Abstract
Medical management is the standard treatment of chronic type B aortic dissection (CTBAD). However, the roles of open surgical repair (OSR) and thoracic endovascular repair (TEVAR) in patients with CTBAD remain controversial. Thus, this study aimed to assess and compare the mid- and long-term clinical outcomes of OSR via left thoracotomy with that of TEVAR for CTBAD. The data of 85 consecutive patients who underwent surgery for CTBAD from April 2007 to May 2021 were retrospectively reviewed. The patients were divided into two groups: Group G, which included patients who underwent OSR, and Group E, which included patients who underwent TEVAR. Groups G and E comprised 33 and 52 patients, respectively. Preoperative and postoperative computed tomography (CT) studies were retrospectively analyzed for the maximum diameter. The mean duration of the follow-up period was 5.8 years. Operative mortality did not occur. There was no difference in complications, such as stroke (G: 2 vs. E: 0, p = 0.30), paraplegia (G: 1 vs. E: 1, p = 0.66), and respiratory failure (G: 2, vs. E: 0, p = 0.30). The difference in preoperative factors was observed, including the intervals between onset and operation (G; 4.9 years vs. E; 1.9 years, p < 0.01), maximum diameter in preoperative CT (G; 59.0 mm vs. E; 50.5 mm, p < 0.001), and maximum false lumen diameter (G; 35.5 mm vs. E; 29.0 mm, p < 0.01). There was no significant difference in the mid- and long-term survival rates (p = 0.49), aorta-related deaths (p = 0.33), and thoracic re-intervention rates (p = 0.34). Postoperative adverse events occurred in Group E: four cases of retrospective type A aortic dissection, two cases of aorto-bronchial fistula, and one case of aorto-esophagus fistula. Aorta-related death and re-intervention rates crossed over in both groups after seven years postoperatively. Although endovascular repair of CTBAD is less invasive, the rate of freedom from re-intervention was unsatisfactory. Some fatal complications were observed in the endovascular group, and the mid- and long-term outcomes were reversed compared with those in the OSR group. Although OSR is an invasive procedure, it could be performed safely without perioperative complications. OSR has more feasible mid- and long-term outcomes.
Similar content being viewed by others
Introduction
Medical management remains the standard treatment modality of type B aortic dissection (TBAD). Different strategies are required for chronic complicated and uncomplicated cases. Although appropriate medical therapy has been administered, dilation of the aneurysm in the subacute or chronic phase has been reported, with a growth rate of 4 mm/year in the thoracic aorta [1]. Particularly, residual dissection particularly persists in patients with acute aortic dissection. In the chronic phase, conventional open surgery or thoracic endovascular aortic repair (TEVAR) should be performed in those with malperfusion, intractable pain, or other severe complications [2,3,4]. Treatment aim is to prevent aortic-related death in mid- and late-term outcomes. Although open surgery or the endovascular approach has been discussed, their roles in patients with chronic TBAD remain controversial. Thus, this single-center study aimed to assess the mid- and long-term clinical outcomes of conventional open surgery compared with TEVAR for chronic TBAD (CTBAD).
Materials and methods
Patients and study design
Data were obtained from the database of Saitama Medical University International Medical Center. The study protocol was approved by our Institutional Ethics Committee (ID: 19–164, September 4, 2019).
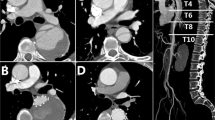
The records of 107 consecutive patients who underwent surgery for chronic TBAD at our center between July 2007 and May 2021 were retrospectively reviewed. A total of 22 were excluded because they underwent total aortic arch replacement using the frozen elephant trunk technique. Meanwhile, 33 patients were treated with conventional open surgical repair (Group G), and 52 underwent TEVAR (Group E). The operative indication for TEVAR for CTBAD was a dilated aneurysm > 50 mm in the descending aorta in both groups and an adequate proximal and distal landing zone for endovascular treatment. By contrast, extensive aneurysms involving the entire thoracic and thoracoabdominal aorta and its branches required open repair. The decision to perform TEVAR or open surgical repair was based on the patients' clinical status of multiple preoperative comorbidities including the procedure era. The era of TEVAR was after 2011, whereas open surgical repair was after 2007. Early-, mid-, and long-term results were retrospectively analyzed.
