Abstract
Background
A low 1,5-anhydro-d-glucitol (AG) blood level is considered a clinical marker of postprandial hyperglycemia. Previous studies reported that 1,5-AG levels were associated with vascular endothelial dysfunction and coronary artery disease (CAD). However, the association between 1,5-AG levels and coronary artery plaque in patients with CAD is unclear.
Methods
This study included 161 patients who underwent percutaneous coronary intervention for CAD. The culprit plaque characteristics and the extent of coronary calcification, which was measured by the angle of its arc, were assessed by preintervention intravascular ultrasound (IVUS). Patients with chronic kidney disease or glycosylated hemoglobin ≥ 7.0 were excluded. Patients were divided into 2 groups according to serum 1,5-AG levels (< 14.0 μg/mL vs. ≥ 14 μg/mL).
Results
The total atheroma volume and the presence of IVUS-attenuated plaque in the culprit lesions were similar between groups. Calcified plaques were frequently observed in the low 1,5-AG group (p = 0.06). Compared with the high 1,5-AG group, the low 1,5-AG group had significantly higher median maximum calcification (144° vs. 107°, p = 0.03) and more frequent calcified plaques with a maximum calcification angle of ≥ 180° (34.0% vs. 13.2%, p = 0.003). Multivariate logistic regression analysis showed that a low 1,5-AG level was a significant predictor of a greater calcification angle (> 180°) (OR 2.64, 95% CI 1.10–6.29, p = 0.03).
Conclusions
Low 1,5-AG level, which indicated postprandial hyperglycemia, was associated with the severity of coronary artery calcification. Further studies are needed to clarify the effects of postprandial hyperglycemia on coronary artery calcification.
Similar content being viewed by others
Background
Type 2 diabetes mellitus (DM) is a complex disease that is related to atherosclerotic diseases. Patients with type 2 DM have a higher incidence of cardiovascular disease (CVD) compared with the general population [1, 2]. Increased glycosylated hemoglobin (HbA1c), which is a common marker of long-term glycemic control, had been associated with poor prognosis in patients with DM [3]. Moreover, previous studies demonstrated that postprandial hyperglycemia affected mortality and CVD progression [4,5,6]. 1,5-anhydro-d-glucitol (1,5-AG) is a naturally occurring 1-deoxy form of glucose and thought to originate in the diet [7]. Serum 1,5-AG levels have been known to rapidly decrease along with the excretion of glucose in the urine and were reported to better reflect short-term glucose control and postprandial hyperglycemia, compared with HbA1c levels [8, 9]. Some studies have shown that 1,5-AG levels were associated with vascular endothelial dysfunction [10] and superior to HbA1c in detecting the presence of CVD [11, 12]. Our colleagues demonstrated that low 1,5-AG levels predicted the long-term clinical outcomes in CVD patients with HbA1c levels < 7.0% [13, 14]. Therefore, 1,5-AG level might be a useful predictive marker in patients with relatively low HbA1c levels. However, the mechanisms of the relationship between CVD and 1,5-AG level are unclear. In this study, we sought to evaluate the association between 1,5-AG level and culprit coronary plaque findings, including quantitative and qualitative analyses by gray-scale intravascular ultrasound (IVUS), in patients with CVD who underwent percutaneous coronary intervention (PCI).
Methods
Study population
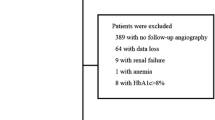
In this prospective, single-center, observational study, 324 consecutive coronary artery disease (CAD) patients who were admitted to Juntendo University Hospital were enrolled from August 2014 to August 2016 (Fig. 1). The inclusion criteria were (1) patients who underwent PCI under IVUS guidance to treat a de novo culprit lesion and (2) patients who were evaluated using IVUS. The exclusion criteria were (1) patients who had in-stent restenosis or a lesion with chronic total occlusion; (2) patients who had chronic kidney disease (CKD), which was defined as an estimated glomerular filtration rate of < 60 mL/min/1.73 m2 that was calculated using the Modification of Diet in Renal Disease equation, modified with a Japanese coefficient using baseline serum creatinine [15]; (3) patients who had HbA1c levels ≥ 7.0% and those under treatment with sodium-glucose co-transporter 2 inhibitors; and (4) patients in whom adequate IVUS images or data on 1,5-AG levels were not obtained. Patients were divided into 2 groups (low 1,5-AG group, < 14.0 µg/mL; high 1,5-AG group, ≥ 14.0 µg/mL).
