingulotomy for refractory obsessive-compulsive disorder. A long-term follow-up of 33 patients. Arch Gen Psychiatry 48(6):548–555
Jimenez-Ponce F, Velasco-Campos F, Castro-Farfan G, Nicolini H, Velasco AL, Salin-Pascual R et al (2009) Preliminary study in patients with obsessive-compulsive disorder treated with electrical stimulation in the inferior thalamic peduncle. Neurosurgery 65(6 Suppl):203–209, discussion 209
Johannessen Landmark C, Johannessen SI (2008) Pharmacological management of epilepsy: recent advances and future prospects. Drugs 68(14):1925–1939
Kellner M (2010) Drug treatment of obsessive-compulsive disorder. Dialogues Clin Neurosci 12(2):187–197
Kondziolka D, Flickinger JC, Hudak R (2011) Results following gamma knife radiosurgical anterior capsulotomies for obsessive compulsive disorder. Neurosurgery 68(1):28–32, discussion 23–3
Kothare SV, Kaleyias J (2007) The adverse effects of antiepileptic drugs in children. Expert Opin Drug Saf 6(3):251–265
Krauss JK, Pohle T, Weber S, Ozdoba C, Burgunder JM (1999) Bilateral stimulation of globus pallidus internus for treatment of cervical dystonia. Lancet 354(9181):837–838
Krauss JK, Mohadjer M, Braus DF, Wakhloo AK, Nobbe F, Mundinger F (1992) Dystonia following head trauma: a report of nine patients and review of the literature. Mov Disord 7(3):263–272
Kravitz AV, Freeze BS, Parker PR, Kay K, Thwin MT, Deisseroth K et al (2010) Regulation of parkinsonian motor behaviours by optogenetic control of basal ganglia circuitry. Nature 466(7306):622–626
Kudrjavcev T, Schoenberg BS, Kurland LT, Groover RV (1985) Cerebral palsy: survival rates, associated handicaps, and distribution by clinical subtype (Rochester, MN, 1950–1976). Neurology 35(6):900–903
Kuhn J, Lenartz D, Mai JK, Huff W, Lee SH, Koulousakis A et al (2007) Deep brain stimulation of the nucleus accumbens and the internal capsule in therapeutically refractory Tourette-syndrome. J Neurol 254(7):963–965
Kulisevsky J, Lleo A, Gironell A, Molet J, Pascual-Sedano B, Pares P (2000) Bilateral pallidal stimulation for cervical dystonia: dissociated pain and motor improvement. Neurology 55(11):1754–1755
Kumar R, Dagher A, Hutchison WD, Lang AE, Lozano AM (1999) Globus pallidus deep brain stimulation for generalized dystonia: clinical and PET investigation. Neurology 53(4):871–874
Kupsch A, Benecke R, Muller J, Trottenberg T, Schneider GH, Poewe W et al (2006) Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N Engl J Med 355(19):1978–1990
Kurlan R (2010) Tourette’s syndrome. N Engl J Med 363(8):2332–2338
Kwak C, Dat Vuong K, Jankovic J (2003) Premonitory sensory phenomenon in Tourette’s syndrome. Mov Disord 18(12):1530–1533
Kwak CH, Hanna PA, Jankovic J (2000) Botulinum toxin in the treatment of tics. Arch Neurol 57(8):1190–1193
Leckman JF, Zhang H, Vitale A, Lahnin F, Lynch K, Bondi C et al (1998) Course of tic severity in Tourette syndrome: the first two decades. Pediatrics 102(1):14–19
Lees A (2010) The bare essentials: Parkinson’s disease. Pract Neurol 10(4):240–246
Lega BC, Halpern CH, Jaggi JL, Baltuch GH (2010) Deep brain stimulation in the treatment of refractory epilepsy: update on current data and future directions. Neurobiol Dis 38(3):354–360
Leiphart JW, Valone FH 3rd (2010) Stereotactic lesions for the treatment of psychiatric disorders. J Neurosurg 113(6):1204–1211
Liu K, Zhang H, Liu C, Guan Y, Lang L, Cheng Y et al (2008) Stereotactic treatment of refractory obsessive compulsive disorder by bilateral capsulotomy with 3 years follow-up. J Clin Neurosci 15(6):622–629
Loddenkemper T, Pan A, Neme S, Baker KB, Rezai AR, Dinner DS et al (2001) Deep brain stimulation in epilepsy. J Clin Neurophysiol 18(6):514–532
Lohmann E, Welter ML, Fraix V, Krack P, Lesage S, Laine S et al (2008) Are parkin patients particularly suited for deep-brain stimulation? Mov Disord 23(5):740–743
