Abstract
To investigate the impact of the coronavirus disease 2019 (COVID-19) pandemic on myocardial infarctions (MIs), consecutive MI patients were retrospectively reviewed in a multi-center registry. The patient characteristics and 180-day mortality for both ST-segment elevation myocardial infarctions (STEMIs) and non-STEMIs (NSTEMIs) in the after-pandemic period (7 April 2020–6 April 2021) were compared to the pre-pandemic period (7 April 2019–6 April 2020). Inpatients with MIs, STEMIs, and NSTEMIs decreased by 9.5%, 12.5%, and 4.1% in the after-pandemic period. The type of the presenting symptoms (as classified as typical symptoms, atypical symptoms, and out-of-hospital cardiac arrests [OHCAs]) did not differ between the two time periods for both STEMIs and NSTEMIs, while the rate of OHCAs was numerically higher in the after-pandemic period for the STEMIs (12.1% vs. 8.0%, p = 0.30). The symptom-to-admission time (STAT) did not differ between the two time periods for both STEMIs and NSTEMIs, but the door-to-balloon time (DTBT) for STEMIs was significantly longer in the after-pandemic period (83.0 [67.0–100.7] min vs. 70.0 [59.0–88.7] min, p = 0.004). The 180-day mortality did not significantly differ between the two time periods for both STEMIs (15.9% vs. 11.4%, p = 0.14) and NSTEMIs (9.9% vs. 8.0%, p = 0.59). In conclusion, hospitalizations for MIs decreased after the COVID-19 pandemic. Although the DTBTs were significantly longer in the after-pandemic period, the mid-term outcomes for MIs were preserved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The world health organization (WHO) declared coronavirus disease 2019 (COVID-19) a pandemic on March 11, 2020. In Japan, a state of emergency declaration for COVID-19 was proposed in Tokyo, Saitama, Chiba, Kanagawa, Osaka, Hyogo, and Fukuoka prefectures on April 7, 2020. After that, both the Cardiovascular Intervention and Therapeutics (CVIT) [1] and Japanese Circulation Society (JCS) academic societies, [2] dealing with acute myocardial infarction (AMI) medical care, proposed an AMI treatment strategy, which aimed to prevent infections in health care workers and maintain the treatment in critically ill and urgent patients even during the COVID-19 spread.
Several studies from Japan have reported a significantly longer time of the door-to-balloon time (DTBT), while the short-term mortality has been preserved after the COVID-19 pandemic as compared to that before the pandemic in patients with ST-elevation myocardial infarctions (STEMIs) [3,4,5]. As for the patients with non-ST-elevation myocardial infarctions (NSTEMIs), there are few Japanese data focusing on investigating the impact of the COVID-19 pandemic. In our single-center retrospective observational study, we reported that, for NSTEMIs, the time from the onset of the myocardial infarctions (MIs) to admission was significantly longer and the short-term outcome worsened after the COVID-19 pandemic [6]. However, most reports are from a single-center registry with the short-term outcomes, and the impact of the COVID-19 pandemic on the mid-term outcomes for both STEMIs and NSTEMIs in Japan remains unknown. The purpose of this study was to investigate the clinical impact of the COVID-19 pandemic on both STEMIs and NSTEMIs focusing on the mid-term outcomes, by comparing the outcomes 1 year after the COVID-19 pandemic with those 1 year before the pandemic in a multi-center Japanese registry.
Methods
Study design and population
This registry of MIs was a retrospective observational multi-center study conducted at 6 Japanese medical institutions, including Nihon University School of Medicine, Tokyo, Japan, Nihon University Hospital, Tokyo, Japan, Tokyo Rinkai Hospital, Tokyo, Japan, Kawaguchi Municipal Medical Center, Saitama, Japan, Kasukabe Municipal Hospital, Saitama, Japan, and TMG Asaka Medical center, Saitama, Japan. We included consecutive MI patients that had been admitted to a total of six hospitals and underwent coronary angiography (CAG) between April 7, 2019 and April 6, 2021 (n = 781). All patients included in the study were admitted within 30 days of the MI symptom onset. The patients included were identified through a review of the records of consecutive patients admitted for MIs, and all had consented by the opt-out method to the use of their data for study purposes.