Flow chart of the study inclusion IVUS analysis was performed in 324 patients between August 2014 and August 2016. A total of 161 patients (168 lesions) were enrolled. 1,5-AG 1,5-anhydro-d-glucitol, CKD chronic kidney disease, CTO chronic total occlusion, eGFR estimated glomerular filtration rate, ISR in-stent restenosis, IVUS intravascular ultrasound, PCI percutaneous coronary intervention
This study was approved by the Juntendo University ethics committee and was performed in accordance with the Declaration of Helsinki. All participants provided written, informed consent.
Data collection and blood sampling
Data on demographics, CAD risk factors, and medication use were collected from our institutional database. Blood samples were collected in the early morning after overnight fasting, and blood pressure (BP) was measured on admission. Patients with BP > 140/90 mmHg or those receiving antihypertensive drugs were regarded as hypertensive. Dyslipidemia was defined as low-density lipoprotein cholesterol ≥ 140 mg/dL, high-density lipoprotein cholesterol ≤ 40 mg/dL, triglycerides ≥ 150 mg/dL, or current treatment with statins and/or lipid-lowering agents [16]. DM was defined as either an HbA1c ≥ 6.5% or use of medications, such as insulin or oral hypoglycemic drugs. A current smoker was defined as a person who was a smoker at the time of PCI or who had quit smoking within 1 year before PCI. Acute coronary syndrome (ACS) was defined as acute myocardial infarction (MI) and unstable angina. Acute MI was characterized by elevated cardiac enzymes. Unstable angina was diagnosed in the presence of ischemic symptoms, without the elevation of the enzymes and biomarkers associated with myocardial necrosis.
To measure 1,5-AG levels, blood samples were obtained immediately prior to coronary angiography and stored at − 80 °C until measurement. Serum 1,5-AG levels were measured with a colorimetric method (Nippon Kayaku, Tokyo, Japan) using a Lana 1,5-AG auto liquid automatic analyzer (JCA-BM 8060, JEOL Ltd., Tokyo, Japan).
IVUS image acquisition and analysis
In all study patients, the culprit plaque lesion was evaluated by preintervention IVUS. By comparing pre- and post-PCI IVUS findings, a culprit lesion segment was defined as the lesion that was stented. In this study, the mechanical rotating 40-MHz transducer that was used were from 1 commercially available IVUS systems and catheters (Atlantis Pro2, Boston Scientific Corporation, Natick, MA, USA; View It, Terumo Corporation, Tokyo, Japan). After intracoronary administration of 0.1–0.2 mg nitroglycerin, IVUS imaging of the culprit lesion segment was performed before balloon dilatation or after small (1.5–2.0 mm) balloon dilatation. All IVUS pullback maneuvers were performed automatically at 0.5 mm/s. All measurements were fulfilled at the end of this study. Quantitative and qualitative IVUS analyses were performed according to the criteria of the American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies [17]. The morphological features were diagnosed by careful review of the IVUS images and upon the agreement of the 2 independent experienced cardiologists (H.W. and T.D.) who were blinded to the clinical data. Offline analyses of all imaged segments were performed using computerized planimetry software (QIVUS; Medis Medical Imaging System, Leiden, the Netherlands).
The quantitative IVUS measurements included the external elastic membrane (EEM), lumen cross-sectional area (CSA), and the plaque plus media CSA (EEM–lumen CSA). The plaque burden was calculated as the plaque plus media CSA divided by the lesion EEM CSA multiplied by 100. Total atheroma volume (TAV) was calculated as the sum of the differences between the EEM and the luminal areas across all segments analyzed. Percent atheroma volume was calculated as the proportion of the entire lesion segment occupied by the atherosclerotic plaque. The qualitative IVUS variables included plaque rupture (presence of a cavity that communicated with the lumen with an overlying residual fibrous cap); thrombus (an intraluminal mass, often with a layered, lobulated, or pedunculated appearance); calcification (brighter plaque than adventitia with acoustic shadowing); and ultrasound attenuation behind the plaque in the absence of calcification. The maximum angle of the ultrasound attenuation and the calcification of the lesion were also measured. The remodeling index was calculated as the EEM CSA at the minimal lumen area site divided by the average of the proximal and distal reference EEM CSA. A representative case is shown in Fig. 2.
