Abstract
Limited data regarding the prognostic impact of ventricular tachyarrhythmias related to out-of-hospital (OHCA) compared to in-hospital cardiac arrest (IHCA) is available. A large retrospective single-center observational registry with all patients admitted due to ventricular tachyarrhythmias was used including all consecutive patients with ventricular tachycardia (VT) and fibrillation (VF) on admission from 2002 to 2016. Survivors discharged after OHCA were compared to those after IHCA using multivariable Cox regression models and propensity-score matching for evaluation of the primary endpoint of long-term all-cause mortality at 2.5 years. Secondary endpoints were all-cause mortality at 6 months and cardiac rehospitalization at 2.5 years. From 2.422 consecutive patients with ventricular tachyarrhythmias, a total of 524 patients survived cardiac arrest and were discharged from hospital (OHCA 62%; IHCA 38%). In about 50% of all cases, acute myocardial infarction was the underlying disease leading to ventricular tachyarrhythmias with consecutive aborted cardiac arrest. Survivors of IHCA were associated with increased long-term all-cause mortality compared to OHCA even after multivariable adjustment (28% vs. 16%; log rank p = 0.001; HR 1.623; 95% CI 1.002–2.629; p = 0.049) and after propensity-score matching (28% vs. 19%; log rank p = 0.045). Rates of cardiac rehospitalization rates at 2.5 years were equally distributed between OHCA and IHCA survivors. In patients presenting with ventricular tachyarrhythmias, survivors of IHCA were associated with increased risk for all-cause mortality at 2.5 years compared to OHCA survivors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sudden cardiac arrest is common and one of the leading causes of death in developed industrial countries [1]. Most non-traumatic OHCA result from acute coronary syndromes (ACS), structural heart disease or cardiac arrhythmias [1, 2]. In-hospital cardiac arrest (IHCA) data are scarce; however, reported incidences range from 1 to 5 events per 1000 hospital admissions [3, 4]. Immediate cardiopulmonary resuscitation (CPR) and treatment of the underlying cardiac or non-cardiac pathology are necessary for a return of a spontaneous circulation (ROSC).
Mortality rates of cardiac arrest remained stable in the last decades. In Europe, overall survival rate is 10.3% after OHCA and 23% after IHCA [1, 5]. The majority of deaths occur during the initial resuscitation. However, a substantial portion of deaths from cardiac arrest occur in patients with primarily successful resuscitation [6]. This increased mortality post resuscitation can be attributed to a combination of whole-body ischemia, reperfusion-mediated tissue damage and underlying diseases that lead to cardiac arrest [7].
Survival and outcome analyses of OHCA and IHCA can be numerously found in current literature, showing better short-term survival rates for IHCA in many studies [8, 9]. The present study evaluates the long-term prognostic impact of OHCA and IHCA in consecutive patients presenting with ventricular tachyarrhythmias.
Methods
Study patients, design and data collection
The present study is derived from an observational analysis of the “Registry of Malignant Arrhythmias and Sudden Cardiac Death—Influence of Diagnostics and Interventions (RACE-IT)” and represents a single-center registry including consecutive patients presenting with ventricular tachyarrhythmias and aborted sudden cardiac death (SCD) being admitted to the University Medical Center Mannheim (UMM), Germany (clinicaltrials.gov identifier: NCT02982473) from 2002 until 2016. The UMM is a large tertiary care University hospital in the metropolitan area of Rhine/Main with over 1.350 beds with optional supply of extracorporeal membrane oxygenation (ECMO) and target temperature management (TTM).
Ventricular tachyarrhythmias comprised ventricular tachycardia (VT) and fibrillation (VF), as defined by current international guidelines [10]. Sustained VT was defined by a duration of > 30 s or causing hemodynamic collapse within 30 s [10].
The overall presence of an activated ICD comprises the total sum of all patients with a prior implanted ICD before admission, those undergoing new ICD implantation at index stay, as well as those with ICD implantation at the complete follow-up period after index hospitalization, referring to transvenous ICD, subcutaneous-ICD (s-ICD) and cardiac resynchronization therapy with defibrillator function (CRT-D). Pharmacological treatment was documented according to the discharge medication of patients surviving index hospitalization.
Values of left ventricular ejection fraction (LVEF) were retrieved from standardized transthoracic echocardiographic examinations usually being performed before hospital discharge in survivors to assess realistic LVEF values beyond the acute phase of ventricular tachyarrhythmias or related acute coronary ischemia. In minor part and only if available, earlier LVEF values assessed on admission or during intensive care were retrieved from patients.