Because a state of emergency declaration for COVID-19 in Japan on April 7, 2020, was proposed in the Tokyo, Saitama, Chiba, Kanagawa, Osaka, Hyogo, and Fukuoka prefectures, we defined the patients who suffered from MIs from April 7, 2020 to April 6, 2021 as the after-pandemic period group. We defined the MI patients who suffered from MIs from April 7, 2019 to April 6, 2020 as the pre-pandemic period group.
The study protocol was approved by the Ethics Committee of Nihon University Itabashi Hospital (RK-210914-15) and was in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Data collection and definitions
Information from the patients’ clinical records was entered anonymously into an Excel spreadsheet conducted by physicians or the clinical research coordinator at the 6 Japanese multicenter medical institutions as mentioned above. The MIs were diagnosed on the basis of the European Society of Cardiology (ESC)/American College of Cardiology (ACC) Foundation/American Heart Association/World Heart Federation Task Force for the Universal Definition of Myocardial Infarction [7]. The MIs were classified as STEMIs or NSTEMIs, depending on the presence or absence of ST-segment elevation at the J point in at least 2 continuous leads or a new left bundle branch block pattern [8]. The MIs were also classified as AMIs or recent MIs (RMIs), depending on the time from the symptom onset to the diagnosis, whether < 24 h or 24 h to 30 days, respectively [9]. Echocardiography was performed at the time of admission. The following cardiovascular risk factors were assessed as previously reported [10]. Heart failure, if present at the time of the initial presentation, was classified by the severity according to the Killip classification [11]. The definition of the TIMI flow was graded as TIMI 0 = no perfusion, TIMI 1 = penetration without perfusion, TIMI 2 = partial perfusion, and TIMI 3 = complete perfusion, as described for the Phase I TIMI Trial [12]. If the percutaneous coronary intervention (PCI) was performed during the same session as the index CAG, it was defined as an ad hoc PCI, and especially for STEMIs, an ad-hoc PCI as the primary reperfusion strategy for AMIs without previous or concomitant thrombolytic therapy was defined as a primary PCI [13]. The symptom-to-admission time (STAT) was defined as the time from the symptom onset of the MI to admission. The admission-to-CAG time was defined as the time from the admission to entering the catheterization room to perform the CAG. The door-to-balloon time (DTBT) was evaluated as the time between admission and the time of the first balloon inflation or first manual thrombus aspiration in the patients who underwent a primary PCI. The type of presenting symptoms of the MIs upon admission was classified into typical symptoms, atypical symptoms, and out-of-hospital cardiac arrests (OHCAs). Typical symptoms were defined as any symptoms of chest pain or pressure with/without radiating to the arm, shoulder, neck, or jaw. Atypical symptoms were defined as any symptoms due to myocardial ischemia other than typical symptoms, including shortness of breath, nausea, abdominal pain, and loss of consciousness [14]. If the patients had a cardiopulmonary arrest at admission, it was defined as an OHCA.
Evaluations and study endpoints
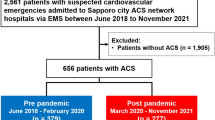
The study flowchart is shown in Fig. 1. We first divided the total 781 MI patients into STEMIs (n = 495) and NSTEMIs (n = 286). Second, both the STEMI and NSTEMI patients were divided into 2 time periods: those who were admitted between April 7, 2020 and April 6, 2021 (after-pandemic period, STEMI; n = 231, NSTEMI; n = 140) and those between April 7, 2019 and April 6, 2020 (pre-pandemic group, STEMI; n = 264, NSTEMI; n = 146). Then, we investigated the number of MI, STEMI, and NSTEMI inpatients between the two time periods. Next, we investigated the STEMI and NSTEMI patients separately, and compared the patient characteristics and mid-term outcomes between the two time periods, for both STEMIs and NSTEMIs, respectively.