Representative case of intravascular ultrasound-detected attenuated plaque. A 70-year-old man with stable coronary artery disease is shown to have severe coronary artery stenosis on angiography (A). Intravascular ultrasound examination B–F shows a severely calcified plaque (maximum calcification angle, 275°) in the proximal left descending artery (E). In this case, the serum 1,5-anhydro-d-glucitol level is 8.3 µg/mL
Statistical analysis
Quantitative data are presented as mean ± standard deviation (SD) or median [interquartile range (IQR)]. Categorical variables are presented as frequencies. Continuous variables were compared using unpaired t-test or the Mann–Whitney U-test, as appropriate. Categorical variables were compared using the Chi-square test. A logistic regression analysis was used to compare the odds ratios (ORs) of the calcified plaque (maximum calcified angle ≥ 180°) between 2 groups (low 1,5-AG and high 1,5-AG). Differences were considered significant at p < 0.05. Statistical analyses were carried out using JMP version 12.0 software (SAS Institute, Cary, NC, USA).
Results
Baseline patient clinical characteristics
In the 161 patients, the median and mean 1,5-AG were 17.6 (IQR 13.4, 23.3) and 18.6 ± 7.1, respectively; of these, 45 patients (28.0%) were assigned to the low 1,5-AG group. The baseline demographics are summarized in Table 1. The mean age of the patients was 64.9 years, 86.3% were men, and the rate of DM was 19.9%. Compared with the patients in the high 1,5-AG group, those in the low 1,5-AG group were more likely to have DM and have higher fasting blood glucose levels. On the other hand, there was no significant difference in the HbA1c levels between the low 1,5-AG and high 1,5-AG groups.
Quantitative and qualitative IVUS findings
A total of 168 culprit lesions were analyzed. The lesion-level findings on coronary angiography and IVUS are shown in Table 2. The overall median minimal lumen area, percentage atheroma volume, and remodeling index were 2.1 mm2, 60.8%, and 1.1, respectively. There were no significant differences in the quantitative parameters, such as plaque burden at the minimal lumen area, percent atheroma volume, total atheroma volume, and remodeling index between the low 1,5-AG and high 1,5-AG groups.
In the overall qualitative analysis, 37.5% and 17.3% of the plaques were described as soft and calcific, respectively. There was no significant difference in the culprit plaque type between the groups. Similarly, the frequency of plaque rupture and calcified nodules did not differ between the groups. The frequency of calcified lesion tended to be higher in the low 1,5-AG group than in the high 1,5-AG group (72.3% vs. 57.0%; p = 0.06); whereas the frequency of ultrasound attenuation was similar between the groups. The median maximum calcification angle was significantly higher in the low 1,5-AG group than in the high 1,5-AG group (144° vs. 107°, p = 0.03). Plaques with a maximum calcification angle of > 180° were more frequently observed in the low 1,5-AG group than in the high 1,5-AG group (34.0% vs. 13.2%; p = 0.01).
Multivariate logistic regression analysis
The univariate logistic regression analysis showed that low 1,5-AG level was significantly associated with a greater calcification angle (> 180°) (OR 3.39, 95% CI 1.52–7.60; p = 0.003). To determine the value of serum 1,5-AG, a multivariate logistic regression analysis was conducted. The variables for which the unadjusted p value was < 0.10 in the univariate analysis were included in the multivariate model for greater calcification angle. In the multivariate model (Table 3), the independent predictors of a greater calcification angle were low 1,5-AG level (adjusted OR 2.64, 95% confidence interval (CI) 1.10–6.29; p = 0.03) and the presence of diabetes (OR 2.99, 95% CI 1.20–7.33; p = 0.02).