Surgical procedures
Perioperative cerebrospinal fluid drainage was performed for high-risk cases of paraplegia in both groups before surgery. Group G involved exposure of the thoracic descending and thoracoabdominal aorta through the left thoracotomy (n = 25) and thoracoabdominal incision (n = 8). All patients in Group G underwent selective ventilation of the single right lung. Partial cardiopulmonary bypass was established via the femoral artery and venous drainage; total cardiopulmonary bypass and circulatory arrest were rarely required. An aortic cross-clamp is usually placed distal to the left subclavian artery. However, if the initial entry was placed near the left subclavian artery, an aortic cross-clamp must be placed between the left common carotid and left subclavian arteries. For proximal and distal anastomosis, a commercial woven Dacron graft was used for central aortic replacement and reinforced with Teflon felt strips. The remaining thoracic aorta was opened; the upper intercostal arteries were ligated. Lower thoracic intercostal arteries were temporally occluded using balloon-tipped catheters. Four cases required intercostal re-implantation with a graft. Some patients underwent surgery under induced hypothermic circulatory arrest using profound hypothermia of 26 ℃. In cases requiring thoracoabdominal replacement, the repair of the visceral and renal artery was reattached, which was usually performed using a Carrel patch directly to the aortic graft. In addition, in all patients in Group G, motor-evoked potentials (MEPs) were used with or without re-implantation of the intercostal arteries.
Regarding Group E, who underwent TEVAR, the therapeutic strategy was to exclude primary entry and those who presented with proximal aneurysms of the descending aorta, in which there were sufficient proximal and distal landing zones, and thus, not off-label use. Depending on the endovascular device used, sheath placement may be required before endograft positioning. Balloon molding of the endograft was avoided. Device oversizing was less than 10%.
Study variables and definitions
All patient data were retrospectively reviewed. The follow-up was completed with a mean period of 5.8 years (standard deviation [SD] 3.0). Aortic dissection was defined as Stanford classification type B, which is a dissection of the entry site distal to the left subclavian artery. In this study, “chronic” aortic dissection was determined by an interval period over 30 days after symptom onset, based on the International Registry of Aortic Dissection (IRAD) [5].
The diagnosis was based on clinical history and non-invasive imaging study (computed tomography [CT] angiography). Hospital death was defined as death from hospital admission to discharge or within 30 days after surgery. Adverse events as early outcomes were defined as operative death, stroke, paraplegia, or respiratory failure requiring tracheostomy. Stroke was defined as a neurological disorder diagnosed by CT or magnetic resonance imaging after open surgery or TEVAR. Paraplegia was defined as a permanent bilateral motor deficit of the lower extremities.
The primary outcomes were mid- and long-term survival rates, including freedom from all-cause and aorta-related death (ARD). The secondary outcomes were defined as freedom from aortic adverse events in mid- and long-term outcomes. Aortic adverse events included retrograde type A aortic dissection (RTAD), aortoesophageal fistula (AEF), aorto-bronchial fistula (ABF), and thoracic aortic re-intervention. Thoracic aortic re-intervention was defined as additional open or endovascular repair of the descending thoracic and thoracoabdominal aortas due to the progression of aortic disease.
Statistical analysis
The results for categorical variables are expressed as numbers (percentages of the total). Continuous variables are presented as mean ± SD. The cumulative rate was determined using the Kaplan–Meier method. Logistic regression analysis was used to examine the significance of the clinical, diameter-calculated CT and operative variables. Differences in outcomes were considered statistically significant when p < 0.05. The χ2 test was used to compare categorical variables. The Fisher’s exact test was used if the expected frequency was < 5. Continuous variables were compared using Student’s t test. All statistical analyses were performed using JMP version 14.0 (SAS Institute Inc., Cary. NC. USA).
Results
Patient characteristics
The baseline characteristics and patient profiles are summarized in Table 1. Comorbidities, such as hypertension, dyslipidemia, diabetes mellitus, chronic kidney disease, coronary artery disease, history of stroke, and prevalence of chronic obstructive pulmonary disease, were not significantly different between the two groups. The patients in Group G were significantly younger than those in Group E, with a significant difference (60.1 ± 14.1 years vs. 68.6 ± 11.6 years, p < 0.01). The interval between the onset of TBAD and operation was 4.9 ± 3.9 years in Group G and 1.9 ± 2.9 years in Group E, showing significant differences in each group (p < 0.01). A preoperative CT review demonstrated that the maximum diameter of the descending aorta in Group G was larger than that in Group E (G; 59.0 ± 9.3 mm, E; 50.5 ± 7.9 mm, p < 0.001), as well as the maximum diameter of the false lumen (G; 35.5 ± 13.8 mm, E; 9.0 ± 10.0 mm, p < 0.01).
