Abstract
Background
Although glucose variability (GV) is reportedly associated with coronary plaque vulnerability, namely lipid-rich plaque, details are not fully understood. The aim of this study was to evaluate relations of GV after discharge to vulnerable plaque formation assessed by near-infrared spectroscopy intravascular ultrasound (NIRS-IVUS) in patients with and without diabetes.
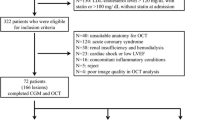
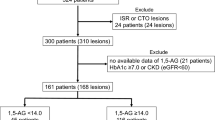
Methods
A total of 40 patients undergoing percutaneous coronary intervention under NIRS-IVUS guidance were included, among whom 13 (33%) had diabetes and 20 (50%) presented with acute myocardial infarction (MI). GV was evaluated by a flush glucose monitoring system, primarily with mean amplitude of glycemic excursion (MAGE). Lipid-rich plaque was assessed by maximum lipid core burden index in 4 mm (maxLCBI4mm) in the target lesion using NIRS-IVUS.
Results
Mean MAGE and maxLCBI4mm were 69.7 ± 25.6 mg/dl and 508.0 ± 294.9. Intra-day GV was not significantly associated with maxLCBI4mm in the entire study population, while MAGE was correlated with maxLCBI4mm in non-diabetic patients (r = 0.46, p = 0.02). In patients with and without acute MI presentation, no significant relations were found between MAGE and maxLCBI4mm.
Conclusion
GV was associated with lipid core plaque formation, especially in non-diabetic patients.



Similar content being viewed by others
References
Nallamothu BK, Normand SL, Wang Y, Hofer TP, Brush JE Jr, Messenger JC, Bradley EH, Rumsfeld JS, Krumholz HM (2015) Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet 385:1114–1122
Ozaki Y, Katagiri Y, Onuma Y, Amano T, Muramatsu T, Kozuma K, Otsuji S, Ueno T, Shiode N, Kawai K, Tanaka N, Ueda K, Akasaka T, Hanaoka KI et al (2018) CVIT expert consensus document on primary percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) in 2018. Cardiovasc Interv Ther 33:178–203
GBD (2013) Mortality and Causes of Death Collaborators (2015) Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385:117–171
Bom MJ, van der Heijden DJ, Kedhi E, van der Heyden J, Meuwissen M, Knaapen P, Timmer SAJ, van Royen N (2017) Early detection and treatment of the vulnerable coronary plaque: can we prevent acute coronary syndromes? Circ Cardiovasc Imaging 10:e005973
Pasterkamp G, den Ruijter HM, Libby P (2017) Temporal shifts in clinical presentation and underlying mechanisms of atherosclerotic disease. Nat Rev Cardiol 14:21–29
Amano T, Matsubara T, Uetani T, Nanki M, Marui N, Kato M, Yoshida T, Arai K, Yokoi K, Ando H, Kumagai S, Ishii H, Izawa H, Hotta N, Murohara T (2008) Abnormal glucose regulation is associated with lipid-rich coronary plaque: relationship to insulin resistance. JACC Cardiovasc Imaging 1:39–45
Inaba S, Okayama H, Funada J, Higashi H, Saito M, Yoshii T, Hiasa G, Sumimoto T, Takata Y, Nishimura K, Inoue K, Ogimoto A, Higaki J (2012) Impact of type 2 diabetes on serial changes in tissue characteristics of coronary plaques: an integrated backscatter intravascular ultrasound analysis. Eur Heart J Cardiovasc Imaging 13:717–723
Kuroda M, Shinke T, Sakaguchi K, Otake H, Takaya T, Hirota Y, Sugiyama D, Nakagawa M, Hariki H, Inoue T, Osue T, Taniguchi Y, Iwasaki M, Nishio R, Kinutani H, Konishi A, Hiranuma N, Takahashi H, Terashita D, Hirata KI (2015) Effect of daily glucose fluctuation on coronary plaque vulnerability in patients pre-treated with lipid-lowering therapy: a prospective observational study. JACC Cardiovasc Interv 8:800–811
Okada K, Hibi K, Gohbara M, Kataoka S, Takano K, Akiyama E, Matsuzawa Y, Saka K, Maejima N, Endo M, Iwahashi N, Tsukahara K, Kosuge M, Ebina T, Fitzgerald PJ, Honda Y, Umemura S, Kimura K (2015) Association between blood glucose variability and coronary plaque instability in patients with acute coronary syndromes. Cardiovasc Diabetol 14:111
