Abstract
Although high thromboembolic risk was assumed in elderly patients with heart failure (HF) and atrial fibrillation (AF), inadequate control of prothrombin time/international normalized ratio was often observed in patients using vitamin K antagonists (VKAs). We hypothesized that patients treated with direct oral anticoagulants (DOAC) would have a better outcome than those treated with VKAs. The aim of this study was to compare the efficacies of DOACs and VKAs in elderly patients with HF and AF. We retrospectively analyzed data from a multicenter, prospective observational cohort study. A total of 1036 patients who were hospitalized for acute decompensated HF were enrolled. We assessed 329 patients aged > 65 years who had non-valvular AF and divided them into 2 groups according to the anticoagulant therapy they received. A subgroup analysis was performed using renal dysfunction based on estimated glomerular filtration rate (eGFR; mL/min/1.73 m2). The primary outcome was all-cause mortality, and the secondary outcomes were non-cardiovascular death or stroke. The median follow-up period was 730 days (range 334–1194 days). The primary outcome was observed in 84 patients; non-cardiovascular death, in 25 patients; and stroke, in 14 patients. The Kaplan–Meier analysis revealed that all-cause mortality was significantly lower in the DOAC group than in the VKA group (log-rank p = 0.033), whereas the incidence rates of non-cardiovascular death (log-rank p = 0.171) and stroke (log-rank p = 0.703) were not significantly different in the crude population. DOAC therapy was not associated with lower mortality in the crude population (log-rank p = 0.146) and in the eGFR ≥ 45 mL/min/1.73 m2 subgroup (log-rank p = 0.580). However, DOAC therapy was independently associated with lower mortality after adjustments for age, diabetes mellitus, and albumin level (hazard ratio, 0.55; 95% confidence interval, 0.30–0.99; p = 0.045) in the eGFR < 45 mL/min/1.73 m2 subgroup. Compared with VKA therapy, DOAC therapy was associated with lower risk of all-cause mortality in the elderly HF patients with AF and renal dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is a common form of cardiac arrhythmia in elderly patients. Moreover, heart failure (HF) or renal dysfunction frequently coexists with AF [1], and high thromboembolic risk was assumed in elderly patients with HF and AF [2]. Vitamin K antagonists (VKA) have been the standard therapeutic agents for patients with AF for decades, and a previous study reported that VKA reduced stroke risk by 64% and mortality by 26% as compared with placebo [3]. VKAs are effective and relatively safe drugs with an adequate time in therapeutic range (TTR) of > 70%, but inadequate control of prothrombin time/international normalized ratio is often observed in patients using VKAs [4]. A subanalysis of data from the ROCKET AF (Rivaroxaban Once Daily Oral Direct Factor Xa Inhibitor Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation) trial reported that renal dysfunction was associated with a lower TTR of VKA during the administration period [5]. In the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation registry, multiple comorbidities such as frailty, HF, renal dysfunction, chronic obstructive pulmonary disease, and diabetes were identified as risk factors of lower TTR [6]. Patients with multiple comorbidities tend to be given more concomitant drugs, which are associated with low treatment adherence. Direct oral anticoagulants (DOACs) have become common therapeutic agents for preventing stroke or systemic embolism in patients with AF. Four DOACs are available for paroxysmal/persistent AF. Previous studies revealed that use of DOACs as compared with VKAs was associated with lower risks of stroke, systemic embolism, and major bleeding [7, 8], but the efficacy of DOACs in patients with renal dysfunction has not been fully discussed. Physicians sometimes hesitate to prescribe DOACs for elderly patients with renal dysfunction because of fear of hemorrhagic complications. Recently, Makani et al. [9] reported the safety and efficacy of DOAC use in patients with concomitant renal dysfunction and AF. However, a meta-analysis of DOACs indicated that the standard dose of DOACs as compared with that of VKAs was safer and more effective in Asians than in non-Asians [10]. We hypothesized that better outcomes can be obtained using DOACs in high-risk patients with HF. The aim of this study was to evaluate the efficacy of DOACs in HF patients with AF and renal dysfunction in the Japanese population.