The main study endpoint was the 180-day mortality, defined as deaths from any cause within 180 days after admission, which was ascertained through our review of the patient data. Thus, we compared the 180-day mortality between the after-pandemic period and pre-pandemic period, for both STEMIs and NSTEMIs, separately.
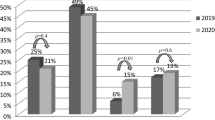
Screening tests and medical treatment of patients suspected of having MIs, whose COVID-19 could not be excluded, at 6 Japanese medical institutions
The 6 Japanese multicenter medical institutions participating in this study were affiliated hospitals and worked together daily to share the system of medical treatment. The flowchart of the MI treatment during the after-pandemic period has been updated day by day and our medical flowchart has been reported previously [6]. The temporal trend in the screening tests and medical treatment of patients suspected of having MIs at the 6 medical institutions after the after-pandemic period is shown in Fig. 2. Since April 7, 2020, medical history interviews regarding COVID-19, chest computed tomography (CT), and medical treatment with full personal protective equipment (PPE) have been performed in all 6 medical institutions. Antigen and/or polymerase chain reaction (PCR) tests for COVID-19 have been performed at Nihon University School of Medicine and Rinkai Hospital since May 2020, Kasukabe Municipal Hospital and TMG Asaka Medical Center since June 2020, and Nihon University Hospital and Kawaguchi Municipal Medical Center since December 2020, respectively.
Time trend for the screening tests and medical treatment in the patients suspected of having MIs and in whom COVID-19 could not be excluded, at 6 Japanese medical institutions. COVID-19, coronavirus disease 2019; CT, computed tomography; MIs, myocardial infarctions; PCR, polymerase chain reaction; PPE, personal protective equipment
Statistical analysis
Continuous variables are shown as the mean ± SD values, and the differences between groups were analyzed by a Student’s t test or Mann–Whitney U test. Categorical variables were shown as the number and percentage of patients, and the between-group differences in those variables were analyzed by a chi-square or Fisher’s exact test. The 180-day mortality among the patients compared between the two time periods was estimated by the Kaplan–Meier method, and the between-group differences were assessed by a log-rank test. All analyses were performed with SPSS Statistics 19.0 software (SPSS Inc., Chicago, IL, USA), and a P < 0.05 was considered significant.
Results
Comparison of the MI inpatients between the after-pandemic period and pre-pandemic period
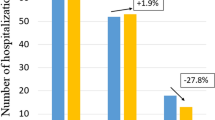
In the after-pandemic period, there was a 9.5% reduction in MI inpatients, 12.5% reduction in STEMIs, and 4.1% reduction in NSTEMIs (Fig. 3).
Number of MIs, STEMIs, and NSTEMIs inpatients between the after-pandemic period and pre-pandemic period. In the after-pandemic pandemic, there was a 9.5% reduction in the MI, 12.5% reduction in the STEMI, and 4.1% reduction in the NSTEMI inpatients, respectively. MI, myocardial infarction; NSTEMI, non ST-segment elevation myocardial infarction; STEMI, ST-segment elevation myocardial infarction
The enforcement rates of antigen and/or PCR tests for COVID-19 in the after-pandemic period at 6 Japanese medical institutions
The enforcement rates of antigen and/or PCR tests for COVID-19 at 6 Japanese medical institutions are shown in Fig. 4. They were 76.6% for Nihon University School of Medicine, 27.3% for Nihon University Hospital, 92.5% for Tokyo Rinkai Hospital, 25.4% for Kawaguchi City Medical Center, 71.7% for Kasukabe Municipal Hospital, and 78.3% for TMG Asaka Medical Center, respectively.