Perioperative outcomes
All procedures in both groups were technically successful. The thoracoabdominal aortic replacement was performed in eight patients in Group G. Perioperative results are presented in Table 2. Thirty-day mortality was not observed in either group. The overall hospital death rate was only 3.0% (one patient) in Group G due to postoperative low-output syndrome. Two patients (6.0%) in Group G had a stroke, and none in Group E. Paraplegia developed in one patient (3.0%) in Group G and one patient (1.9%) in Group E. Respiratory failure requiring tracheostomy was observed in two patients (6.0%) in Group G, and none in Group E. Group E had better surgical outcomes in terms of fewer complications than did Group G, without finding statistically significant differences. However, in Group E, RTAD occurred in four patients: three were salvageable and one died (Table 3).
Mid- and long-term outcomes
The overall estimated postoperative survivals at 5, 7, and 10 years, as assessed by the Kaplan–Meier method in Group G, were 84.9%, 74.5%, and 65.2%, respectively, and 81.6%, 78.7%, and 60.9%, respectively, in Group E (p = 0.49) (Fig. 1). Delayed mortality occurred in two patients who underwent open surgery for stroke, one patient in Group G who had hemoptysis and developed ABF, and seven patients in Group E due to aneurysm rupture (n = 3), AEF (n = 1), RTAD (n = 1), and heart failure (n = 1). The cause of death could not be confirmed in one patient.
The avoidance of aortic-related death was not significantly different between the two groups at 10 years (84.9% in Group G and 74.9% in Group E). However, the rate crossed over at seven years postoperatively (Fig. 2) (p = 0.33).
Figure 3 shows the estimated Kaplan–Meier curves of freedom from thoracic re-intervention for Group G and Group E. The overall postoperative freedom from thoracic re-intervention at 5, 7, and 10 years in Group G were 76.3%, 67.8%, and 50.9%, respectively, and 72.8%, 58.5%, and 48.8% in Group E, without a significant difference (p = 0.34). The rate of re-intervention was consistently worse in Group E. The indications for re-intervention were pseudo-aneurysm of the proximal site (n = 3) and false lumen enlargement in micron graft failure (n = 2) in Group G. The causes of late open conversion in Group E were stent-graft infection (n = 1), AEF (n = 1), type 1a endoleak (n = 1), and type 3b endoleak (n = 1). The causes of open conversion are shown in Table 4.
Discussion
The current gold standard therapy for uncomplicated acute TBAD is optimal medical therapy aiming to limit the progression of dissection by reducing aortic wall pressure. Some reports indicated that patients who did not undergo surgery and received optimal medical treatment had a 90–100% in-hospital survival rates and a 5-year survival of 50–87% [5,6,7,8,9,10,11]. In addition, the INSTEAD trial showed complete false lumen thrombosis 2 years after medical treatment in only 19.4% of patients compared with 91.3% in those after TEVAR [7, 12]. However, the effectiveness of conservative therapy in uncomplicated CTBAD remains unclear, which means that it may result in unfavorable long-term outcomes due to severe complications, such as rupture and malperfusion [13]. Desai et al. [14] reported that patients who underwent TEVAR for uncomplicated acute TBAD were successfully treated for the next 10 years but then experienced recurrence. The IRAD recently reported that a mean annual progressive aortic expansion was observed in 59% of patients with medically treated TBAD, with an expansion rate of 1.7 ± 7.6 mm/year [15].
Chronic aortic dissection carries a high risk of late aneurysmal dilation mainly due to false lumen enlargement and rupture. Thus, surgical treatment was indicated. Operative therapy was defined as open or endovascular repair. Endovascular repair has supplanted open surgery for the treatment of the descending aorta, with good short-term results. However, the preference for endovascular surgery for CTBAD remains controversial. Several studies reported in a systematic review that the long-term advantage of endovascular repair over open repair remains unclear and requires further investigation [4, 16, 17].
