Abstract
Little is known regarding the long-term (> 10 years) outcomes and risk factors of total arterial coronary artery bypass grafting (CABG). This study evaluated the long-term outcomes and risk factors for all-cause mortality and major adverse cardiac and cerebrovascular events (MACCEs) following total arterial on-pump CABG (ONCAB) or off-pump CABG (OPCAB) with complete revascularization. This retrospective cohort analysis enrolled patients with stable angina who underwent total arterial CABG with complete revascularization in our institute between July 2000 and June 2019. The endpoints were all-cause mortality and MACCE incidence, including a comparison between OPCAB and ONCAB. Long-term (10-year) outcomes were analyzed using propensity score-matched pairs, and risk factors were evaluated using univariate and multivariate analyses. Overall, 401 patients who underwent primary total arterial CABG were classified into the OPCAB (n = 269) and ONCAB (n = 132) groups. Using propensity score matching (PSM), 88 patients who underwent OPCAB were matched with 88 patients who underwent ONCAB. The mean follow-up period was 7.9 ± 6.3 years. No significant difference in all-cause mortality (hazard ratio, 1.04; 95% confidence interval, 0.53–2.04; p = 0.9138) and MACCE incidence (hazard ratio, 1.06; 95% confidence interval, 0.68–1.65; p = 0.7901) was observed between the two groups. Renal failure requiring dialysis was a significant risk factor for mortality (p < 0.0001) and MACCEs (p = 0.0003). Long-term outcomes of total arterial OPCAB and ONCAB with complete revascularization showed similar findings using PSM. Renal failure requiring dialysis was a significant risk factor for mortality and morbidity.Journal standard instruction requires an unstructured abstract; hence the headings provided in abstract were deleted. Kindly check and confirm.Thank you for your kindness.
Clinical registration number 5598, Tokyo Women’s Medical University Hospital.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The SYNTAX trial showed that coronary artery bypass grafting (CABG) is more effective than percutaneous coronary intervention (PCI) in complex coronary artery regions [1,2,3].
It is also apparent that failure rates are predominantly higher with saphenous vein grafts (SVG) than with arterial grafts in terms of perioperative outcomes [4, 5]. Furthermore, CABG using arterial grafts could improve mid-term survival (up to 10 years) [6,7,8].
However, there is limited information regarding the long-term (> 10 years) outcomes and risk factors for total arterial CABG. Furthermore, comparisons of outcomes between total arterial off-pump CABG (OPCAB) and on-pump CABG (ONCAB) with complete revascularization have not been reported often.
Thus, this study aimed to assess the clinical benefits of total arterial OPCAB compared with those of ONCAB with complete revascularization using propensity score matching (PSM) and to reveal the risk factors for total arterial CABG. Additionally, the study examined the 30-day complications, details of postoperative graft patency, and risk factors for mortality and MACCEs.
Materials and methods
Study design
This study was a retrospective cohort analysis of patients with stable angina who underwent total arterial CABG with complete revascularization in our institute between July 2000 and June 2019. The inclusion and exclusion criteria for selecting the study participants are summarized in Table 1. Younger patients underwent total arterial CABG for long-term patency.
Please check and confirm the layout of all tables.Thank you. I have checked and confirmed that everything is in order
The preoperative risk score was calculated based on patients’ characteristics. Postoperative coronary angiography was routinely performed on patients depending on their renal function. All patients were administered selective graft injections.
The Institutional Review Board of Tokyo Women’s Medical University approved this study (Approval No. 5598). The review board waived the need for informed consent because of the retrospective nature of this study. This study was performed in conformance with the Declaration of Helsinki.
Operation
ONCAB was performed previously at the facility. Recently, depending on the surgeon’s preference, OPCAB is now the preferred option. Both procedures were performed by several surgeons. Prophylactic intra-aortic balloon pumping (IABP) was performed for patients with severe left main trunk disease or a low left ventricular ejection fraction (LVEF).