Patient characteristics between the after-pandemic period and pre-pandemic period in both the STEMI and NSTEMI patients
The clinical characteristics, symptom presentations, CAG findings, therapeutic interventions, medications at discharge, and time course of the treatment are summarized in Table 1. For the STEMIs, the age was significantly older (69.3 ± 12.2 vs. 66.7 ± 13.3 years, p = 0.025), rate of OHCAs numerically higher (12.1% vs. 8.0%, p = 0.30), and lactate level significantly lower (1.7 [interquartile range [IQR]: 1.3–2.2] vs. 2.0 [IQR: 1.5–3.0] mmol/L, p = 0.046), in the after-pandemic period than the pre-pandemic period, but not for NSTEMIs. For the NSTEMIs, culprit vessels involving the left main trunk (LMT) were significantly greater (6.1% vs. 0.8%, p = 0.036) and rate of a pre-TIMI grade 3 lesser (17.6% vs. 31.0%, p = 0.029) in the after-pandemic period than the pre-pandemic period, but not for STEMIs. For both the STEMIs and NSTEMIs, the use of mechanical ventilation was significantly greater in the after-pandemic period than the pre-pandemic period (STEMIs: 20.3% vs. 13.6%, p = 0.046, and NSTEMIs: 17.9% vs. 9.6%, p = 0.042); however, the use of non-invasive positive pressure ventilation was numerically lesser in the after-pandemic period. The STAT was numerically (but not significantly) longer in the after-pandemic period than the pre-pandemic period for both STEMIs (145.0 [IQR: 70.0–286.7] minutes vs. 130.0 [IQR: 75.0–254.3] minutes, p = 0.50) and NSTEMIs (330.0 [IQR: 190.3–636.7] minutes vs. 257.0 [IQR: 143.0–471.0] minutes, p = 0.43). The admission-to-CAG time (53.0 [IQR: 39.0–74.0] minutes vs. 41.0 [IQR: 30.0–58.3] minutes, p < 0.001) and DTBT (83.0 [IQR: 67.0–100.7] min vs. 70.0 [IQR: 59.0–88.7] min, p = 0.004) for STEMIs were significantly longer in the after-pandemic period than the pre-pandemic period.
Comparison of the mortality within 180 days between the after-pandemic period and pre-pandemic period
During the follow-up period (138.3 ± 69.3 days), a total of 89 patients with MIs died. For the STEMIs, the incidence of mortality was numerically greater in the after-pandemic period than the pre-pandemic period (30 days: 14.9% vs. 9.6%, and 180 days: 15.9% vs. 11.4%), but was not statistically significant (p = 0.14 by log-rank test) (Fig. 5). For the NSTEMIs, the incidence of mortality did not significantly differ between the two time periods (30 days: 6.6% vs. 6.4%, and 180 days: 9.9% vs. 8.0%, p = 0.59 by log-rank test).
Kaplan–Meier curves for the 180-day mortality in patients with STEMIs and NSTEMIs between the after-pandemic period and pre-pandemic period, respectively. The incidence of mortality did not significantly differ between the two time periods for both STEMIs (30 days: 14.9% vs. 9.6%, and 180 days: 15.9% vs. 11.4%, p = 0.14 by a log-rank test) and NSTEMIs (30 days: 6.6% vs. 6.4%, and 180 days: 9.9% vs. 8.0%, p = 0.59 by a log-rank test). NSTEMI, non ST-segment elevation myocardial infarction; STEMI, ST-segment elevation myocardial infarction
Discussion
The major findings in the present study were as follows: (1) there was a 9.5% reduction in hospitalizations among the MI patients in the after-pandemic period in a Japanese multi-center registry, (2) in those with STEMIs, the DTBT was significantly longer in the after-pandemic period than the pre-pandemic period, (3) in terms of the symptom presentation, the rate of OHCAs was numerically higher in the after-pandemic period in the STEMI patients but did not differ in the NSTEMI patients, (4) the 180-day mortality for both those with STEMIs and NSTEMIs did not significantly different between the after-pandemic period and pre-pandemic period. This study disclosed the impact of the COVID-19 pandemic on hospitalizations and the mid-term outcomes in patients with MIs in a Japanese multi-center registry, by performing an annual comparison at the multi-centers. To our knowledge, this is the first report to have focused on the mid-term outcomes between the after-pandemic period and pre-pandemic period in both STEMI and NSTEMI patients.