A careful treatment strategy for CTBAD is required for endovascular repair, which not only targets the occlusion of the proximal entry tear but also of the false lumen to prevent aortic dilation and promote aortic remodeling. Stent graft coverage of the aortic entry tear provides mid- and long-term results of sealing the primary entry, including false lumen thrombosis, which can potentially reduce late ARDs. In addition, devices and delivery systems, as well as an understanding of potential complications, may improve endovascular repair [18].
However, endovascular repair does not deliver the expected results. Guangqi et al. [19] reported that 22 of 121 consecutive patients who underwent endovascular repair of acute and CTBAD had postoperative endoleaks, with a 30-day mortality rate of 8.2%. TEVAR is not risk-free and has a high 30-day mortality rate; severe complications, such as RTAD (2.5–8%) [20, 21], stroke (4.6%), and paraplegia (1.9–4.4%) may also occur [22, 23]. TEVAR in patients with extensive aneurysmal sac may have limitations in terms of aneurysm size and location, occlusion by the false lumen, or thrombus formation for CTBAD [4, 24]. In our study, as presented in Table 4, the causes of open conversion after TEVAR were RTAD during the early postoperative period, infection during the mid-term outcomes, and type 1a and 3b endoleaks during the long-term outcomes. The choice of TEVAR for CTBAD remains controversial because stent grafting bears the risk of eliminating antegrade false lumen flow by persisting through the primary entry. In contrast, retrograde false lumen flow persists through potential dissection re-entry more distally. Regarding CTBAD, false lumen patency can cause worse outcomes. Therefore, TEVAR alone cannot be used in false lumens, which should be treated to promote thrombosis or excluded from systemic circulation [1]. In other words, the treatment of chronic aortic dissection requires intervention in the false lumen, and retrograde false lumen perfusion should be controlled to maintain perfusion and pressurization [24].
Open surgical repair is an acceptable option for most patients with progressive aneurysmal dilation of CTBAD. In our study, there were no ARDs in Group G in the early outcomes, and only seven (21.2%) cases occurred in the mid- and long-term outcomes, which was not significantly different from that in Group E. In addition, few perioperative complications, such as stroke, paraplegia, and respiratory failure, occurred, which was not significantly different from that in Group E. Furthermore, only one patient had fatal complications, such as aorto-bronchial fistula, in the mid- and long-term outcomes. Some reports have mentioned that conventional open surgery is acceptable, with reported in-hospital mortality rates between 9.6 and 22.4% [25, 26] and a 5-year survival rate of 78% in other studies of thoracoabdominal aortic replacements [25, 27]. In patients with chronic aortic dissection, control of blood flow in the false lumen is debatable. Yamana et al. [28] reviewed the mid-term results of the open repair of chronic aortic dissection with anastomosis to the true lumen only and both true and false lumens. They indicated that there were no differences in survival, ARD, late distal aortic events, and false lumen conditions, although thrombosis of the false lumen was better with true lumen only. Nozdrzykowski et al. [24] indicated that the treatment of CTBAD in patients with extensive aneurysms, malperfusion, or acute rupture may be surgically challenging, and the use of TEVAR might be limited in terms of aneurysm size and location, occlusion by the false lumen of the dissection, or thrombus formation within the chronic aneurysm. Fleerakkers et al. [29] reported that in patients with chronic dissections and aneurysmal degeneration, open surgery remains the gold standard, particularly in younger patients with reasonable life expectancy and limited comorbidities. TEVAR or fenestrated and branched endovascular repair can be considered in selecting patients (frail older patients) with suitable anatomy. Our results indicated that open repair CTBAD could be performed safely, although invasive.
However, even using open repair, the risk of re-intervention remains uncertain. Boufi et al. [30] discussed that open repair was not exempt from re-intervention risk. Indeed, in the open group, the rate was as high as 12%, with more than half with the distal expansion of the dissected aorta. However, distal anastomosis is usually performed in the apparently healthy aorta. Ryomoto et al. [31] reported that open surgery is preferable for CTBAD but is associated with late adverse events in the distal unresected aortic portion. In our study, five patients (15.2%) required additional TEVAR for pseudo-aneurysm of the anastomotic site in the mid- and long-term outcomes. The results were similar to those of Group E, in which eight patients (15.4%) required re-intervention. Thus, additional procedures in the mid- and long-term outcomes were similar in both groups.
Intervention for CTBAD could be performed with good results, either using open or endovascular repair. Based on these results, as several other studies reported [29, 32], open repair remains the golden standard for CTBAD, particularly in patients with good life expectancy and limited comorbidities. TEVAR is indicated for high-risk patients for open surgery with anatomic features favorable for endovascular approach.