Discussion
In the present study, the association between 1,5-AG level and culprit coronary plaque findings in CVD patients who underwent PCI was examined. The major findings of the present study were (1) compared with patients in the high 1,5-AG group, those in the low 1,5-AG group were more likely to have a higher fasting blood glucose levels despite similar HbA1c levels; (2) plaques with a maximum calcification angle of > 180° were more frequently observed in the low 1,5-AG group than in the high 1,5-AG group; and (3) low 1,5-AG level was an independent predictor of a greater calcification angle. Overall, our results showed that low 1,5-AG was associated with more severe plaque calcification, which is a discriminator of plaque atherosclerosis.
1,5-AG is a monosaccharide that can be primarily obtained from dietary sources. The concentrations of 1,5-AG in blood and tissues are maintained constant, because the amount filtered by the glomeruli is reabsorbed in the renal proximal tubule. Reabsorption is competitively inhibited by glucose. In the setting hyperglycemia, 1,5-AG is excreted in the urine, and its serum level decreases rapidly [7]. Therefore, serum 1,5-AG level is considered a clinical marker of short-term glycemic status. In addition, 1,5-AG had been reported to reflect glycemic excursions, often in the postprandial state, more robustly than HbA1c, in patients with moderately controlled DM [8]. No differences in 1,5-AG levels were found in patients with markedly different estimated glomerular filtration rates [18], and these levels were not influenced by administration of a gliptin compound [19]. Serum 1,5-AG concentration is a marker for hyperglycemia and may be particularly useful as an indicator for short-term glycemic excursions [20] and is significantly higher in DM patients [21]. Finally, 1,5-AG might suppress the blood glucose elevation through inhibition of sucrase and intestinal glucose absorption [22].
HbA1c is a well-known useful maker for the diagnosis of DM and glycemic control. Elevated HbA1c had been associated with increased risk of cardiovascular events [3, 23, 24], and a target of < 7.0% had been established by the American Diabetes Association [25]. However, despite the beneficial effects of lowering HbA1c level to < 7.0% on macrovascular disease, the risks for macrovascular complications remain [26, 27]. Accordingly, comprehensive evaluation, in addition to that of HbA1c, may be necessary for the prevention of macrovascular diseases, especially in patients with relatively low HbA1c levels.
Our colleagues have demonstrated that low 1,5-AG levels predicted the long-term clinical outcomes in both ACS and stable CAD patients with HbA1c levels < 7.0% [13, 14]. They considered that 1,5-AG, which detected postprandial hyperglycemia, may be a useful marker for risk stratification in CAD patients with HbA1c < 7.0%. In the present study, we showed that a lower 1,5-AG was associated with more severe plaque calcification, as detected by IVUS imaging. Interestingly, coronary atheroma volume or plaque burden were not significantly associated with serum 1,5-AG levels. Postprandial hyperglycemia might not affect plaque quantitative parameters among patients with relatively low HbA1c levels and preserved renal function. Coronary calcification had been recognized to be associated with atherosclerosis [28] and is an established predictor of future cardiac events [29,30,31]. Coronary artery calcification is generally related with the extent of CAD. In a histologic study, Sangiorgi et al. reported a significant association between coronary calcification area and plaque volume [32]. In addition, studies on IVUS and computed tomography (CT) showed an association between coronary artery calcification and extent of atherosclerosis plaque [33, 34]. Coronary artery calcification tended to be higher in patients with DM, correlated with total plaque burden, and was an independent risk factor for adverse cardiac events [34, 35]. Medial artery calcification, which is a non-obstructive condition leading to related artery compliance, is known a risk factor of future cardiovascular events among patients with DM [36]. Previous in vivo experiments reported that diabetes promote vascular calcification in part by recruiting adventitial cell with osteogenic potential [37]. So, osteopontin, an osteoblast matrix protein, is thought to play a role in the development of vascular complication among patients with diabetes [38]. Previous studies have shown the association between elevated HbA1c and coronary artery calcification using CT [39, 40]. In a study on 2076 participants without DM, Carson et al. evaluated the predictive value of HbA1c using CT at baseline and after a 5-year follow-up [39]. They showed that higher HbA1c was independently associated with advanced coronary artery calcification and calcification progression. Our study demonstrated that low 1,5-AG level was related with the incidence of severe coronary calcification, independent of the other risk factors. Furthermore, patients with CKD, which had been recognized a strong risk factor for coronary artery calcification, were excluded in the present study. Therefore, among patients with relatively low HbA1c and without CKD, 1,5-AG might be useful marker to predict the incidence of severe coronary artery calcification and future cardiovascular events.