Gohbara M, Hibi K, Mitsuhashi T, Maejima N, Iwahashi N, Kataoka S, Akiyama E, Tsukahara K, Kosuge M, Ebina T, Umemura S, Kimura K (2016) Glycemic variability on continuous glucose monitoring system correlates with non-culprit vessel coronary plaque vulnerability in patients with first-episode acute coronary syndrome - optical coherence tomography study. Circ J 80:202–210
Gardner CM, Tan H, Hull EL, Lisauskas JB, Sum ST, Meese TM, Jiang C, Madden SP, Caplan JD, Burke AP, Virmani R, Goldstein J, Muller JE (2008) Detection of lipid core coronary plaques in autopsy specimens with a novel catheter-based near-infrared spectroscopy system. JACC Cardiovasc Imaging 1:638–648
Mori N, Saito Y, Saito K, Matsuoka T, Tateishi K, Kadohira T, Kitahara H, Fujimoto Y, Kobayashi Y (2020) Relation of plasma xanthine oxidoreductase activity to coronary lipid core plaques assessed by near-infrared spectroscopy intravascular ultrasound in patients with stable coronary artery disease. Am J Cardiol 125:1006–1012
Tateishi K, Kitahara H, Saito Y, Kadohira T, Saito K, Matsuoka T, Mori N, Nakayama T, Fujimoto Y, Kobayashi Y (2021) Impact of clinical presentations on lipid core plaque assessed by near-infrared spectroscopy intravascular ultrasound. Int J Cardiovasc Imaging 37:1151–1158
Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R (2016) Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet 388:2254–2263
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction (2018) Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol 72:2231–2264
Suzuki N, Asano T, Nakazawa G, Aoki J, Tanabe K, Hibi K, Ikari Y, Kozuma K (2020) Clinical expert consensus document on quantitative coronary angiography from the Japanese Association of Cardiovascular Intervention and Therapeutics. Cardiovasc Interv Ther 35:105–116
Saito Y, Mori N, Murase T, Nakamura T, Akari S, Saito K, Matsuoka T, Tateishi K, Kadohira T, Kitahara H, Fujimoto Y, Kobayashi Y (2021) Greater coronary lipid core plaque assessed by near-infrared spectroscopy intravascular ultrasound in patients with elevated xanthine oxidoreductase: a mechanistic insight. Heart Vessels 36:597–604
Saito Y, Kobayashi Y, Fujii K, Sonoda S, Tsujita K, Hibi K, Morino Y, Okura H, Ikari Y, Honye J (2022) Clinical expert consensus document on intravascular ultrasound from the Japanese Association of Cardiovascular Intervention and Therapeutics (2021). Cardiovasc Interv Ther 37:40–51
Sonoda S, Hibi K, Okura H, Fujii K, Honda Y, Kobayashi Y (2020) Current clinical use of intravascular ultrasound imaging to guide percutaneous coronary interventions. Cardiovasc Interv Ther 35:30–36
Mintz GS (2020) Intravascular ultrasound guidance improves patient survival (mortality) after drug-eluting stent implantation: review and updated bibliography. Cardiovasc Interv Ther 35:37–43
American Diabetes Association (2020) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care 43:S14–S31
Kovatchev B, Cobelli C (2016) Glucose variability: timing, risk analysis, and relationship to hypoglycemia in diabetes. Diabetes Care 39:502–510
Battelino T, Danne T, Bergenstal RM, Amiel SA, Beck R, Biester T, Bosi E, Buckingham BA, Cefalu WT, Close KL, Cobelli C, Dassau E, DeVries JH, Donaghue KC, Dovc K, Doyle FJ 3rd, Garg S, Grunberger G, Heller S, Heinemann L, Hirsch IB, Hovorka R, Jia W, Kordonouri O, Kovatchev B, Kowalski A, Laffel L, Levine B, Mayorov A, Mathieu C, Murphy HR, Nimri R, Nørgaard K, Parkin CG, Renard E, Rodbard D, Saboo B, Schatz D, Stoner K, Urakami T, Weinzimer SA, Phillip M (2019) Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care 42:1593–1603
Zhou Z, Sun B, Huang S, Zhu C, Bian M (2020) Glycemic variability: adverse clinical outcomes and how to improve it? Cardiovasc Diabetol 19:102
EasyGV. http://www.phc.ox.ac.uk/research/diabetes/software/easygv. Accessed 22 Feb 2022.