Limitations
Our study has several limitations. First, this was a retrospective study. Patient selection bias was not considered, which may have led to partially improved results compared with the anatomical and clinical status. Second, the cohort of treated patients was small. Third, the rates of major adverse outcomes were probably underestimated in both procedures. Furthermore, propensity matching was not performed for patient selection. Particularly, the age of the patients in Group E was significantly higher compared with those in Group G. Several studies have indicated that ages less than 60 years were associated with significantly increased aortic growth rates [1, 33, 34]. Preoperative CT showed that those in Group G had larger aortic aneurysm diameters than those in Group E. Therefore, a comparison with other cohort studies is necessary. Despite these limitations, we suggest that this study could provide a sole comparative assessment in which results were similar between the mid- and long-term outcomes.
Conclusion
Although endovascular repair of CTBAD is less invasive, the rate of freedom from re-intervention was unsatisfactory. Therefore, the preference for endovascular repair over open repair remains controversial. Some fatal complications, such as RTAD, AEF, and ABF, due to aneurysmal dilation were observed in the endovascular group in the mid- and long-term outcomes. Compared with endovascular repair, open repair can be performed safely without perioperative complications. Open repair has feasible mid- and long-term outcomes.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Sueyoshi E, Sakamoto I, Hayashi K, Yamaguchi T, Imada T (2004) Growth rate of aortic diameter in patients with type B aortic dissection during the chronic phase. Circulation 110:II256-11261
Erbel R, Alfonso F, Boileau C, Dirsch O, Eber B, Haverich A, Rakowski H, Struyven J, Radegran K, Sechtem U, Taylor J, Zollikofer C, Klein WW, Mulder B, Task Force on Aortic Dissection, European Society of Cardiology (2001) Diagnosis and management of aortic dissection. Eur Heart J 22:1642–1681
Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, Evangelista A, Fattori R, Suzuki T, Oh JK, Moore AG, Malouf JF, Pape LA, Gaca C, Sechtem U, Lenferink S, Deutsch HJ, Diedrichs H, Marcos y Robles J, Llovet A, Gilon D, Das SK, Armstrong WF, Deeb GM, Eagle KA, (2000) The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 283:897–903
Svensson LG, Kouchoukos NT, Miller DC, Bavaria JE, Coselli JS, Curi MA, Eggebrecht H, Elefteriades JA, Erbel R, Gleason TG, Lytle BW, Mitchell RS, Nienaber CA, Roselli EE, Safi HJ, Shemin RJ, Sicard GA, Sundt TM 3rd, Szeto WY, Wheatley GH 3rd, Society of Thoracic Surgeons Endovascular Surgery Task Force (2008) Expert consensus document on the treatment of descending thoracic aortic disease using endovascular stent-grafts. Ann Thorac Surg 85:S1–S41
Booher AM, Isselbacher EM, Nienaber CA, Trimarchi S, Evangelista A, Montgomery DG, Froehlich JB, Ehrlich MP, Oh JK, Januzzi JL, O’Gara P, Sundt TM, Harris KM, Bossone E, Pyeritz RE, Eagle KA, Investigators IRAD (2013) The IRAD classification system for characterizing survival after aortic dissection. Am J Med 126:730.e19-e24
Afifi RO, Sandhu HK, Leake SS, Boutrous ML, Kumar V 3rd, Azizzadeh A, Charlton-Ouw KM, Saqib NU, Nguyen TC, Miller CC 3rd, Safi HJ, Estrera AL (2015) Outcomes of patients with acute type B (DeBakey III) aortic dissection: a 13-year, single-center experience. Circulation 132:748–754
Brunkwall J, Kasprzak P, Verhoeven E, Heijmen R, Taylor P, Trialists ADSORB, Alric P, Canaud L, Janotta M, Raithel D, Malina W, Resch T, Eckstein HH, Ockert S, Larzon T, Carlsson F, Schumacher H, Classen S, Schaub P, Lammer J, Lönn L, Clough RE, Rampoldi V, Trimarchi S, Fabiani JN, Böckler D, Kotelis D, Böckler D, Kotelis D, von Tenng-Kobligk H, Mangialardi N, Ronchey S, Dialetto G, Matoussevitch V (2014) Endovascular repair of acute uncomplicated aortic type B dissection promotes aortic remodelling: 1 year results of the ADSORB trial. Eur J Vasc Endovasc Surg 48:285–291