All arterial grafts were harvested in a skeletonized manner using an ultrasonic scalpel (Harmonic Scalpel; Ethicon Endosurgery, Cincinnati, OH). The left internal thoracic artery (LITA), right internal thoracic artery (RITA), and gastroepiploic artery (GEA) were used as in-situ grafts. The radial artery (RA) was anastomosed to the ascending aorta as central anastomosis and in-situ grafts were divided after heparinization. The bilateral internal thoracic artery and in-situ gastroepiploic artery (GEA) were the preferred in-situ grafts with OPCAB to achieve total arterial revascularization.
Surgical technique for OPCAB
A stabilizer (Octopus, Medtronic, Minneapolis, MN, USA) was used for the heart. Two deep pericardial sutures were placed in the posterior pericardium between the inferior vena cava and the left lower pulmonary vein, exposing the lateral or inferior walls. A bloodless field was acquired using a proximal snare and a carbon dioxide blower. Each anastomosis was performed using an 8-0 polypropylene running suture with the parachute technique. The graft patency was assessed using transit-time flow measurement before and after protamine reversal.
Surgical technique for ONCAB
After preparing the conduits, standard cannulation for cardiopulmonary bypass was performed using ascending aortic cannulation and dual-stage cannulation of the right atrium with an antegrade cardioplegia cannula. The aorta was clamped, and cold blood cardioplegia was injected every 20 min. After completing the anastomosis, the patient was weaned off cardiopulmonary bypass. Similarly, graft patency was assessed using transit-time flow measurement before and after protamine reversal.
Postoperative coronary angiography
Postoperative coronary angiography was performed around 1–2 weeks postoperatively before discharge. The exclusion of postoperative coronary angiography was determined by considering patients’ renal function and general condition.
Definition of complete revascularization
Complete revascularization was defined as the treatment of any lesion with > 75% area stenosis in vessels measuring ≥ 1.0 mm, as estimated on the diagnostic angiography.
Study outcomes
The primary endpoint was all-cause mortality, including the comparison between OPCAB and ONCAB. In contrast, the secondary endpoint was the incidence of MACCEs.
Statistical analysis
Continuous variables are reported as mean ± standard deviation and number (%) and were analyzed using an unpaired t-test or Mann–Whitney U test. Categorical variables were analyzed using Pearson’s Chi-squared test. Survival curves were drawn on an actuarial basis using the Kaplan–Meier technique, and comparisons were made using Cox proportional hazard ratios and the log-rank test. Univariate and multivariate Cox proportional hazard regression models were constructed to identify independent predictors of mortality and MACCEs.
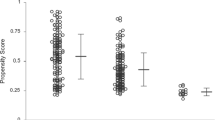
Considering the differences between the baseline characteristics of the two groups, PSM was used to identify a cohort of patients with similar baseline characteristics, matched for age, male sex, body mass index, old myocardial infarction, previous PCI, previous stroke, peripheral arterial disease, renal failure requiring dialysis, hypertension, diabetes mellitus, diabetes mellitus with insulin, LVEF, LVEF < 35%, IABP, left main coronary disease, triple vessels coronary disease, JapanSCORE, euroSCORE II, Society of Thoracic Surgeons score, and SYNTAX score.
The propensity score was estimated with a non-parsimonious multivariable logistic regression model using all the baseline characteristics outlined in Table 1 as covariates. Matching was performed using a 1:1 matching protocol without replacement (greedy-matching algorithm), with a caliper width equal to 0.2 of the standard deviation of the logit of the propensity score.
A two-sided p-value of < 0.05 was considered statistically significant for all tests. All statistical analyses were performed using JMP Pro version 15 (SAS Institute Inc, Cary, NC, USA) software.
Results
Patient population
In total, 1498 patients underwent primary CABG in our institute. This study enrolled 401 of them who underwent primary total arterial CABG. All patients underwent complete revascularization. OPCAB and ONCAB were performed on 269 and 132 patients, respectively (Fig. 1). Although patients who underwent OPCAB and ONCAB were randomly, not sequentially, grouped, the number of OPCAB procedures in the facility has increased recently. Patients who underwent combined operations were excluded.
Preoperative characteristics
The preoperative characteristics of the patients are shown in Table 2. Before PSM, significant differences in the incidence of old myocardial infarction (OMI), hypertension (HT), and left ventricular ejection fraction (LVEF) ≤ 35% were observed between the two groups. Using PSM, 88 patients who underwent OPCAB were matched with 88 patients who underwent ONCAB.