Materials and methods
Patient population
This study was a post hoc analysis of a multicenter, prospective observational cohort study. In this study, 1036 consecutive patients who were admitted at 13 institutions in Nagano Prefecture, Japan, between July 2014 and December 2018 because of acute decompensated HF (ADHF) were enrolled. The diagnosis of HF was based on the criteria used in the Framingham study [11]. The exclusion criteria were patients aged < 20 years, those who were impossible to follow-up, those from whom informed consent was difficult to obtain, and those with acute coronary syndrome. After admission, medical therapy was initiated at the discretion of the physician. Clinical data, including patient demographics, past medical history, drug usage, echocardiography findings, electrocardiography findings, and laboratory data, were collected during the compensated state of HF. Echocardiography was performed in accordance with the recommendations of the American Society of Echocardiography [12]. After the patients’ discharge, follow-up data were collected from their medical records or through telephone interview. The clinical events were all-cause death, cardiovascular death, acute coronary syndrome, stroke, hospitalization for acute decompensated HF, and hospitalization for any cardiovascular disease. This study was approved by the ethics committees of the hospitals and performed in accordance with the tenets of the 1975 Declaration of Helsinki for clinical research protocols. Informed consent was obtained from all the patients.
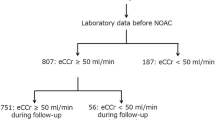
Study protocol
We screened 541 patients aged > 65 years who had paroxysmal/persistent AF and excluded 212 patients who had undergone surgery, had severe valvular disease, and had not received anticoagulant therapy. The remaining 329 patients were assessed as having non-valvular AF (NVAF) and divided into 2 groups according to the anticoagulant therapy they received (Fig. 1). A subgroup analysis was performed using renal dysfunction based on estimated glomerular filtration rate (eGFR; mL/min/1.73 m2). The cutoff value was set at 45 mL/min/1.73 m2 as an approximate value of median eGFR (46 mL/min/1.73m2) and as the boundary of chronic kidney disease (CKD) grade between G3a and G3b. The primary outcome was all-cause mortality, and the secondary outcomes were non-cardiovascular death and stroke.
Statistical analyses
Continuous variables are expressed as mean ± standard deviation when normally distributed and as median and interquartile range when non-normally distributed. Normality was assessed using the Shapiro–Wilk W test. Categorical variables are expressed as number and percentage. The patients’ baseline characteristics were compared using a contingency table and t test for normally distributed continuous variables, the Mann–Whitney U test for non-normally distributed continuous variables, and the chi-square test for categorical variables. P values of < 0.05 were considered statistically significant. The cumulative incidence of the end point was analyzed using the Kaplan–Meier method, and differences were assessed with the log-rank test. Cox proportional hazard analysis was performed to adjust for baseline differences and assess whether the variables were independent predictors of outcome. Following univariate analysis, covariates that were associated with outcome (p < 0.1) were included in the multivariate model. The SPSS version 27.0 statistical software (SPSS Inc., Chicago, Illinois) was used in the analysis.
Results
Patients’ characteristics
Among the 329 patients, 119 were treated with VKA and 210 were treated with DOACs. The patients’ baseline characteristics are shown in Table 1. The median age was 82 years (interquartile range: 76–86 years), and 49% (n = 161) of the patients were female. Among the comorbidities, diabetes mellitus was more frequently observed in the VKA group, but history of stroke was more prevalent in the DOAC group. Laboratory data indicated that hemoglobin level was lower in the VKA group, but serum albumin level, eGFR, brain natriuretic peptide level, and C-reactive protein level were not significantly different between the two groups. Whereas β-blocker was more frequently prescribed in the DOAC group, the use frequencies of antiplatelet and conventional drugs for HF, including angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, and mineralocorticoid receptor antagonist were not markedly different between the two groups.