This study had several limitations. First, as a single-center, observational study on a small patient cohort, unknown confounding factors might have affected the outcomes. Studies with large sample size and racial diversity would be more effective in evaluating the value of 1,5-AG levels. Second, we detected lesion calcifications using gray-scale IVUS only. Although the calcium thickness or volume could not be calculated by IVUS, these can be easily used to detect lesion calcification [41, 42]. Finally, we don’t have any vitro experiments that would help support the results of the present study. Previous study demonstrated that advanced glycation end products induce calcification of vascular smooth muscle cells by osteoblast-like differentiation of smooth muscle cells [43]. Further studies to prove the association between low 1,5-AG levels and coronary calcification are needed.
Conclusions
This study found that low 1,5-AG level, which indicated postprandial hyperglycemia, was associated with the severity of coronary artery calcification. Further studies are needed to confirm the independent effects of postprandial hyperglycemia on coronary artery calcification.
Availability of data and materials
The datasets during and/or analyzed during the current study are available from the corresponding author with reasonable request.
Abbreviations
- ACS:
-
acute coronary syndrome
- 1,5-AG:
-
1,5-anhydro-d-glucitol
- BP:
-
blood pressure
- CAD:
-
coronary artery disease
- CI:
-
confidence interval
- CSA:
-
cross-sectional area
- CT:
-
computed tomography
- CVD:
-
cardiovascular disease
- DM:
-
diabetes mellitus
- EEM:
-
external elastic membrane
- IQR:
-
interquartile range
- HbA1c:
-
glycosylated hemoglobin
- IVUS:
-
intravascular ultrasound
- MI:
-
myocardial infarction
- OR:
-
odds ratio
- PCI:
-
percutaneous coronary intervention
- SD:
-
standard deviation
- TAV:
-
total atheroma volume
References
Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241(19):2035–8.
Rawshani A, Rawshani A, Franzen S, Eliasson B, Svensson AM, Miftaraj M, McGuire DK, Sattar N, Rosengren A, Gudbjornsdottir S. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017;376(15):1407–18.
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–12.
Bonora E, Muggeo M. Postprandial blood glucose as a risk factor for cardiovascular disease in type II diabetes: the epidemiological evidence. Diabetologia. 2001;44(12):2107–14.
Ceriello A, Hanefeld M, Leiter L, Monnier L, Moses A, Owens D, Tajima N, Tuomilehto J. Postprandial glucose regulation and diabetic complications. Arch Intern Med. 2004;164(19):2090–5.
Gohbara M, Hibi K, Mitsuhashi T, Maejima N, Iwahashi N, Kataoka S, Akiyama E, Tsukahara K, Kosuge M, Ebina T, et al. Glycemic variability on continuous glucose monitoring system correlates with non-culprit vessel coronary plaque vulnerability in patients with first-episode acute coronary syndrome—optical coherence tomography study. Circ J. 2016;80(1):202–10.
Dungan KM. 1,5-Anhydroglucitol (GlycoMark) as a marker of short-term glycemic control and glycemic excursions. Expert Rev Mol Diagn. 2008;8(1):9–19.
Dungan KM, Buse JB, Largay J, Kelly MM, Button EA, Kato S, Wittlin S. 1,5-Anhydroglucitol and postprandial hyperglycemia as measured by continuous glucose monitoring system in moderately controlled patients with diabetes. Diabetes Care. 2006;29(6):1214–9.
Yamanouchi T, Ogata N, Tagaya T, Kawasaki T, Sekino N, Funato H, Akaoka L, Miyashita H. Clinical usefulness of serum 1,5-anhydroglucitol in monitoring glycaemic control. Lancet. 1996;347(9014):1514–8.
Torimoto K, Okada Y, Mori H, Tanaka Y. Low levels of 1,5-anhydro-d-glucitol are associated with vascular endothelial dysfunction in type 2 diabetes. Cardiovasc Diabetol. 2014;13:99.
Ikeda N, Hara H, Hiroi Y. 1,5-Anhydro-d-glucitol predicts coronary artery disease prevalence and complexity. J Cardiol. 2014;64(4):297–301.