This multi-center study indicated a reduction in MI inpatients (MI: 9.5%, STEMI: 12.5%, NSTEMI: 4.1%) in the after-pandemic period as compared to the pre-pandemic period, which was consistent with the findings of previous Japanese reports (STEMI: 10.7%) [4]. The effect of the COVID-19 pandemic on MI hospitalizations might be multifactorial, such as the fear of contracting COVID-19 and a low physical stress due to stay-at-home orders [15, 16]. The rate of OHCAs in STEMI patients has increased after the COVID-19 pandemic, and there is concern that the number of hospitalizations will decrease due to sudden death in patients who conventionally visit the hospital [17]. Similar to this report, the present study showed that the STEMI patients with OHCAs were numerically greater in the after-pandemic period than the pre-pandemic period.
In the present study, the DTBT was significantly longer and 180-day mortality numerically (but not significantly) greater in the after-pandemic period than the pre-pandemic period, which was consistent with the previous Japanese reports [3,4,5]. On the other hand, the results outside of Japan have shown an increase in the mortality from AMIs in the after-pandemic period [18,19,20]. The reason could be considered to be that the STATs of AMIs and the enforcement rate of a primary PCI differed between our study and the other countries [20, 21]. In an observational study in China, the pre-hospital and in-hospital treatment times for STEMIs after the COVID-19 pandemic were significantly longer than those before, which resulted in a mortality increase [20]. In an observational study in Egypt, the volume of primary PCIs decreased at 80% of the centers [21]. In the present study, the enforcement rate of a primary PCI (97.8% vs. 98.5%, p = 0.74) and STATs were maintained in the after-pandemic period, which might be related to the lack of significant differences in the mid-term outcomes between the two time periods. Kobayashi S et.al suggested that chest CT for screening for COVID-19 before a primary PCI is significantly associated with a longer DTBT, but is not associated with the short-term outcomes [3]. Furthermore, in the present study, the longer DTBT in the after-pandemic period might be also considered to be due in part to the effect that the patients who would have been conventionally treated with non-invasive ventilation (NPPV) in the pre-pandemic period underwent tracheal intubation for fear of increasing the aerosol dispersion by the NPPV. The prognostic benefit of shortening the DTBT is reported to be limited to when it is within 2 h of the symptom onset [22]. In the present study, the longer DTBT in the after-pandemic period might not have affected the mid-term outcomes, because the median STATs were more than 2 h. Those findings suggest that although the DTBT will be extended by both chest CT to screen for COVID-19 and an increase in ventilator use in the after-pandemic period, it is important to prevent an increase in the mortality by performing infection prevention measures with full PPE assuming a COVID-19 infection and maintaining the enforcement of a primary PCI.
We reported in a previous report that the 30-day mortality of NSTEMIs was significantly greater during the COVID-19 period than control period [6]. In that previous study, the STATs of NSTEMIs were significantly longer (COVID-19 period vs. control period: 426.2 vs. 197.7 min, p = 0.011), and the admission-to-CAG time tended to be longer during the COVID-19 period (463.3 vs. 136.2 min, p = 0.11), which may also have resulted in an increase in the 30-day mortality. It was speculated that the fear of contracting COVID-19 could have made patients with MIs afraid to seek acute cardiac treatment. Patients misinterpreting MI symptoms, such as atypical symptoms, which are sometimes similar to COVID-19-related symptoms, might have interfered with an early diagnosis of an MI by choosing home recuperation [15]. In general, atypical symptoms in MI patients are reported to have a longer time-to-admission and reperfusion, and higher short-term mortality [14, 23]. However, in the present study, there was no significant difference in the rate of symptom presentation and STATs in the NSTEMI patients between the after-pandemic period and pre-pandemic period, which might result in no difference in the 180-day mortality between the two time periods. To reduce the mortality of NSTEMIs, we updated the clinical flowchart of the MIs reported in the previous report [6].