Operative findings and postoperative graft patency
The operative findings and postoperative graft patency are shown in Table 3. Complete revascularization occurred in all cases. Distal anastomoses were performed individually or by employing a sequential technique. In terms of sequential anastomosis, the LITA, RITA, GEA, and RA were used in 113 of 395 (29%), 10 of 327 (3%), 54 of 215 (25%), and 11 of 47 (23%) cases, respectively. One case involved using the RITA extended with the RA as a composite graft due to heavy calcification of the ascending aorta. After PSM, significant differences were observed in the utilization rates of sequential grafts using the GEA (OPCAB: 35% vs. ONCAB: 6%, p = 0.0117) and RA (OPCAB: 78% vs. ONCAB: 29%, p = 0.0211). However, the number of distal anastomoses (OPCAB: 3.0 ± 1.0 vs. ONCAB: 2.9 ± 0.9, p = 0.3865) and conduits used were not significantly different between the two groups.
Postoperative coronary angiography was performed after a mean postoperative duration of 13.5 ± 8.7 days. Angiography was performed in 83% of patients who underwent OPCAB (n = 73) and ONCAB (n = 73). Graft patency for all patients (OPCAB: 92% vs. ONCAB: 92%, p = 1.0000) and all anastomoses (OPCAB: 97% vs. ONCAB: 97%, p = 0.9215) and 30-day mortality (OPCAB: 0% vs. ONCAB: 2%, p = 0.1549) were not significantly different between the two groups.
The details of postoperative graft patency are shown in Table 4. After PSM, graft patency for each graft and target was not different between the two groups.
The 30-day complications, including mortality, MACCEs, cerebral infarction, mediastinitis, and re-exploration, significantly differed between the two groups after PSM.
Primary endpoint
In total, 79.6% (n = 319) of patients were followed up for a mean duration of 7.9 ± 6.3 years. Figure 1 shows a matched comparison of the cumulative survival rates between the OPCAB and ONCAB groups, demonstrating no significant difference (OPCAB hazard ratio, 1.04; 95% confidence interval, 0.53–2.04; p = 0.9138).
Secondary endpoint
Figure 2 shows a matched comparison of the cumulative rates of freedom from MACCEs between the OPCAB and the ONCAB groups, demonstrating no significant difference (OPCAB hazard ratio, 1.06; 95% confidence interval, 0.68–1.65; p = 0.7901).
Cumulative rates of freedom from MACCEs in the matched cohort. The panel shows the cumulative rates of freedom from major adverse cardiac and cerebrovascular events in the matched cohort. The hazard ratios of the off-pump group compared to those of the on-pump group are shown. MACCEs major adverse cardiac and cerebrovascular events, OPCAB off-pump coronary artery bypass grafting, ONCAB on-pump coronary artery bypass grafting
Risk analysis
Table 5 shows the results of the univariate and multivariate analyses for all-cause mortality. Based on the univariate analysis, previous stroke, renal failure requiring dialysis, LVEF ≤ 35%, and IABP were significantly associated with mortality. Multivariate analysis for mortality revealed that previous stroke and IABP were not independently associated with mortality. In contrast, renal failure requiring dialysis (hazard ratio, 4.67; 95% confidence interval, 2.48–8.79; p < 0.0001) and LVEF ≤ 35% (hazard ratio, 2.00; 95% confidence interval, 1.11–3.62; p = 0.0219) were independently associated with mortality.
Table 6 shows the results of univariate and multivariate analyses for MACCE. Based on the univariate analysis results, renal failure requiring dialysis and LVEF ≤ 35% were significantly associated with mortality. The results of the multivariate analysis for MACCEs revealed that LVEF ≤ 35% was not independently associated with MACCEs. Contrastingly, renal failure requiring dialysis was independently associated with MACCEs (hazard ratio, 2.23; 95% confidence interval, 1.42–3.50; p = 0.0005).