Fattori R, Montgomery D, Lovato L, Kische S, Di Eusanio M, Ince H, Eagle KA, Isselbacher EM, Nienaber CA (2013) Survival after endovascular therapy in patients with type B aortic dissection: a report from the International Registry of Acute Aortic Dissection (IRAD). JACC Cardiovasc Interv 6:876–882
Luebke T, Brunkwall J (2014) Type B aortic dissection: a review of prognostic factors and meta-analysis of treatment options. Aorta (Stamford) 2:265–278
Nienaber CA, Kische S, Rousseau H, Eggebrecht H, Rehders TC, Kundt G, Glass A, Scheinert D, Czerny M, Kleinfeldt T, Zipfel B, Labrousse L, Fattori R, Ince H, INSTEAD-XL trial, (2013) Endovascular repair of type B aortic dissection: long-term results of the randomized investigation of stent grafts in aortic dissection trial. Circ Cardiovasc Interv 6:407–416
Song C, Lu Q, Zhou J, Yu G, Feng X, Zhao Z, Bao J, Feng R, Jing Z (2016) The new indication of TEVAR for uncomplicated type B aortic dissection. Medicine (Baltimore) 95:e3919
Nienaber CA, Rousseau H, Eggebrecht H, Kische S, Fattori R, Rehders TC, Kundt G, Scheinert D, Czerny M, Kleinfeldt T, Zipfel B, Labrousse L, Ince H, Trial INSTEAD (2009) Randomized comparison of strategies for type B aortic dissection: the INvestigation of STEnt Grafts in Aortic Dissection (INSTEAD) trial. Circulation 120:2519–2528
Nienaber CA, Zannetti S, Barbieri B, Kische S, Schareck W, Rehders TC, INSTEAD study collaborators (2005) INvestigation of STEnt grafts in patients with type B Aortic Dissection: design of the INSTEAD trial–a prospective, multicenter, European randomized trial. Am Heart J 149:592–599
Desai ND, Pochettino A, Szeto WY, Moser GW, Moeller PJ, Sodhi N, Jackson B, Woo E, Fairman RM, Bavaria J (2011) Thoracic endovascular aortic repair: evolution of therapy, patterns of use, and results in a 10-year experience. J Thorac Cardiovasc Surg 142:587–594
Jonker FH, Trimarchi S, Rampoldi V, Patel HJ, O’Gara P, Peterson MD, Fattori R, Moll FL, Voehringer M, Pyeritz RE, Hutchison S, Montgomery D, Isselbacher EM, Nienaber CA, Eagle KA, International Registry of Acute Aortic Dissection (IRAD) Investigators (2012) Aortic expansion after acute type B aortic dissection. Ann Thorac Surg 94:1223–1229
Fattori R, Cao P, De Rango P, Czerny M, Evangelista A, Nienaber C, Rousseau H, Schepens M (2013) Interdisciplinary expert consensus document on management of type B aortic dissection. J Am Coll Cardiol 61:1661–1678
Tian DH, De Silva RP, Wang T, Yan TD (2014) Open surgical repair for chronic type B aortic dissection: a systematic review. Ann Cardiothorac Surg 3:340–350
Roselli EE (2015) Thoracic endovascular aortic repair versus open surgery for type-B chronic dissection. J Thorac Cardiovasc Surg 149:S163–S167
Guangqi C, Xiaoxi L, Wei C, Songqi L, Chen Y, Zilun L, Shenming W (2009) Endovascular repair of Stanford type B aortic dissection: early and mid-term outcomes of 121 cases. Eur J Vasc Endovasc Surg 38:422–426
Chen Y, Zhang S, Liu L, Lu Q, Zhang T, Jing Z (2017) Retrograde type A aortic dissection after thoracic endovascular aortic repair: a systematic review and meta-analysis. J Am Heart Assoc 6:e004649
Yammine H, Briggs CS, Stanley GA, Ballast JK, Anderson WE, Nussbaum T, Madjarov J, Frederick JR, Arko FR 3rd (2019) Retrograde type A dissection after thoracic endovascular aortic repair for type B aortic dissection. J Vasc Surg 69:24–33
Khoynezhad A, Donayre CE, Bui H, Kopchok GE, Walot I, White RA (2007) Risk factors of neurologic deficit after thoracic aortic endografting. Ann Thorac Surg 83:S882–S889