Our study had several limitations. First, although WHO declared the pandemic on 11 March 2020, we defined the pandemic period in the present study as starting April 7, 2020, when a state of emergency declaration for COVID-19 in Japan was proposed. Therefore, the indirect effects of the COVID-19 pandemic could have already been reflected in the latter pre-pandemic period, and it might be possible that the effects of the COVID-19 pandemic were underestimated. Second, the timing of the initiation and enforcement rate of antigen and/or PCR tests for COVID-19 varied among the 6 Japanese medical institutions in the present study, which might have affected the time course and outcomes in the present study. Third, for both STEMIs and NSTEMIs, the patient background was not exactly the same between the two time periods, so other factors beyond the COVID-19 pandemic could have affected the 180-day mortality. Finally, the observation period was 180 days, and thus the long-term outcomes were not evaluated. However, in this multi-center retrospective study, the two limitations of our previous study, that is (1) a single-center and (2) semi-annual comparison before and after the COVID-19 pandemic, were overcome by being performed at multi-centers and carrying out an annual comparison [6].
Conclusions
This study demonstrated the indirect effects of the COVID-19 pandemic on MIs in a Japanese multi-center registry for both STEMIs and NSTEMIs, by comparing 1 year before with 1 year after the COVID-19 pandemic. In the STEMIs, although the age was older, the DTBT longer, and rate of OCHAs numerically greater in the after-pandemic period, the enforcement rate of a primary PCI and the mid-term outcomes were maintained at the same level as that in the pre-pandemic period. For NSTEMIs, the mid-term outcome was maintained at the same level without any delay from the onset to the treatment even in the after-pandemic period. These findings suggested that it is important to attempt to encourage MI patients to visit the hospital, and to ensure that the treatment is not delayed after admission even during the COVID-19 pandemic.
Abbreviations
- AMI:
-
Acute myocardial infarction
- CABG:
-
Coronary artery bypass graft
- CAG:
-
Coronary angiography
- CK:
-
Creatine kinase
- COVID-19:
-
Coronavirus disease 2019
- CVIT:
-
Cardiovascular intervention and therapeutics
- DTBT:
-
Door-to-balloon time
- ECG:
-
Electrocardiography
- IABP:
-
Intra-aortic balloon pump
- JCS:
-
Japanese circulation society
- MI:
-
Myocardial infarction
- NSTEMI:
-
Non-ST elevation myocardial infarction
- LMT:
-
Left main trunk
- OHCA:
-
Out of hospital cardiac arrest
- PCI:
-
Percutaneous coronary intervention
- POBA:
-
Plain old balloon angioplasty
- PPE:
-
Personal protective equipment
- RMI:
-
Recent myocardial infarction
- STAT:
-
Symptom-to-admission time
- STEMI:
-
ST elevation myocardial infarction
- TIMI:
-
Thrombolysis in myocardial infarction
- VA-ECMO:
-
Veno-arterial extracorporeal membrane oxygenation
- WHO:
-
World Health Organization
References
The Japanese association of cardiovascular intervention and therapeutics (CVIT) (2020) Recommendations for cardiac catheterization and treatment under the spread of coronavirus infection. URL: http://www.cvit.jp/files/news/2020/0413.pdf Accessed Dec 3.