Lozano AM, Kumar R, Gross RE, Giladi N, Hutchison WD, Dostrovsky JO et al (1997) Globus pallidus internus pallidotomy for generalized dystonia. Mov Disord 12(6):865–870
Lyons MK (2011) Deep brain stimulation: current and future clinical applications. Mayo Clin Proc 86(7):662–672
Mallet L, Polosan M, Jaafari N, Baup N, Welter ML, Fontaine D et al (2008) Subthalamic nucleus stimulation in severe obsessive-compulsive disorder. N Engl J Med 359(20):2121–2134
Mallet L, Mesnage V, Houeto JL, Pelissolo A, Yelnik J, Behar C et al (2002) Compulsions, Parkinson’s disease, and stimulation. Lancet 360(9342):1302–1304
Malone DA Jr (2010) Use of deep brain stimulation in treatment-resistant depression. Cleve Clin J Med 77(Suppl 3):S77–S80
Mancuso E, Faro A, Joshi G, Geller DA (2010) Treatment of pediatric obsessive-compulsive disorder: a review. J Child Adolesc Psychopharmacol 20(4):299–308
Marks WA, Honeycutt J, Acosta F, Reed M, Bailey L, Pomykal A, et al. (2011) Dystonia due to cerebral palsy responds to deep brain stimulation of the globus pallidus internus. Movement Disorders 26(9):1748–1751
Marks WA, Honeycutt J, Acosta F, Reed M (2009) Deep brain stimulation for pediatric movement disorders. Semin Pediatr Neurol 16(2):90–98
Marras C, Andrews D, Sime E, Lang AE (2001) Botulinum toxin for simple motor tics: a randomized, double-blind, controlled clinical trial. Neurology 56(5):605–610
Martínez-Fernández R, Zrinzo L, Aviles-Olmos I, Hariz M, Martinez-Torres I, Joyce E, et al. (2011) Deep brain stimulation for Gilles de la Tourette syndrome: a case series targeting subregions of the globus pallidus internus. Movement Disorders 26(10):1922–1930
Martinez-Torres I, Hariz MI, Zrinzo L, Foltynie T, Limousin P (2009) Improvement of tics after subthalamic nucleus deep brain stimulation. Neurology 72(20):1787–1789
McCracken CB, Grace AA (2007) High-frequency deep brain stimulation of the nucleus accumbens region suppresses neuronal activity and selectively modulates afferent drive in rat orbitofrontal cortex in vivo. J Neurosci 27(46):12601–12610
Mehrkens JH, Borggraefe I, Feddersen B, Heinen F, Botzel K (2010) Early globus pallidus internus stimulation in pediatric patients with generalized primary dystonia: long-term efficacy and safety. J Child Neurol 25(11):1355–1361
Mehrkens JH, Botzel K, Steude U, Zeitler K, Schnitzler A, Sturm V et al (2009) Long-term efficacy and safety of chronic globus pallidus internus stimulation in different types of primary dystonia. Stereotact Funct Neurosurg 87(1):8–17
Mian MK, Campos M, Sheth SA, Eskandar EN (2010) Deep brain stimulation for obsessive-compulsive disorder: past, present, and future. Neurosurg Focus 29(2):E10
Milby AH, Halpern CH, Baltuch GH (2009) Vagus nerve stimulation in the treatment of refractory epilepsy. Neurotherapeutics 6(2):228–237
Mirski MA, Fisher RS (1994) Electrical stimulation of the mammillary nuclei increases seizure threshold to pentylenetetrazol in rats. Epilepsia 35(6):1309–1316
Mirski MA, Ferrendelli JA (1986) Selective metabolic activation of the mammillary bodies and their connections during ethosuximide-induced suppression of pentylenetetrazol seizures. Epilepsia 27(3):194–203
Mirski MA, Ferrendelli JA (1984) Interruption of the mammillothalamic tract prevents seizures in guinea pigs. Science 226(4670):72–74
Misbahuddin A, Warner TT (2001) Dystonia: an update on genetics and treatment. Curr Opin Neurol 14(4):471–475
Moro E, Volkmann J, Konig IR, Winkler S, Hiller A, Hassin-Baer S et al (2008) Bilateral subthalamic stimulation in parkin and PINK1 parkinsonism. Neurology 70(14):1186–1191
Motta F, Stignani C, Antonello CE (2008) Effect of intrathecal baclofen on dystonia in children with cerebral palsy and the use of functional scales. J Pediatr Orthop 28(2):213–217