Outcomes
The median follow-up period was 730 days (interquartile range 334–1194 days). The primary outcome was observed in 84 patients (25.5%). Non-cardiovascular death occurred in 25 patients (7.6%), and stroke occurred in 14 patients (4.3%). The hazard ratio (HRs) and 95% confidence interval (CIs) for the primary and secondary outcomes are shown in Table 2. The incidence of non-cardiovascular death and stroke were not statistically significantly different between the two groups, but all-cause death was more frequently observed in the VKA group. The Kaplan–Meier analyses for the primary and secondary outcomes are shown in Fig. 2. All-cause mortality was significantly lower in the DOAC group than in the VKA group (log-rank p = 0.033), while the incidence rates of non-cardiovascular death and stroke were not significantly different between the two groups. DOAC use was not significantly associated with all-cause mortality (HR, 0.71; 95% CI 0.45–1.13; p = 0.146) in multivariate analysis of the crude population, although it was associated with a lower incidence of the primary outcome (HR, 0.63; 95% CI 0.41–0.97; p = 0.035) in univariate analysis (Table 3).
Kaplan–Meier analysis for the incidence of all-cause mortality, non-cardiovascular death, stroke. All-cause mortality was significantly lower in the DOAC group than in the VKA group, but non-cardiovascular death and stroke were not statistically significantly different between the two groups. DOAC direct oral anticoagulant, VKA vitamin K antagonists
The subgroup analysis for renal dysfunction is shown in Fig. 3. DOAC administration was associated with lower mortality rates in the eGFR < 45 mL/min/1.73 m2 subgroup (log-rank p = 0.036) but not in the eGFR ≥ 45 mL/min/1.73 m2 subgroup (log-rank p = 0.581). The Cox proportional hazard analysis revealed that DOAC therapy was independently associated with lower mortality after adjustments for age, diabetes mellitus, and albumin level (HR, 0.55; 95% CI 0.30–0.99; p = 0.045) in the eGFR < 45 mL/min/1.73 m2 subgroup (Table 4) but not associated in the eGFR ≥ 45 mL/min/1.73 m2 subgroup (HR, 1.27; 95% CI 0.60–2.67; p = 0.533).
Kaplan–Meier analysis for the incidence of all-cause mortality in eGFR < 45 mL/min/1.73 m2 subgroup and eGFR ≥ 45 mL/min/1.73 m2 subgroup. DOAC administration was associated with lower mortality rates in the eGFR < 45 mL/min/1.73 m2 subgroup but not associated in the eGFR ≥ 45 mL/min/1.73 m2 subgroup. DOAC direct oral anticoagulant, eGFR estimated glomerular filtration rate, VKA vitamin K antagonists
Discussion
The major finding of our study was that DOAC therapy was independently associated with lower mortality rate in patients with renal dysfunction in the Japanese population. Previous studies showed that use of DOACs was associated with lower risks of stroke and systemic embolism, but its association with all-cause mortality has not been fully evaluated especially in patients with renal dysfunction. Four mega studies were conducted for each DOAC; however, three studies (ROCKET AF, RE-LY [Randomized Evaluation of Long-term Anticoagulant Therapy], and ENGAGE AF-TIMI 48 [Effective Anticoagulation with Factor xA Next Generation in Atrial Fibrillation–Thrombolysis in Myocardial Infarction study 48]) excluded patients with creatinine clearance values < 30 mL/min. The ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial excluded patients with creatinine clearance values < 25 mL/min. Recently, Makani et al. reported the safety and efficacy of DOAC use in patients with concomitant renal dysfunction and AF. In this study, the patients were classified into three groups according to eGFR (> 60, 30–60, and < 30 mL/min/1.73 m2), and DOAC administration was associated with lower risk of mortality across all stages of renal dysfunction [9]. However, the efficacy of DOACs in the patients with renal dysfunction was not equal across races and ethnicity because the meta-analysis of five mega studies revealed that the usual DOAC dose as compared with that of VKA was effective for the prevention of stroke or systemic prevention and safer in terms of reducing the risk of major bleeding in Asians than in non-Asians [10]. The difference in the efficacy of DOACs between the populations remains an unsolved problem.