Discussion
The SYNTAX trial revealed that CABG was more effective in repairing complex coronary artery regions than PCI [1,2,3] and that survival outcomes were better with arterial grafts than with SVGs [4]. However, most previous studies reported only mid-term results for mortality [4,5,6,7,8]. The present study showed the long-term survival rate after total arterial CABG with either the OPCAB or ONCAB technique with complete revascularization. Additionally, the study examined details of postoperative graft patency, 30-day complications, and risk factors for mortality and MACCEs.
The currently published evidence on long-term outcomes after OPCAB compared to ONCAB remains controversial [9,10,11,12,13,14,15]. No significant difference in all-cause mortality and MACCE incidence was observed between the two groups in this study. The 5-year survival rates reported in this study (OPCAB: 87.7% vs. ONCAB: 91.6%, p = 0.9164) were favorable relative to the outcomes in the ROOBY (OPCAB: 84.8% vs. ONCAB: 88.1%, p = 0.02) [9, 10], CORONARY (OPCAB: 85.4% vs. ONCAB: 86.5%, p = 0.30) [11, 12], GOPCABE (OPCAB: 69% vs. ONCAB: 70%, p = 0.71) [13], and SYNTAX [1, 2] (CABG: 89.9% vs. PCI: 91.1%, p = 0.64) trials. Furthermore, the 10-year survival rates reported in this study (OPCAB: 87.7% vs. ONCAB: 79.4%, p = 0.9164) were more favorable than those in the SYNTAX [3] (CABG: 76% vs. PCI: 72%, p = 0.066) trial. This study showed that total arterial OPCAB and ONCAB had similar survival rates. The favorable long-term mortality outcomes observed in this study were probably due to the total arterial CABG with better patency grafts [6] and complete revascularization.
Several studies have reported that arterial grafts have better patency compared to SVGs. Some of the existing literature addressing the superior outcomes of multiple arterial versus traditional CABG has reported the decreased progression of native vessel disease in coronary territories revascularized with arterial grafts compared with SVGs as an explanatory factor [16]. This finding was based on the review of a large amount of coronary recatheterization data in patients treated with CABG, and the relatively greater release of nitric oxide from arterial versus SVG tissues has been suggested as the mechanism for this protection of native coronary beds against atherosclerosis progression [16, 17].
Indeed, the present study only observed short-term patency. However, especially regarding arterial grafts, given that the short-term patency is confirmed, it is reasonable to assume that long-term patency could be expected and also ensured [18,19,20]. Before PSM, significant differences in OMI, HT, and LVEF ≤ 35% were observed between the two groups. These factors were predictors of adverse long-term outcomes after CABG [21,22,23,24,25]. However, these differences were mitigated after propensity score matching, and the study specifically focused on comparing OPCAB and ONCAB.
The important similarity between the two groups in this study was the achievement of complete revascularization. Incomplete revascularization has a detrimental impact on long-term mortality [26, 27]. The ROOBY trial [9, 10] reported that a smaller number of anastomoses (OPCAB: 2.9 ± 0.9 vs. ONCAB: 3.0 ± 1.0, p = 0.002) and a higher rate of graft failure (OPCAB: 17.4% vs. ONCAB: 12.2%, p < 0.001) were associated with poorer outcomes in patients who underwent OPCAB. The present study shows that complete revascularization is paramount for better long-term outcomes, either with OPCAB or ONCAB.
OPCAB is technically demanding in terms of complete revascularization and patency [9, 10]. This study showed that OPCAB and ONCAB had a similar number of distal anastomoses and patencies. The postoperative graft patency details were observed to compare each graft and target. After PSM, graft patency for each graft and target was not different between the two groups.
Additionally, the existing literature showed that OPCAB had less postoperative morbidity at 30 days [11, 28]. However, this difference was not statistically significant after PSM.
This study demonstrated that renal failure requiring dialysis was a common finding after CABG, with increased mortality and MACCEs, similar to the observations in the CREDO-Kyoto cohort [29]. Furthermore, the present study observed that LVEF ≤ 35% was an independent risk factor for mortality, as reported in the STICH trial [30]. In summary, complete revascularization achieved through arterial grafts, with long-term patency assured, is expected to improve long-term outcomes, regardless of whether OPCAB or ONCAB is employed.