Ikeda N, Hara H, Hiroi Y, Nakamura M. Impact of serum 1,5-anhydro-d-glucitol level on prediction of major adverse cardiac and cerebrovascular events in non-diabetic patients without coronary artery disease. Atherosclerosis. 2016;253:1–6.
Ouchi S, Shimada K, Miyazaki T, Takahashi S, Sugita Y, Shimizu M, Murata A, Kadoguchi T, Kato T, Aikawa T, et al. Low 1,5-anhydroglucitol levels are associated with long-term cardiac mortality in acute coronary syndrome patients with hemoglobin A1c levels less than 7.0. Cardiovasc Diabetol. 2017;16(1):151.
Takahashi S, Shimada K, Miyauchi K, Miyazaki T, Sai E, Ogita M, Tsuboi S, Tamura H, Okazaki S, Shiozawa T, et al. Low and exacerbated levels of 1,5-anhydroglucitol are associated with cardiovascular events in patients after first-time elective percutaneous coronary intervention. Cardiovasc Diabetol. 2016;15(1):145.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53(6):982–92.
Teramoto T, Sasaki J, Ishibashi S, Birou S, Daida H, Dohi S, Egusa G, Hiro T, Hirobe K, Iida M, et al. Diagnostic criteria for dyslipidemia. J Atheroscler Thromb. 2013;20(8):655–60.
Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, Pinto FJ, Rosenfield K, Siegel RJ, Tuzcu EM, et al. American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001;37(5):1478–92.
Kakuta K, Dohi K, Miyoshi M, Yamanaka T, Kawamura M, Masuda J, Kurita T, Ogura T, Yamada N, Sumida Y, et al. Impact of renal function on the underlying pathophysiology of coronary plaque composition in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2017;16(1):131.
Yamada H, Tanaka A, Kusunose K, Amano R, Matsuhisa M, Daida H, Ito M, Tsutsui H, Nanasato M, Kamiya H, et al. Effect of sitagliptin on the echocardiographic parameters of left ventricular diastolic function in patients with type 2 diabetes: a subgroup analysis of the PROLOGUE study. Cardiovasc Diabetol. 2017;16(1):63.
Ma C, Sheng J, Liu Z, Guo M. Excretion rates of 1,5-anhydro-d-glucitol, uric acid and microalbuminuria as glycemic control indexes in patients with type 2 diabetes. Sci Rep. 2017;7:44291.
Yoshida N, Yamamoto H, Shinke T, Otake H, Kuroda M, Terashita D, Takahashi H, Sakaguchi K, Hirota Y, Emoto T, et al. Impact of CD14(++)CD16(+) monocytes on plaque vulnerability in diabetic and non-diabetic patients with asymptomatic coronary artery disease: a cross-sectional study. Cardiovasc Diabetol. 2017;16(1):96.
Nakamura S, Tanabe K, Yoshinaga K, Shimura F, Oku T. Effects of 1,5-anhydroglucitol on postprandial blood glucose and insulin levels and hydrogen excretion in rats and healthy humans. Br J Nutr. 2017;118(2):81–91.
Palta P, Huang ES, Kalyani RR, Golden SH, Yeh HC. Hemoglobin A1c and mortality in older adults with and without diabetes: results from the national health and nutrition examination surveys (1988–2011). Diabetes Care. 2017;40(4):453–60.
Raghavan S, Vassy JL, Ho YL, Song RJ, Gagnon DR, Cho K, Wilson PWF, Phillips LS. Diabetes mellitus-related all-cause and cardiovascular mortality in a national cohort of adults. J Am Heart Assoc. 2019;8(4):e011295.
American Diabetes Association. Glycemic targets. Diabetes Care. 2016;39(Suppl 1):S39–46.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–53.
Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–72.
Otsuka F, Sakakura K, Yahagi K, Joner M, Virmani R. Has our understanding of calcification in human coronary atherosclerosis progressed? Arterioscler Thromb Vasc Biol. 2014;34(4):724–36.
Williams MC, Moss AJ, Dweck M, Adamson PD, Alam S, Hunter A, Shah ASV, Pawade T, Weir-McCall JR, Roditi G, et al. Coronary artery plaque characteristics associated with adverse outcomes in the SCOT-HEART study. J Am Coll Cardiol. 2019;73(3):291–301.