In the Japanese population, three major observational studies were conducted in patients with AF [13,14,15]. The J-RHYTHM Registry 2, a multicenter observational study, revealed that the incidence of all-cause death in the DOAC group was extremely low as compared with those in the non-OAC and VKA groups. However, this study expanded the follow-up period in the J-RHYTHM Registry, which enrolled patients from January 2010 to July 2010. At baseline, the antithrombotic therapy was VKA only (5737 patients), but 923 patients were switched from VKA to DOAC, and the exact follow-up time after the switch was unknown. The Fushimi AF registry was a prospective, observational multicenter cohort study conducted between March 2011 and November 2015. In this registry, DOAC use was not statistically associated with stroke or systemin embolism (p = 0.70) or major bleeding (p = 0.34) after propensity score matching, but all-cause mortality was not evaluated [15]. The Shinken Database is a single-hospital-based cohort that was started in 2004, and the 9-year trends of anticoagulation therapy and thromboembolic events or major bleeding were analyzed, but the incidence of all-cause death was not evaluated.
Recently, the SAKURA-AF registry was established to compare the safety and efficacy of DOACs and VKAs in the Japanese AF population and revealed that the incidence rates of stroke/systemic embolism, major bleeding, and all-cause mortality were not statistically significantly different between the VKA and DOAC groups after adjustment by propensity score matching.
Our study represents a real-world analysis of the efficacy of DOACs in elderly NVAF patients with renal dysfunction. As compared with VKA administration, the use of DOACs was associated with lower mortality rates among patients with AF and renal dysfunction. Although this was a retrospective analysis, our findings suggest that DOACs do not appear to be inferior to VKA, and physicians should not hesitate to prescribe DOACs for patients with concomitant renal dysfunction and AF.
Two hypotheses may explain the association of DOAC use with the lower risk of mortality in our registry. First, the SAKURA-AF registry included TTR, which was relatively high (65.4% ± 31.1%) as compared with those in other recent randomized controlled trials (mean TTR: 55–68%) [16,17,18]. The better TTR in the VKA users would result in a low clinical event rate as in the DOAC users. Although our registry did not include TTR, it would be lower in the eGFR < 45 mL/min/1.73 m2 subgroup than in the eGFR ≥ 45 mL/min/1.73 m2 subgroup because renal dysfunction was identified as risk factor of lower TTR [6]. Moreover, Lin et al. reported that VKA was associated with higher incident of significant bleeding and myocardial infarction in patients with stage 3–5 CKD [19]. Second, the mean CHADS2 score in our registry was 3.0 in both subgroups, which was relatively higher than those in other registries in Japan, ranging from 1.8 to 2.1 [15, 20, 21], or the SAKURA-AF registry, ranging from 1.7 to 1.9 [22]. Patients with high CHADS2 scores have more comorbidities and are associated with the use of more concomitant drug treatments, that is, polypharmacy. A previous study reported that adverse clinical outcomes such as death and bleeding complications occurred more frequently in patients with polypharmacy [23,24,25]. These outcomes could be derived from the increasing risk of drug-to-drug interactions with the use of many concomitant drug treatments. Although our registry did not analyze the number of drugs used, having more comorbidities would be associated with the incidence of stroke or other adverse clinical events and lead to high mortality in patient with renal dysfunction. Further randomized control trials are needed to certify our hypotheses.