Mpakopoulou M, Gatos H, Brotis A, Paterakis KN, Fountas KN (2008) Stereotactic amygdalotomy in the management of severe aggressive behavioral disorders. Neurosurg Focus 25(1):E6
Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH (1992) Long-term morbidity and mortality of overweight adolescents. N Engl J Med 327(19):1350–1355
Neuner I, Podoll K, Lenartz D, Sturm V, Schneider F (2009) Deep brain stimulation in the nucleus accumbens for intractable Tourette’s syndrome: follow-up report of 36 months. Biol Psychiatry 65(4):e5–e6
Nuttin BJ, Gabriels LA, Cosyns PR, Meyerson BA, Andreewitch S, Sunaert SG et al (2003) Long-term electrical capsular stimulation in patients with obsessive-compulsive disorder. Neurosurgery 52(6):1263–1272, discussion 1272–4
O’Brien PE, Sawyer SM, Laurie C, Brown WA, Skinner S, Veit F et al (2010) Laparoscopic adjustable gastric banding in severely obese adolescents: a randomized trial. JAMA 303(6):519–526
O’Doherty JP, Deichmann R, Critchley HD, Dolan RJ (2002) Neural responses during anticipation of a primary taste reward. Neuron 33(5):815–826
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM (2006) Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 295(13):1549–1555
Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J et al (2005) A potential decline in life expectancy in the United States in the 21st century. N Engl J Med 352(11):1138–1145
Ozaki N, Goldman D, Kaye WH, Plotnicov K, Greenberg BD, Lappalainen J et al (2003) Serotonin transporter missense mutation associated with a complex neuropsychiatric phenotype. Mol Psychiatry 8(11):933–936
Pahwa R, Lyons KE, Wilkinson SB, Tröster AI, Overman J, Kieltyka J et al (2001) Comparison of thalamotomy to deep brain stimulation of the thalamus in essential tremor. Mov Disord 16(1):140–143
Palminteri S, Lebreton M, Worbe Y, Hartmann A, Lehericy S, Vidailhet M, et al. (2011 Jul 3) Dopamine-dependent reinforcement of motor skill learning: evidence from Gilles de la Tourette syndrome. Brain 134(Pt 8):2287–2301
Pauls DL (2010) The genetics of obsessive-compulsive disorder: a review. Dialogues Clin Neurosci 12(2):149–163
Pediatric OCD Treatment Study (POTS) Team (2004) Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: the pediatric OCD treatment study (POTS) randomized controlled trial. JAMA 292(16):1969–1976
Pin TW, McCartney L, Lewis J, Waugh MC. (2011 Jun 3) Use of intrathecal baclofen therapy in ambulant children and adolescents with spasticity and dystonia of cerebral origin: a systematic review. Dev Med Child Neurol 53(11):1065
Pisapia JM, Halpern CH, Williams NN, Wadden TA, Baltuch GH, Stein SC (2010) Deep brain stimulation compared with bariatric surgery for the treatment of morbid obesity: a decision analysis study. Neurosurg Focus 29(2):E15
Porta M, Brambilla A, Cavanna AE, Servello D, Sassi M, Rickards H et al (2009) Thalamic deep brain stimulation for treatment-refractory Tourette syndrome: two-year outcome. Neurology 73(17):1375–1380
Pratt JS, Lenders CM, Dionne EA, Hoppin AG, Hsu GL, Inge TH et al (2009) Best practice updates for pediatric/adolescent weight loss surgery. Obesity (Silver Spring) 17(5):901–910
Pringsheim T, Lam D, Ching H, Patten S (2011) Metabolic and neurological complications of second-generation antipsychotic use in children: a systematic review and meta-analysis of randomized controlled trials. Drug Saf 34(8):651–668
Quinn N, Critchley P, Marsden CD (1987) Young onset Parkinson’s disease. Mov Disord 2(2):73–91
Robertson MM (2008) The prevalence and epidemiology of Gilles de la Tourette syndrome: Part 1: the epidemiological and prevalence studies. J Psychosom Res 65(5):461–472
Rogawski MA, Loscher W (2004) The neurobiology of antiepileptic drugs. Nat Rev Neurosci 5(7):553–564