This clinical study had certain limitations. First, it was a retrospective observational study. Second, the results are susceptible to selection bias, as demonstrated by the differences in baseline characteristics, even after a propensity score-matched comparison. Third and most importantly, the follow-up rate was relatively lower than intended. Two reasons for this phenomenon exist: (i) Many patients from all over Japan who visited our facility were enrolled; hence, long-term follow-up of distant patients was difficult, and (ii) most Japanese families are nuclear; hence, many patients relocated during the follow-up period. Based on these limitations, comparing these results to other studies may be insufficient. Hence, additional studies with a longer follow-up and larger data sets may be required for further analysis. Nonetheless, this is currently one of the longest follow-up studies with PSM on total arterial CABG from a single institution in Japan.
In conclusion, total arterial OPCAB and ONCAB with complete revascularization showed similar rates of graft patency, survival, and MACCE incidence using PSM. Furthermore, renal failure requiring dialysis was observed to be a significant risk factor for mortality and MACCEs.
Data availability
Derived data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW, Investigators SYNTAX (2009) Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 360:961–972
Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR, Morel MA, Van Dyck N, Houle VM, Dawkins KD, Serruys PW (2013) Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 381:629–638
Thuijs DJFM, Kappetein AP, Serruys PW, Mohr FW, Morice MC, Mack MJ, Holmes DR, Curzen N, Davierwala P, Noack T, Milojevic M, Dawkins KD, da Costa BR, Jüni P, Head SJ, Extended Survival Investigators SYNTAX (2019) Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet 394:1325–1334
Cameron A, Davis KB, Green G, Schaff HV (1996) Coronary bypass surgery with internal-thoracic-artery grafts—effects on survival over a 15-year period. N Engl J Med 334:216–219
Shah PJ, Gordon I, Fuller J, Seevanayagam S, Rosalion A, Tatoulis J, Raman JS, Buxton BF (2003) Factors affecting saphenous vein graft patency: clinical and angiographic study in 1402 symptomatic patients operated on between 1977 and 1999. J Thorac Cardiovasc Surg 126:1972–1977
Habib RH, Dimitrova KR, Badour SA, Yammine MB, El-Hage-Sleiman AK, Hoffman DM, Geller CM, Schwann TA, Tranbaugh RF (2015) CABG versus PCI: greater benefit in long-term outcomes with multiple arterial bypass grafting. J Am Coll Cardiol 66:1417–1427
Lytle BW, Blackstone EH, Loop FD, Houghtaling PL, Arnold JH, Akhrass R, McCarthy PM, Cosgrove DM (1999) Two internal thoracic artery grafts are better than one. J Thorac Cardiovasc Surg 117:855–872
Taggart DP, Benedetto U, Gerry S, Altman DG, Gray AM, Lees B, Gaudino M, Zamvar V, Bochenek A, Buxton B, Choong C, Clark S, Deja M, Desai J, Hasan R, Jasinski M, O’Keefe P, Moraes F, Pepper J, Seevanayagam S, Sudarshan C, Trivedi U, Wos S, Puskas J, Flather M, Investigators ART (2019) Bilateral versus single internal-thoracic-artery grafts at 10 years. N Engl J Med 380:437–446
Shroyer AL, Grover FL, Hattler B, Collins JF, McDonald GO, Kozora E, Lucke JC, Baltz JH, Novitzky D, Veterans Affairs Randomized On/Off Bypass (ROOBY) Study Group (2009) On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 361:1827–1837
Shroyer AL, Hattler B, Wagner TH, Collins JF, Baltz JH, Quin JA, Almassi GH, Kozora E, Bakaeen F, Cleveland JC, Bishawi M, Grover FL, Veterans Affairs ROOBY-FS Group (2017) Five-year outcomes after on-pump and off-pump coronary-artery bypass. N Engl J Med 377:623–632
Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Paolasso E, Straka Z, Piegas LS, Akar AR, Jain AR, Noiseux N, Padmanabhan C, Bahamondes JC, Novick RJ, Vaijyanath P, Reddy S, Tao L, Olavegogeascoechea PA, Airan B, Sulling TA, Whitlock RP, Ou Y, Ng J, Chrolavicius S, Yusuf S, CORONARY Investigators (2012) Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med 366:1489–1497
Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Straka Z, Piegas LS, Avezum A, Akar AR, Lanas Zanetti F, Jain AR, Noiseux N, Padmanabhan C, Bahamondes JC, Novick RJ, Tao L, Olavegogeascoechea PA, Airan B, Sulling TA, Whitlock RP, Ou Y, Gao P, Pettit S, Yusuf S, CORONARY Investigators (2016) Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med 375:2359–2368
Diegeler A, Börgermann J, Kappert U, Breuer M, Böning A, Ursulescu A, Rastan A, Holzhey D, Treede H, Rieß FC, Veeckmann P, Asfoor A, Reents W, Zacher M, Hilker M, GOPCABE Study Group (2013) Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 368:1189–1198
Puskas JD, Williams WH, Mahoney EM, Huber PR, Block PC, Duke PG, Staples JR, Glas KE, Marshall JJ, Leimbach ME, McCall SA, Petersen RJ, Bailey DE, Weintraub WS, Guyton RA (2004) Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA 291:1841–1849
Zhao DF, Edelman JJ, Seco M, Bannon PG, Wilson MK, Byrom MJ, Thourani V, Lamy A, Taggart DP, Puskas JD, Vallely MP (2017) Coronary artery bypass grafting with and without manipulation of the ascending aorta: a network meta-analysis. J Am Coll Cardiol 69:924–936
Dimitrova KR, Hoffman DM, Geller CM, Dincheva G, Ko W, Tranbaugh RF (2012) Arterial grafts protect the native coronary vessels from atherosclerotic disease progression. Ann Thorac Surg 94:475–481
Hayward PA, Zhu YY, Nguyen TT, Hare DL, Buxton BF (2013) Should all moderate coronary lesions be grafted during primary coronary bypass surgery? An analysis of progression of native vessel disease during a randomized trial of conduits. J Thorac Cardiovasc Surg 145:140–148 (discussion 148–149)
Ura M, Sakata R, Nakayama Y, Arai Y, Saito T (1998) Long-term patency rate of right internal thoracic artery bypass via the transverse sinus. Circulation 98:2043–2048
Suzuki T, Asai T, Nota H, Kuroyanagi S, Kinoshita T, Takashima N, Hayakawa M (2013) Early and long-term patency of in situ skeletonized gastroepiploic artery after off-pump coronary artery bypass graft surgery. Ann Thorac Surg 96:90–95
Deb S, Cohen EA, Singh SK, Une D, Laupacis A, Fremes SE, Fremes SE, Cohen EA, Feder-Elituv R, Laupacis A, Deb S, Singh SK, Une D, Buller C, Desai ND, Errett L, Morin JF, Myers ML, Novick R, Rubens FD, Yau T, Almond D, Dragatakis L, Higginson L, Schwartz L, Tymchak W, Watson R, Afshar M, Algarni K, Sever J, Katik M, Kiss A, Dubbin J, Ko D, Moody A, Pen V, Radhakrishnan S, Joyner C, Moussa F, Myers M, Del Rizzo D, Carrier M, Cartier R, Leclerc Y, Boyd D, Menkis A, Shum-Tim D, Bonneau D, Latter D, Abouzhar L, Bhatnagar G, Christakis GT, Cutrara C, Goldman B, Brister S, Cusimano RJ, Peniston C, Ralph-Edwards A, Scully H, Weisel R, Gelfand E, Penkoske P, Burr L, Fradet G, Thompson D, Finlay S, Fox R, Fox S, Germain S, Harris L, Hsu N, James MA, Jesina C, Keith M, Mokbel R, Montebruno L, Munoz A, Nacario C, Naidoo S, Sohal R, Tsang K (2012) Radial artery and saphenous vein patency more than 5 years after coronary artery bypass surgery: results from RAPS (Radial Artery Patency Study). J Am Coll Cardiol 60:28–35
Voisine P, Mathieu P, Doyle D, Perron J, Baillot R, Raymond G, Métras J, Dagenais F (2006) Influence of time elapsed between myocardial infarction and coronary artery bypass grafting surgery on operative mortality. Eur J Cardiothorac Surg 29:319–323