Limitations
This study has several limitations. First, the sample size was relatively small and it would not be enough to represent the general population. Second, we did not evaluate TTR in the VKA group. Third, we did not specify the kinds of DOACs used. In the 2019 AHA/ACC guideline, only VKA and apixaban are recommended for patients with severe CKD, and other DOACs are not recommended [26]. Safety and efficacy would differ between DOACs. Fourth, the HAS-BLED (hypertension, abnormal renal/liver function, previous stroke, bleeding history or predisposition, labile international normalized ratio [INR], elderly and drugs/alcohol consumption) score could not be determined because information on alcohol dependency was unavailable. Fifth, only three patients had severe renal dysfunction (eGFR < 15 mL/min/1.73 m2), and we could not perform a sufficient evaluation for these patients.
Conclusion
DOAC therapy for HF patients with NVAF and renal dysfunction is associated with lower mortality than VKA therapy.
References
Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, D’Agostino RB, Murabito JM, Kannel WB, Benjamin EJ (2003) Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation 107(23):2920–2925
Jun M, James MT, Manns BJ, Quinn RR, Ravani P, Tonelli M, Perkovic V, Winkelmayer WC, Ma ZH, Hemmelgarn BR, Network AKD (2015) The association between kidney function and major bleeding in older adults with atrial fibrillation starting warfarin treatment: population based observational study. BMJ 350:246
Hart RG, Pearce LA, Aguilar MI (2007) Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 146(12):857–867
Guimarães PO, Lopes RD, Alexander JH, Thomas L, Hellkamp AS, Hijazi Z, Hylek EM, Gersh BJ, Garcia DA, Verheugt FWA, Hanna M, Flaker G, Vinereanu D, Granger CB (2019) International normalized ratio control and subsequent clinical outcomes in patients with atrial fibrillation using warfarin. J Thromb Thrombolysis 48(1):27–34
Fordyce CB, Hellkamp AS, Lokhnygina Y, Lindner SM, Piccini JP, Becker RC, Berkowitz SD, Breithardt G, Fox KA, Mahaffey KW, Nessel CC, Singer DE, Patel MR, Committee RAS, Investigators, (2016) On-treatment outcomes in patients with worsening renal function with rivaroxaban compared with warfarin: insights from ROCKET AF. Circulation 134(1):37–47
Pokorney SD, Simon DN, Thomas L, Fonarow GC, Kowey PR, Chang P, Singer DE, Ansell J, Blanco RG, Gersh B, Mahaffey KW, Hylek EM, Go AS, Piccini JP, Peterson ED (2015) Patients’ time in therapeutic range on warfarin among US patients with atrial fibrillation: Results from ORBIT-AF registry. Am Heart J 170(1):141–148
Pan KL, Singer DE, Ovbiagele B, Wu YL, Ahmed MA, Lee M (2017) Effects of non-vitamin K antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and valvular heart disease: A systematic review and meta-analysis. J Am Heart 6(7):e005835
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, Camm AJ, Weitz JI, Lewis BS, Parkhomenko A, Yamashita T, Antman EM (2014) Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 383(9921):955–962
Makani A, Saba S, Jain SK, Bhonsale A, Sharbaugh MS, Thoma F, Wang Y, Marroquin OC, Lee JS, Estes NAM, Mulukutla SR (2020) Safety and efficacy of direct oral anticoagulants versus warfarin in patients with chronic kidney disease and atrial fibrillation. Am J Cardiol 125(2):210–214
Wang KL, Lip GY, Lin SJ, Chiang CE (2015) Non-vitamin K antagonist oral anticoagulants for stroke prevention in asian patients with nonvalvular atrial fibrillation: meta-analysis. Stroke 46(9):2555–2561
McKee PA, Castelli WP, McNamara PM, Kannel WB (1971) The natural history of congestive heart failure: the Framingham study. N Engl J Med 285(26):1441–1446
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of echocardiography and the European Association of cardiovascular imaging. J Am Soc Echocardiogr 29(4):277–314