The Japanese circulation society (JCS) (2020) COVID-19 Recommendations for maintaining the cardiovascular medical system during the epidemic. URL: https://www.j-circ.or.jp/cms/wp-content/uploads/2020/04/COVID-19 Accessed Dec 3.
Kobayashi S, Sakakura K, Jinnouchi H, Taniguchi Y, Tsukui T, Watanabe Y, Yamamoto K, Seguchi M, Wada H, Fujita H (2022) Comparison of door-to-balloon time and in-hospital outcomes in patients with ST-elevation myocardial infarction between before versus after COVID-19 pandemic. Cardiovasc Interv Ther. https://doi.org/10.1007/s12928-022-00836-4
Watanabe Y, Miyachi H, Mozawa K, Yamada K, Oka E, Shiomura R, Sugizaki Y, Matsuda J, Nakata J, Tara S, Tokita Y, Iwasaki YK, Yamamoto T, Takano H, Shimizu W (2021) Impact of the COVID-19 pandemic on ST-elevation myocardial infarction from a single-center experience in Tokyo. Intern Med 60:3693–3700
Matsubara Y, Izumikawa T, Washimi S, Yamada T, Hashimoto S, Taniguchi N, Nakajima S, Hata T, Takahashi A (2021) Impact of the SARS-CoV-2 pandemic on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction. Int Heart J 62:1230–1234
Arai R, Fukamachi D, Ebuchi Y, Migita S, Morikawa T, Monden M, Takei N, Tamaki T, Kojima K, Akutsu N, Murata N, Kitano D, Okumura Y (2021) Impact of the COVID-19 outbreak on hospitalizations and outcomes in patients with acute myocardial infarction in a Japanese single center. Heart Vessels 36(10):1474–1483
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA (2018) White HD (2018) fourth universal definition of myocardial infarction. Circulation 138:e618–e651
Kimura K, Kimura T, Ishihara M, Nakagawa Y, Nakao K, Miyauchi K, Sakamoto T, Tsujita K, Hagiwara N, Miyazaki S, Ako J, Arai H, Ishii H, Origuchi H, Shimizu W, Takemura H, Tahara Y, Morino Y, Iino K, Itoh T, Iwanaga Y, Uchida K, Endo H, Kongoji K, Sakamoto K, Shiomi H, Shimohama T, Suzuki A, Takahashi J, Takeuchi I, Tanaka A, Tamura T, Nakashima T, Noguchi T, Fukamachi D, Mizuno T, Yamaguchi J, Yodogawa K, Kosuge M, Kohsaka S, Yoshino H, Yasuda S, Shimokawa H, Hirayama A, Akasaka T, Haze K, Ogawa H, Tsutsui H, Yamazaki T (2019) JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ J 83(5):1085–1196
Arai R, Fukamachi D, Ebuchi Y, Migita S, Morikawa T, Monden M, Tamaki T, Kojima K, Akutsu N, Murata N, Kitano D, Okumura Y (2021) Mechanical complications of myocardial infarction. Int Heart J 62:499–509
Arai R, Suzuki S, Semba H, Arita T, Yagi N, Otsuka T, Sagara K, Sasaki K, Kano H, Matsuno S, Kato Y, Uejima T, Oikawa Y, Kunihara T, Yajima J, Yamashita T (2018) The predictive role of E/e’ on ischemic stroke and atrial fibrillation in Japanese patients without atrial fibrillation. J Cardiol 72:33–41
Killip T 3rd, Kimball JT (1967) Treatment of myocardial infarction in a coronary care unit. a two year experience with 250 patients. Am J Cardiol 20:457–464
Chesebro JH, Knatterud G, Roberts R, Borer J, Cohen LS, Dalen J, Dodge HT, Francis CK, Hillis D, Ludbrook P et al (1987) Thrombolysis in myocardial infarction (TIMI) trial, phase i: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clin Find Through Hosp Disch Circul 76:142–154
Keeley EC, Boura JA, Grines CL (2003) Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 361:13–20