Ketonen M, Pajunen P, Koukkunen H, Immonen-Räihä P, Mustonen J, Mähönen M, Niemelä M, Kuulasmaa K, Palomäki P, Arstila M, Vuorenmaa T, Lehtonen A, Lehto S, Miettinen H, Torppa J, Tuomilehto J, Airaksinen J, Pyörälä K, Salomaa V (2008) Long-term prognosis after coronary artery bypass surgery. Int J Cardiol 124:72–79
Aronson S, Boisvert D, Lapp W (2002) Isolated systolic hypertension is associated with adverse outcomes from coronary artery bypass grafting surgery. Anesth Analg 94:1079–1084 (table of contents)
Herlitz J, Brandrup-Wognsen G, Karlson BW, Sjöland H, Karlsson T, Caidahl K, Hartford M, Haglid M (1999) Mortality, risk indicators, mode and place of death and symptoms of angina pectoris in the five years after coronary artery bypass grafting in patients with and without a history of hypertension. Blood Press 8:200–206
Awan NI, Jan A, Rehman MU, Ayaz N (2020) The effect of ejection fraction on mortality in coronary bypass grafting (CABG) patients. Pak J Med Sci 36:1454–1459
Farooq V, Serruys PW, Garcia-Garcia HM, Zhang Y, Bourantas CV, Holmes DR, Mack M, Feldman T, Morice MC, Ståhle E, James S, Colombo A, Diletti R, Papafaklis MI, de Vries T, Morel MA, van Es GA, Mohr FW, Dawkins KD, Kappetein AP, Sianos G, Boersma E (2013) The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol 61:282–294
Garcia S, Sandoval Y, Roukoz H, Adabag S, Canoniero M, Yannopoulos D, Brilakis ES (2013) Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol 62:1421–1431
Sabik JF, Gillinov AM, Blackstone EH, Vacha C, Houghtaling PL, Navia J, Smedira NG, McCarthy PM, Cosgrove DM, Lytle BW (2002) Does off-pump coronary surgery reduce morbidity and mortality. J Thorac Cardiovasc Surg 124:698–707
Natsuaki M, Furukawa Y, Morimoto T, Nakagawa Y, Akao M, Ono K, Shioi T, Shizuta S, Sakata R, Okabayashi H, Nishiwaki N, Komiya T, Suwa S, Kimura T (2011) Impact of diabetes on cardiovascular outcomes in hemodialysis patients undergoing coronary revascularization. Circ J 75:1616–1625
Velazquez EJ, Lee KL, Deja MA, Jain A, Sopko G, Marchenko A, Ali IS, Pohost G, Gradinac S, Abraham WT, Yii M, Prabhakaran D, Szwed H, Ferrazzi P, Petrie MC, O’Connor CM, Panchavinnin P, She L, Bonow RO, Rankin GR, Jones RH, Rouleau JL, Investigators STICH (2011) Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med 364:1607–1616
Acknowledgements
The authors would like to thank Kazutora Mizukami for his assistance with the statistical analysis.
Funding
None.
Author information
Authors and Affiliations
Contributions
Shizuya Shintomi: conceptualization; data curation; formal analysis; investigation; methodology; validation; visualization; and writing—original draft. Satoshi Saito: conceptualization; formal analysis; investigation; methodology; project administration; and validation. AH: conceptualization; formal analysis; investigation; methodology; project administration; and validation. YI: conceptualization; project administration; and supervision. KM: data curation; formal analysis; investigation; methodology; and validation. MI: investigation; methodology; and validation. SD: investigation; methodology; and validation. AF: investigation; methodology; and validation. HN: conceptualization; methodology; project administration; resources; supervision; and validation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shintomi, S., Saito, S., Hamasaki, A. et al. Propensity score-matched comparison of total arterial off- and on-pump coronary artery bypass with complete revascularization. Heart Vessels 39, 175–184 (2024). https://doi.org/10.1007/s00380-023-02317-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-023-02317-x