Every re-visit at the outpatient clinic or rehospitalization was documented when related to recurrent ventricular tachyarrhythmias and adverse cardiac events. Adverse cardiac events comprised acute heart failure (AHF), CPR, cardiac surgery, recurrent percutaneous coronary intervention (re-PCI), new implants or upgrades of cardiac devices, worsening or improvement of LVEF.
Documentation period lasted from index event until 2016. Documentation of all medical data was performed by independent cardiologists at the time of the patients´ individual period of clinical presentation, being blinded to final data analyses.
The present study was carried out according to the principles of the declaration of Helsinki and was approved by the medical ethics committee II of the Medical Faculty Mannheim, University of Heidelberg, Germany.
Definition of study groups, inclusion and exclusion criteria
For the present analysis, risk stratification was performed according to the presence of IHCA and OHCA as defined by current European and American guidelines [10,11,12]. OHCA group comprises patients with out of hospital ventricular tachyarrhythmias at index hospitalization, who required defibrillation or cardioversion either with or without CPR, or patients with out of hospital ventricular tachyarrhythmias and consecutive asystole requiring CPR. IHCA patients comprise hospitalized patients who developed ventricular tachyarrhythmias, which required defibrillation or cardioversion with or without CPR, or hospitalized patients who developed ventricular tachyarrhythmias and consecutive asystole requiring CPR. IHCA further comprised patients with hemodynamically stable VT on admission requiring CPR due to recurrent ventricular tachyarrhythmias during index hospitalization. Patients were allocated to the IHCA group if cardiac arrest due to ventricular tachyarrhythmias occurred after handing over from emergency physician to hospital staff.
Regarding exclusion criteria, patients without complete follow-up data regarding mortality and those not requiring CPR were excluded. In addition, patients who were not transferred to the university hospital after a cardiac arrest and patients with death during index hospitalization were excluded.
Study endpoints
The primary endpoint was all-cause mortality at 2.5 years. The overall follow-up period lasted until 2016. All-cause mortality was documented using our electronic hospital information system and by directly contacting state resident registration offices (“bureau of mortality statistics”) across Germany. Secondary endpoints were all-cause mortality at 6 months and cardiac rehospitalization within 2.5 years. Cardiac rehospitalization comprised rehospitalization due to VT, VF, AHF, acute myocardial infarction (AMI) or inappropriate ICD shock.
Statistical methods
Quantitative data are presented as mean ± standard error of mean (SEM), median and interquartile range (IQR), and ranges depending on the distribution of the data and were compared using the Student’s t test for normally distributed data or the Mann–Whitney U test for nonparametric data. Deviations from a Gaussian distribution were tested by the Kolmogorov–Smirnov test. Spearman’s rank correlation for nonparametric data was used to test univariate correlations. Qualitative data are presented as absolute and relative frequencies and compared using the Chi2 test or the Fisher’s exact test, as appropriate.
First, data of consecutive patients upon admission is given for the entire unmatched cohort in order to present the real-life character of health-care supply at our institution between 2002 and 2016. Here, multivariable Cox regression models were applied for the evaluation of the primary prognostic endpoint within the total study cohort for IHCA vs. OHCA. Multivariable Cox regression models were adjusted for the following clinically relevant covariables: age, sex, diabetes, chronic kidney disease (CKD) (glomerular filtration rate < 60 mL/min per 1.73 m2), coronary artery disease (CAD), prior HF, prior AMI, presence of AMI, left ventricular ejection fraction (LVEF) < 35% and overall ICD. Multivariable Cox regression was applied in the entire study group as well as in both subgroups of OHCA and IHCA survivors.
Second, propensity score matching was applied using data from the entire patient cohort. We used 1:1 propensity-scores for OHCA vs. IHCA to assemble matched and well-balanced subgroups. One-to-one ratio for propensity score matching was performed, including survivors of cardiac arrest and applying a non-parsimonious multivariable logistic regression model [13, 14].
Propensity scores were created according to the presence of the following independent variables: age in decades, sex, diabetes mellitus, CAD, AMI at index hospitalization, LVEF, CKD, cardiogenic shock and overall presence of ICD. Uni-variable stratification was performed using the Kaplan–Meier method with comparisons between groups using uni-variable hazard ratios (HR) given together with 95% confidence intervals.
Follow-up periods for evaluation of long-term all-cause mortality were set at 2.5 years according to the median survival time of the entire study cohort to guarantee complete follow-up of at least 50% of patients. Patients not meeting long-term follow-up were censored.
The result of a statistical test was considered significant for p < 0.05, p values ≤ 0.1 were defined as a statistical trend. SAS, release 9.4 (SAS Institute Inc., Cary, NC, USA) and SPSS (Version 25, IBM Armonk, New York, USA) were used for statistics.