Ross M, Moldofsky H (1978) A comparison of pimozide and haloperidol in the treatment of Gilles de la Tourette’s syndrome. Am J Psychiatry 135(5):585–587
Roubertie A, Echenne B, Cif L, Vayssiere N, Hemm S, Coubes P (2000) Treatment of early-onset dystonia: update and a new perspective. Childs Nerv Syst 16(6):334–340
Sakai Y, Narumoto J, Nishida S, Nakamae T, Yamada K, Nishimura T et al (2011) Corticostriatal functional connectivity in non-medicated patients with obsessive-compulsive disorder. Eur Psychiatry 26(7):463–469
Saxena S, Rauch SL (2000) Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin N Am 23(3):563–586
Scahill L, Erenberg G, Berlin CM Jr, Budman C, Coffey BJ, Jankovic J et al (2006) Contemporary assessment and pharmacotherapy of Tourette syndrome. NeuroRx 3(2):192–206
Scahill L, Leckman JF, Schultz RT, Katsovich L, Peterson BS (2003) A placebo-controlled trial of risperidone in Tourette syndrome. Neurology 60(7):1130–1135
Schrag A, Schott JM (2006) Epidemiological, clinical, and genetic characteristics of early-onset parkinsonism. Lancet Neurol 5(4):355–363
Schrag A, Ben-Shlomo Y, Brown R, Marsden CD, Quinn N (1998) Young-onset Parkinson’s disease revisited—clinical features, natural history, and mortality. Mov Disord 13(6):885–894
Servello D, Porta M, Sassi M, Brambilla A, Robertson MM (2008) Deep brain stimulation in 18 patients with severe Gilles de la Tourette syndrome refractory to treatment: the surgery and stimulation. J Neurol Neurosurg Psychiatry 79(2):136–142
Shahed J, Poysky J, Kenney C, Simpson R, Jankovic J (2007) GPi deep brain stimulation for Tourette syndrome improves tics and psychiatric comorbidities. Neurology 68(2):159–160
Shapiro AK, Shapiro E (1984) Controlled study of pimozide vs. placebo in Tourette’s syndrome. J Am Acad Child Psychiatry 23(2):161–173
Shinnar S, Pellock JM (2002) Update on the epidemiology and prognosis of pediatric epilepsy. J Child Neurol 17(Suppl 1):S4–S17
Sillanpaa M, Schmidt D (2006) Natural history of treated childhood-onset epilepsy: prospective, long-term population-based study. Brain 129(Pt 3):617–624
Simpson DM, Blitzer A, Brashear A, Comella C, Dubinsky R, Hallett M et al (2008) Assessment: Botulinum neurotoxin for the treatment of movement disorders (an evidence-based review): report of the therapeutics and technology assessment subcommittee of the American Academy of Neurology. Neurology 70(19):1699–1706
Skoog G, Skoog I (1999) A 40-year follow-up of patients with obsessive-compulsive disorder [see comments]. Arch Gen Psychiatry 56(2):121–127
Spencer S, Huh L (2008) Outcomes of epilepsy surgery in adults and children. Lancet Neurol 7(6):525–537
Spencer SS, Berg AT, Vickrey BG, Sperling MR, Bazil CW, Shinnar S et al (2003) Initial outcomes in the multicenter study of epilepsy surgery. Neurology 61(12):1680–1685
Stewart SE, Geller DA, Jenike M, Pauls D, Shaw D, Mullin B et al (2004) Long-term outcome of pediatric obsessive-compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiatr Scand 110(1):4–13
Stillman A, Ercan-Sencicek AG, State MW (1993) Tourette disorder overview. In: Pagon RA, Bird TD, Dolan CR, Stephens K, Adam MP (eds) Gene reviewsTM [Internet]. University of Washington, Seattle, Seattle (WA). Available from: http://proxy.library.upenn.edu:2082/books/NBK21138/
Sturm V, Lenartz D, Koulousakis A, Treuer H, Herholz K, Klein JC et al (2003) The nucleus accumbens: a target for deep brain stimulation in obsessive-compulsive- and anxiety-disorders. J Chem Neuroanat 26(4):293–299
Teegarden SL, Bale TL (2007) Decreases in dietary preference produce increased emotionality and risk for dietary relapse. Biol Psychiatry 61(9):1021–1029
Tellez-Zenteno JF, Dhar R, Wiebe S (2005) Long-term seizure outcomes following epilepsy surgery: a systematic review and meta-analysis. Brain 128(Pt 5):1188–1198