Nakahashi T, Sakata K, Masuda J, Kumagai N, Higuma T, Ogimoto A, Tanigawa T, Hanada H, Nakamura M, Takamura M, Dohi K (2021) Comparison of door-to-balloon time and 30-day mortality according to symptom presentation in patients with acute myocardial infarction. Circ Rep 3:194–200
Mohammad MA, Koul S, Olivecrona GK, Gӧtberg M, Tydén P, Rydberg E, Scherstén F, Alfredsson J, Vasko P, Omerovic E, Angerås O, Fröbert O, Calais F, Völz S, Ulvenstam A, Venetsanos D, Yndigegn T, Oldgren J, Sarno G, Grimfjärd P, Persson J, Witt N, Ostenfeld E, Lindahl B, James SK, Erlinge D (2020) Incidence and outcome of myocardial infarction treated with percutaneous coronary intervention during COVID-19 pandemic. Heart 106(23):1812–1818
Limbers CA, McCollum C, Greenwood E (2020) Physical activity moderates the association between parenting stress and quality of life in working mothers during the COVID-19 pandemic. Ment Health Phys Act 19:100358
Rashid Hons M, Gale Hons CP, Curzen Hons N, Ludman Hons P, De Belder HM, Timmis Hons A, Mohamed Hons MO, Lüscher Hons TF, Hains Hons J, Wu J, Shoaib A, Kontopantelis E, Roebuck C, Denwood T, Deanfield J, Mamas MA (2020) Impact of coronavirus disease 2019 pandemic on the incidence and management of out-of-hospital cardiac arrest in patients presenting with acute myocardial infarction in England. J Am Heart Assoc 9:e018379
Song C, Liu S, Yin D, Wang Y, Zhao Y, Yang W, Qiao S, Dou K, Xu B (2020) Impact of public health emergency response to COVID-19 on management and outcome for stemi patients in beijing-a single-center historic control study. Curr Probl Cardiol 46(3):100693
De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C (2020) Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 41:2083–2088
Fu XY, Shen XF, Cheng YR, Zhou MY, Ye L, Feng ZH, Xu Z, Chen J, Wang MW, Zhang XW (2020) Effect of COVID-19 outbreak on the treatment time of patients with acute ST-segment elevation myocardial infarction. Am J Emerg Med 44:192–197
Mahmoud SED, Etriby SE, Etriby AE, Ghalib A (2020) Management trends in the cath lab during the COVID-19 period, an egyptian survey. Curr Probl Cardiol 46(3):100715
Shiomi H, Nakagawa Y, Morimoto T, Furukawa Y, Nakano A, Shirai S, Taniguchi R, Yamaji K, Nagao K, Suyama T, Mitsuoka H, Araki M, Takashima H, Mizoguchi T, Eisawa H, Sugiyama S, Kimura T (2012) Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ 344:e3257
Ito R, Yamashita J, Chikamori T, Kondo S, Mitsuhashi Y, Iwata H, Saji M, Asano T, Wakabayashi K, Yahagi K, Shinke T, Mase T, Abe K, Miyachi H, Higuchi S, Kishi M, Tanaka H, Yamasaki M, Miyauchi K, Yamamoto T, Nagao K, Takayama M (2020) Clinical differences of recent myocardial infarction compared with acute myocardial infarction—insights from the tokyo CCU network multicenter registry. Circ J 84:1511–1518
Acknowledgements
We thank Mr. John Martin for his help in reporting our findings in English.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interests.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Nihon University Itabashi Hospital (RK-210914–15).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arai, R., Nobuhiro, M., Kojima, K. et al. Impact of the COVID-19 pandemic on the hospitalizations, time course, presenting symptoms, and mid-term outcomes in patients with myocardial infarctions in a Japanese multi-center registry. Heart Vessels 38, 459–469 (2023). https://doi.org/10.1007/s00380-022-02183-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02183-z