Results
Study population
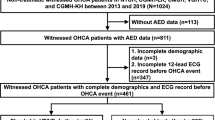
The present study retrospectively included 2.422 consecutive patients presenting with ventricular tachyarrhythmias from 2002 until 2016 (Fig. 1, flow chart). 1.279 patients were excluded without cardiac arrest, 341 OHCA and 278 IHCA patients died within index hospitalization after cardiac arrest and were, therefore, excluded for the present analysis (Fig. 1, flow chart). Lost to follow-up rate was 1.7% (n = 48) regarding survival until the end of the follow-up period.
A total of 524 patients with ventricular tachyarrhythmias and surviving cardiac arrest while being discharged from index hospitalisation were included in this study. 62% of these patients suffered from OHCA. Most patients were males in both subgroups (Table 1, left column). IHCA patients were older, had higher rates of VF compared to VT, as well as higher rates of arterial hypertension and diabetes mellitus. Rates of prior HF, prior CAD, prior AMI, chronic obstructive pulmonary disease (COPD), atrial fibrillation and stroke were higher among IHCA compared to OHCA survivors (Table 1, left column).
In OHCA patients, coronary angiography and subsequent PCI was performed more often. Higher rates of ICD implantation after cardiac arrest were present in OHCA survivors, mainly due to secondary preventative ICDs (Table 1, left column).
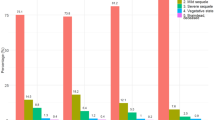
Associated diseases for cardiac arrest
Most cardiac arrests resulted from myocardial infarction (52%). Among OHCA survivors, higher rates of STEMI (44% vs. 27%; p = 0.001) as well as NSTEMI (16% vs. 10%; p = 0.070) were common. Furthermore, higher rates of cardiomyopathies, such as ischemic cardiomyopathy (8% vs. 0%; p = 0.001), DCM (3% vs. 0%; p = 0.009) and other rare cardiomyopathies (3% vs. 0%; p = 0.009) as associated diseases were present among OHCA survivors. IHCA survivors suffered more often from prolonged QT intervals (9% vs. 4%; p = 0.023), respiratory failure with consecutive hypoxia (5% vs. 2%; p = 0.017), septic shock (3% vs. 0%; p = 0.006) and pulmonary embolism (2% vs. 0%; p = 0.008). A significant amount of IHCA was associated with peri-interventional VF during coronary angiography (11% vs. 0%; p = 0.001) or operations (4% vs. 0%; p = 0.001). In 10% of all cases no associated reason for cardiac arrest was found (Table 2; Fig. 2).
Associated diseases for cardiac arrest. AV block atrioventricular block, CMP cardiomyopathy, DCM dilative cardiomyopathy, iCMP ischemic cardiomyopathy, IHCA in-hospital cardiac arrest, NSTEMI non-ST-segment-elevation myocardial infarction, OHCA out-of-hospital cardiac arrest, STEMI ST-segment-elevation myocardial infarction
Characteristics related to resuscitation
In most patients, initial rhythm was VF (93% vs. 78%; p = 0.001), which was treated with defibrillator in most cases (91% vs. 73%; p = 0.001). Median time from initiation of CPR to ROSC was higher among OHCA patients, whereas TTM was performed more frequently in patients with OHCA. Patients with IHCA were cardioverted more often (Table 3).
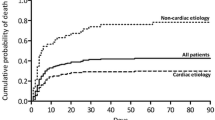
Primary and secondary endpoints
Median follow-up time was 6.3 years for OHCA survivors and 4.8 years for IHCA survivors (IQR 1616–1221 days). As shown in Table 4, left columns, IHCA survivors were associated with higher rates of all-cause mortality at 2.5 years compared to OHCA survivors (28% vs. 16%, log rank p = 0.001; HR 2.005; CI 95% 1.374–2.926; p = 0.001) (Fig. 3, left). IHCA survivors were also associated with higher rates of the secondary endpoint all-cause mortality at 6 months (14% vs. 7%, log rank p = 0.010). Cardiac rehospitalization rates at 2.5 years were equally distributed between OHCA and IHCA survivors.
Multivariable Cox regression models
After applying a multivariable Cox regression model, IHCA was still associated with the primary endpoint of all-cause mortality at 2.5 years compared to OHCA (HR 1.623; 95% CI 1.002–2.629; p = 0.049) (Table 5; right panel). Furthermore, age, CKD and impaired LVEF were associated with increased all-cause mortality, whereas AMI and the presence of an activated ICD were associated with improved survival in all survivors of cardiac arrest.