Temel Y, Visser-Vandewalle V (2004) Surgery in Tourette syndrome. Mov Disord 19(1):3–14
The Tourette Syndrome Classification Study Group (1993) Definitions and classification of tic disorders. Arch Neurol 50(10):1013–1016
Thomsen TR, Rodnitzky RL (2010) Juvenile parkinsonism: epidemiology, diagnosis and treatment. CNS Drugs 24(6):467–477
Timmermann L, Pauls KA, Wieland K, Jech R, Kurlemann G, Sharma N et al (2010) Dystonia in neurodegeneration with brain iron accumulation: outcome of bilateral pallidal stimulation. Brain 133(Pt 3):701–712
Tsai WS, Inge TH, Burd RS (2007) Bariatric surgery in adolescents: recent national trends in use and in-hospital outcome. Arch Pediatr Adolesc Med 161(3):217–221
Tuchman RF, Rapin I, Shinnar S (1991) Autistic and dysphasic children. II: Epilepsy. Pediatrics 88(6):1219–1225
Valleni-Basile LA, Garrison CZ, Jackson KL, Waller JL, McKeown RE, Addy CL et al (1994) Frequency of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry 33(6):782–791
Van Buren JM, Wood JH, Oakley J, Hambrecht F (1978) Preliminary evaluation of cerebellar stimulation by double-blind stimulation and biological criteria in the treatment of epilepsy. J Neurosurg 48(3):407–416
van de Sande-Lee S, Pereira FR, Cintra DE, Fernandes PT, Cardoso AR, Garlipp CR et al (2011) Partial reversibility of hypothalamic dysfunction and changes in brain activity after body mass reduction in obese subjects. Diabetes 60(6):1699–1704
Velasco AL, Velasco F, Jimenez F, Velasco M, Castro G, Carrillo-Ruiz JD et al (2006) Neuromodulation of the centromedian thalamic nuclei in the treatment of generalized seizures and the improvement of the quality of life in patients with Lennox–Gastaut syndrome. Epilepsia 47(7):1203–1212
Vidailhet M, Yelnik J, Lagrange C, Fraix V, Grabli D, Thobois S et al (2009) Bilateral pallidal deep brain stimulation for the treatment of patients with dystonia–choreoathetosis cerebral palsy: a prospective pilot study. Lancet Neurol 8(8):709–717
Vonck K, Boon P, Claeys P, Dedeurwaerdere S, Achten R, Van Roost D (2005) Long-term deep brain stimulation for refractory temporal lobe epilepsy. Epilepsia 46(Suppl 5):98–99
Vonck K, Boon P, Achten E, De Reuck J, Caemaert J (2002) Long-term amygdalohippocampal stimulation for refractory temporal lobe epilepsy. Ann Neurol 52(5):556–565
Watson HJ, Rees CS (2008) Meta-analysis of randomized, controlled treatment trials for pediatric obsessive-compulsive disorder. J Child Psychol Psychiatry 49(5):489–498
Whiteside SP, Port JD, Abramowitz JS (2004) A meta-analysis of functional neuroimaging in obsessive-compulsive disorder. Psychiatry Res 132(1):69–79
Wilent WB, Oh MY, Buetefisch C, Bailes JE, Cantella D, Angle C et al (2011) Mapping of microstimulation evoked responses and unit activity patterns in the lateral hypothalamic area recorded in awake humans. J Neurosurg 115(2):295–300
Wirdefeldt K, Adami HO, Cole P, Trichopoulos D, Mandel J (2011) Epidemiology and etiology of Parkinson’s disease: a review of the evidence. Eur J Epidemiol 26(Suppl 1):S1–S58
Wright GD, McLellan DL, Brice JG (1984) A double-blind trial of chronic cerebellar stimulation in twelve patients with severe epilepsy. J Neurol Neurosurg Psychiatry 47(8):769–774
Zabek M, Sobstyl M, Koziara H, Dzierzecki S (2008) Deep brain stimulation of the right nucleus accumbens in a patient with Tourette syndrome. Case report. Neurol Neurochir Pol 42(6):554–559
Zhang F, Wang LP, Boyden ES, Deisseroth K (2006) Channelrhodopsin-2 and optical control of excitable cells. Nat Methods 3(10):785–792
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DiFrancesco, M.F., Halpern, C.H., Hurtig, H.H. et al. Pediatric indications for deep brain stimulation. Childs Nerv Syst 28, 1701–1714 (2012). https://doi.org/10.1007/s00381-012-1861-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1861-2