Waksman R, Di Mario C, Torguson R, Ali ZA, Singh V, Skinner WH, Artis AK, Cate TT, Powers E, Kim C, Regar E, Wong SC, Lewis S, Wykrzykowska J, Dube S, Kazziha S, van der Ent M, Shah P, Craig PE, Zou Q, Kolm P, Brewer HB, Garcia-Garcia HM, Investigators LRP (2019) Identification of patients and plaques vulnerable to future coronary events with near-infrared spectroscopy intravascular ultrasound imaging: a prospective, cohort study. Lancet 394:1629–1637
Erlinge D, Maehara A, Ben-Yehuda O, Bøtker HE, Maeng M, Kjøller-Hansen L, Engstrøm T, Matsumura M, Crowley A, Dressler O, Mintz GS, Fröbert O, Persson J, Wiseth R, Larsen AI, Okkels Jensen L, Nordrehaug JE, Bleie Ø, Omerovic E, Held C, James SK, Ali ZA, Muller JE, Stone GW, Investigators PROSPECTII (2021) Identification of vulnerable plaques and patients by intracoronary near-infrared spectroscopy and ultrasound (PROSPECT II): a prospective natural history study. Lancet 397:985–995
Bailey T, Bode BW, Christiansen MP, Klaff LJ, Alva S (2015) The performance and usability of a factory-calibrated flash glucose monitoring system. Diabetes Technol Ther 17:787–794
Tateishi K, Saito Y, Kitahara H, Kobayashi Y (2022) Impact of glycemic variability on coronary and peripheral endothelial dysfunction in patients with coronary artery disease. J Cardiol 79:65–70
Ito T, Ichihashi T, Fujita H, Sugiura T, Yamamoto J, Kitada S, Nakasuka K, Kawada Y, Ohte N (2019) The impact of intraday glucose variability on coronary artery spasm in patients with dysglycemia. Heart Vessels 34:1250–1257
Ishihara M (2012) Acute hyperglycemia in patients with acute myocardial infarction. Circ J 76:563–571
Oswald GA, Corcoran S, Yudkin JS (1984) Prevalence and risks of hyperglycaemia and undiagnosed diabetes in patients with acute myocardial infarction. Lancet 1:1264–1267
Mi SH, Su G, Yang HX, Zhou Y, Tian L, Zhang T, Tao H (2017) Comparison of in-hospital glycemic variability and admission blood glucose in predicting short-term outcomes in non-diabetes patients with ST elevation myocardial infarction underwent percutaneous coronary intervention. Diabetol Metab Syndr 9:20
Pu Z, Lai L, Yang X, Wang Y, Dong P, Wang D, Xie Y, Han Z (2020) Acute glycemic variability on admission predicts the prognosis in hospitalized patients with coronary artery disease: a meta-analysis. Endocrine 67:526–534
Park SE, Lee BW, Kim JH, Lee WJ, Cho JH, Jung CH, Lee SH, Suh S, Hur GC, Kim SH, Jang YH et al (2017) Effect of gemigliptin on glycaemic variability in patients with type 2 diabetes (STABLE study). Diabetes Obes Metab 19:892–896
Lee S, Lee H, Kim Y, Kim E (2019) Effect of DPP-IV inhibitors on glycemic variability in patients with T2DM: a systematic review and meta-analysis. Sci Rep 9:13296
Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, Colette C (2006) Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 295:1681–1687
Teraguchi I, Imanishi T, Ozaki Y, Tanimoto T, Ueyama M, Orii M, Shiono Y, Shimamura K, Ishibashi K, Yamano T, Ino Y, Yamaguchi T, Hirata K, Kubo T, Sanke T, Akasaka T (2014) Acute-phase glucose fluctuation is negatively correlated with myocardial salvage after acute myocardial infarction. Circ J 78:170–179
Koska J, Saremi A, Howell S, Bahn G, De Courten B, Ginsberg H, Beisswenger PJ, Reaven PD, Investigators VADT (2018) Advanced glycation end products, oxidation products, and incident cardiovascular events in patients with type 2 diabetes. Diabetes Care 41:570–576
Giacco F, Brownlee M (2010) Oxidative stress and diabetic complications. Circ Res 107:1058–1070
Kataoka Y, Hosoda K, Makino H, Matsubara M, Matsuo M, Ohata Y, Koezuka R, Tamanaha T, Tomita T, Honda-Kohmo K, Noguchi M, Son C, Nishimura K, Asaumi Y, Miyamoto Y, Noguchi T, Yasuda S (2019) The efficacy of glycemic control with continuous glucose monitoring on atheroma progression: rationale and design of the Observation of Coronary Atheroma Progression under Continuous Glucose Monitoring Guidance in Patients with Type 2 Diabetes Mellitus (OPTIMAL). Cardiovasc Diagn Ther 9:431–438
Fujii K, Kubo T, Otake H, Nakazawa G, Sonoda S, Hibi K, Shinke T, Kobayashi Y, Ikari Y, Akasaka T (2022) Expert consensus statement for quantitative measurement and morphological assessment of optical coherence tomography: update 2022. Cardiovasc Interv Ther. https://doi.org/10.1007/s12928-022-00845-3
Acknowledgements
We thank all of the hospital staff who assisted in data collection.
Funding
This study was funded by the Nipro Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yoshio Kobayashi has received research grants from the Nipro Corporation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tateishi, K., Saito, Y., Kitahara, H. et al. Relation of glucose variability to vulnerable plaque formation in patients with coronary artery disease. Heart Vessels 37, 1516–1525 (2022). https://doi.org/10.1007/s00380-022-02063-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02063-6