Criqui MH, Denenberg JO, Ix JH, McClelland RL, Wassel CL, Rifkin DE, Carr JJ, Budoff MJ, Allison MA. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014;311(3):271–8.
Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210–5.
Sangiorgi G, Rumberger JA, Severson A, Edwards WD, Gregoire J, Fitzpatrick LA, Schwartz RS. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: a histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol. 1998;31(1):126–33.
Baumgart D, Schmermund A, Goerge G, Haude M, Ge J, Adamzik M, Sehnert C, Altmaier K, Groenemeyer D, Seibel R, et al. Comparison of electron beam computed tomography with intracoronary ultrasound and coronary angiography for detection of coronary atherosclerosis. J Am Coll Cardiol. 1997;30(1):57–64.
Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92(8):2157–62.
Raggi P, Shaw LJ, Berman DS, Callister TQ. Prognostic value of coronary artery calcium screening in subjects with and without diabetes. J Am Coll Cardiol. 2004;43(9):1663–9.
Lehto S, Niskanen L, Suhonen M, Ronnemaa T, Laakso M. Medial artery calcification. A neglected harbinger of cardiovascular complications in non-insulin-dependent diabetes mellitus. Arterioscler Thromb Vasc Biol. 1996;16(8):978–83.
Towler DA, Bidder M, Latifi T, Coleman T, Semenkovich CF. Diet-induced diabetes activates an osteogenic gene regulatory program in the aortas of low density lipoprotein receptor-deficient mice. J Biol Chem. 1998;273(46):30427–34.
Mori S, Takemoto M, Yokote K, Asaumi S, Saito Y. Hyperglycemia-induced alteration of vascular smooth muscle phenotype. J Diabetes Complicat. 2002;16(1):65–8.
Carson AP, Steffes MW, Carr JJ, Kim Y, Gross MD, Carnethon MR, Reis JP, Loria CM, Jacobs DR Jr, Lewis CE. Hemoglobin a1c and the progression of coronary artery calcification among adults without diabetes. Diabetes Care. 2015;38(1):66–71.
Chang Y, Yun KE, Jung HS, Kim CW, Kwon MJ, Sung E, Ryu S. A1C and coronary artery calcification in nondiabetic men and women. Arterioscler Thromb Vasc Biol. 2013;33(8):2026–31.
Friedrich GJ, Moes NY, Muhlberger VA, Gabl C, Mikuz G, Hausmann D, Fitzgerald PJ, Yock PG. Detection of intralesional calcium by intracoronary ultrasound depends on the histologic pattern. Am Heart J. 1994;128(3):435–41.
Kawasaki M, Bouma BE, Bressner J, Houser SL, Nadkarni SK, MacNeill BD, Jang IK, Fujiwara H, Tearney GJ. Diagnostic accuracy of optical coherence tomography and integrated backscatter intravascular ultrasound images for tissue characterization of human coronary plaques. J Am Coll Cardiol. 2006;48(1):81–8.
Tanikawa T, Okada Y, Tanikawa R, Tanaka Y. Advanced glycation end products induce calcification of vascular smooth muscle cells through RAGE/p38 MAPK. J Vasc Res. 2009;46(6):572–80.
Acknowledgements
The authors are grateful to the staff of the Department of Cardiovascular Medicine at Juntendo University and the Department of Cardiovascular Medicine at Juntendo University Shizuoka Hospital. The authors also appreciate the secretarial assistance of Ms. Yumi Nozawa.
Funding
None.
Author information
Authors and Affiliations
Contributions
HW and TD contributed to conception of the study and the writing of the manuscript. HW, TD, NT, HE, YK, IO, HI, SO, KI and SS contributed to acquire and analyze the data. HW, TD, KM, MO, KS and HD contributed to drafting or revising the manuscript. All authors agree with manuscript results and conclusions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board at the Juntendo University Hospital. All participants provided written informed consent.
Consent for publication
Participants were informed of data sharing with their name and identity hidden per consent.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wada, H., Dohi, T., Miyauchi, K. et al. Impact of serum 1,5-anhydro-d-glucitol level on the prediction of severe coronary artery calcification: an intravascular ultrasound study. Cardiovasc Diabetol 18, 69 (2019). https://doi.org/10.1186/s12933-019-0878-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-019-0878-1