Czerny M, Eggebrecht H, Sodeck G, Verzini F, Cao P, Maritati G, Riambau V, Beyersdorf F, Rylski B, Funovics M, Loewe C, Schmidli J, Tozzi P, Weigang E, Kuratani T, Livi U, Esposito G, Trimarchi S, van den Berg JC, Fu W, Chiesa R, Melissano G, Bertoglio L, Lonn L, Schuster I, Grimm M (2012) Mechanisms of symptomatic spinal cord ischemia after TEVAR: insights from the European Registry of Endovascular Aortic Repair Complications (EuREC). J Endovasc Ther 19:37–43
Nozdrzykowski M, Etz CD, Luehr M, Garbade J, Misfeld M, Borger MA, Mohr FW (2013) Optimal treatment for patients with chronic Stanford type B aortic dissection: endovascularly, surgically or both? Eur J Cardiothorac Surg 44:e165–e174
Bozinovski J, Coselli JS (2008) Outcomes and survival in surgical treatment of descending thoracic aorta with acute dissection. Ann Thorac Surg 85:965–970
Leshnower BG (2018) Better candy for the false lumen. J Thorac Cardiovasc Surg 155:1973
Zoli S, Etz CD, Roder F, Mueller CS, Brenner RM, Bodian CA, Di Luozzo G, Griepp RB (2010) Long-term survival after open repair of chronic distal aortic dissection. Ann Thorac Surg 89:1458–1466
Yamana K, Takami Y, Niwa W, Matsuhashi K, Sakurai Y, Amano K, Akita K, Maekawa A, Takagi Y (2023) Mid-term results of distal anastomosis to the true lumen for chronic type B aortic dissection. Heart Vessels 38:849–856
Fleerakkers J, Schepens M (2019) How should we manage type B aortic dissections? Gen Thorac Cardiovasc Surg 67:154–160
Boufi M, Patterson BO, Loundou AD, Boyer L, Grima MJ, Loftus IM, Holt PJ (2019) Endovascular versus open repair for chronic type b dissection treatment: a meta-analysis. Ann Thorac Surg 107:1559–1570
Ryomoto M, Sakaguchi T, Tanaka H, Yamamura M, Sekiya N, Yajima S, Uemura H, Sato A (2022) Surgical strategy for chronic type B dissecting aortic aneurysm to prevent aorta-related events. Ann Vasc Surg 82:294–302
van Bogerijen GH, Patel HJ, Williams DM, Yang B, Dasika NL, Eliason JL, Deeb GM (2015) Propensity adjusted analysis of open and endovascular thoracic aortic repair for chronic type B dissection: a twenty-year evaluation. Ann Thorac Surg 99:1260–1266
Tolenaar JL, van Keulen JW, Jonker FH, van Herwaarden JA, Verhagen HJ, Moll FL, Muhs BE, Trimarchi S (2013) Morphologic predictors of aortic dilatation in type B aortic dissection. J Vasc Surg 58:1220–1225
van Bogerijen GH, Tolenaar JL, Rampoldi V, Moll FL, van Herwaarden JA, Jonker FH, Eagle KA, Trimarchi S (2014) Predictors of aortic growth in uncomplicated type B aortic dissection. J Vasc Surg 59:1134–1143
Funding
Open Access funding provided by Saitama Medical University.
Author information
Authors and Affiliations
Contributions
Akitoshi Takazawa: conceptualization, data curation, formal analysis, investigation, project administration, writing-original draft; writing – review & editing. Toshihisa Asakura: supervision. Osamu Kinoshita: data curation. Hiroyuki Nakajima: data curation. Akihiro Yoshitake: supervision, statistical analysis, methodology, and validation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Saitama Medical University International Medical Center Ethics Committee (ID: 19–164; September 4, 2019).
Informed consent
Verbal informed consent was obtained and writen informed consent was waived by the Saitama Medical University International Medical Center Ethics Committee. This research was retrospective and consisted of surveys with reports presented no more than minimal risk of harm to subjects and involved no procedures for which written consent is normally required outside the research context.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Takazawa, A., Asakura, T., Kinoshita, O. et al. Mid- and long-term results of open repair for chronic type B aortic dissection in endovascular era. Heart Vessels (2024). https://doi.org/10.1007/s00380-024-02399-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00380-024-02399-1