Atarashi H, Inoue H, Okumura K, Yamashita T, Origasa H (2011) Investigation of optimal anticoagulation strategy for stroke prevention in Japanese patients with atrial fibrillation–the J-RHYTHM Registry study design. J Cardiol 57(1):95–99
Suzuki S, Otsuka T, Sagara K, Semba H, Kano H, Matsuno S, Takai H, Kato Y, Uejima T, Oikawa Y, Nagashima K, Kirigaya H, Kunihara T, Yajima J, Sawada H, Aizawa T, Yamashita T (2016) Nine-year trend of anticoagulation use, thromboembolic events, and major bleeding in patients with non-valvular atrial fibrillation-shinken database analysis. Circ J 80(3):639–649
Yamashita Y, Uozumi R, Hamatani Y, Esato M, Chun YH, Tsuji H, Wada H, Hasegawa K, Ogawa H, Abe M, Morita S, Akao M (2017) Current status and outcomes of direct oral anticoagulant use in real-world atrial fibrillation patients-Fushimi AF registry. Circ J 81(9):1278–1285
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361(12):1139–1151
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Spinar J, Ruzyllo W, Ruda M, Koretsune Y, Betcher J, Shi M, Grip LT, Patel SP, Patel I, Hanyok JJ, Mercuri M, Antman EM, Investigators EA-T (2013) Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 369(22):2093–2104
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL, Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365(11):981–992
Lin MC, Streja E, Soohoo M, Hanna M, Savoj J, Kalantar-Zadeh K, Lau WL (2017) Warfarin use and increased mortality in end-stage renal disease. Am J Nephrol 46(4):249–256
Akao M, Chun YH, Esato M, Abe M, Tsuji H, Wada H, Hasegawa K (2014) Inappropriate use of oral anticoagulants for patients with atrial fibrillation. Circ J 78(9):2166–2172
Kodani E, Atarashi H, Inoue H, Okumura K, Yamashita T, Origasa H (2016) Beneficial effect of non-vitamin K antagonist oral anticoagulants in patients with nonvalvular atrial fibrillation—results of the J-RHYTHM registry 2. Circ J 80(4):843–851
Okumura Y, Yokoyama K, Matsumoto N, Tachibana E, Kuronuma K, Oiwa K, Matsumoto M, Kojima T, Hanada S, Nomoto K, Arima K, Takahashi F, Kotani T, Ikeya Y, Fukushima S, Itou S, Kondo K, Chiku M, Ohno Y, Onikura M, Hirayama A (2018) Three-year clinical outcomes associated with warfarin vs. direct oral anticoagulant use among japanese patients with atrial fibrillation—Findings from the SAKURA AF registry. Circ J 82(10):2500–2509
Gnjidic D, Hilmer SN, Blyth FM, Naganathan V, Waite L, Seibel MJ, McLachlan AJ, Cumming RG, Handelsman DJ, Le Couteur DG (2012) Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol 65(9):989–995
Jyrkkä J, Enlund H, Korhonen MJ, Sulkava R, Hartikainen S (2009) Patterns of drug use and factors associated with polypharmacy and excessive polypharmacy in elderly persons: results of the Kuopio 75+ study: a cross-sectional analysis. Drugs Aging 26(6):493–503
Piccini JP, Hellkamp AS, Washam JB, Becker RC, Breithardt G, Berkowitz SD, Halperin JL, Hankey GJ, Hacke W, Mahaffey KW, Nessel CC, Singer DE, Fox KA, Patel MR (2016) Polypharmacy and the efficacy and safety of rivaroxaban versus warfarin in the prevention of stroke in patients with nonvalvular atrial fibrillation. Circulation 133(4):352–360
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW (2019) 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation 140(2):e125–e151
Acknowledgements
We are grateful to all the cardiologists of the participating centers and the clinical research coordinators.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakai, T., Motoki, H., Fuchida, A. et al. Comparison of prognostic impact of anticoagulants in heart failure patients with atrial fibrillation and renal dysfunction: direct oral anticoagulants versus vitamin K antagonists. Heart Vessels 37, 1232–1241 (2022). https://doi.org/10.1007/s00380-022-02027-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02027-w