As demonstrated in Table 6, age and CKD were significant predictors of all-cause mortality at 2.5 years in OHCA survivors, whereas AMI and an activated ICD were beneficial. In IHCA survivors, only CKD was associated with increased risk of long-term all-cause mortality at 2.5 years.
Propensity-matched cohort
After using propensity-score matching for comparison of OHCA and IHCA survivors 288 matched pairs were achieved with similar baseline characteristics (Table 1, right columns).
Figure 3 (right) illustrates the increased risk for long-time all-cause mortality in IHCA patients compared to OHCA patients presenting with ventricular tachyarrhythmias on hospital admission after propensity-score matching (primary endpoint, all-cause mortality at 2.5 years: 28% vs. 19%; log-rank p = 0.045). No significant differences regarding secondary endpoints were observed after propensity-score matching (Table 4, right columns)
Discussion
This study evaluates the prognostic impact of OHCA compared to IHCA in consecutive patients presenting with ventricular tachyarrhythmias and aborted cardiac arrest and survival until hospital discharge from 2002 and 2016 at one institution.
This study suggests that patients with ventricular tachyarrhythmias represent a group with the highest risk for consecutive sudden or aborted cardiac arrest. The present study showed that IHCA is associated with higher long-term all-cause mortality at 6 months and 2.5 years. This reduced long-term survival of IHCA was even present after multivariable adjustment and propensity score matching. Therefore, this study might identify patients hospitalized due to ventricular tachyarrhythmias developing IHCA as a highest risk patient cohort being endangered of worst prognosis. Notably, since most of the cardiac arrest literature is focused on survival to admission or survival to discharge, patients with an inpatient death were excluded.
It is well known that short-term survival is more likely for IHCA patients compared to OHCA patients [8]. This might be due to the professional setting in hospitals with minimal delay from cardiac arrest to cardioversion or defibrillation and availability of diagnostic and therapeutic options, such as imaging, percutaneous coronary intervention and VT ablation [15]. Our analysis suggests that the initial survival benefit of IHCA patients might not persist as IHCA presents adverse long-term survival compared to OHCA. However, it might be speculated that not all OHCA patients had reached the hospital, possibly impacting the lower mortality among OHCA patients.
VT is often caused by a scar-related substrate due to ischemic cardiomyopathy, structural or inflammatory heart disease [10]. This can also be seen in our cohort, where among IHCA survivors greater rates of prior CAD were present and, accordingly, higher rates of VT could be detected. VF usually occurs in acute myocardial ischemia [10]. Accordingly, the present study demonstrated that OHCA survivors suffered more often from VF as substrate of ischemia during AMI, which is also reflected in higher rates of STEMI and NSTEMI as well as overall rates of CAD among OHCA survivors.
In total, cardiac related resuscitation was much more common among OHCA survivors, which is in line with current literature. Most frequent underlying pathology for OHCA is AMI, being responsible for up to 50% of all cases [16]. Interestingly, despite better intra-hospital diagnostic possibilities, IHCA revealed higher rates of unknown possible underlying cause for occurrence of ventricular tachyarrhythmias with resuscitation. Other trials investigating IHCA reported even higher rates of unknown causes for IHCA [17].
Well established predictors of adverse outcome after cardiac arrest are high lactate and high creatinine levels [3]. Accordingly, the strongest negative effect on long-term all-cause mortality in this study was the presence of CKD in both OHCA and IHCA. Recently, it was shown that the presence of CKD and, especially of renal replacement therapy, was associated with increased long-term mortality among patients with ventricular tachyarrhythmias and aborted cardiac arrest [18]. Hence, among IHCA patients lower lactate and creatinine levels were associated with higher likelihood of survival [19]. However, the latter study included only selected patients, in particular patients treated with extracorporeal cardiopulmonary resuscitation (ECPR) and comprised patients with cardiac and non-cardiac etiology of cardiac arrest [19]. Nevertheless, acute kidney injury (AKI) is common among post-resuscitated patients constituting a major risk factor not only for subsequent mortality but also for poor neurological outcome [20]. The connection between AKI and neurological outcome after resuscitation is still not clear, but it could be speculated that both reflect total ischemia time and severe chronic comorbid conditions [21]. In general, presence and severity of AKI could be used as a marker for hypoxia duration during cardiac arrest. For other acute conditions leading to kidney hypoxia, such as sepsis, cardiogenic shock or haemorrhage, this interaction is well investigated [22, 23]. Accordingly, also in this study OHCA patients revealed higher prevalence of kidney disease as a marker of prolonged ischemia time compared to IHCA patients with is also consistent with increased CPR to ROSC time among those patients. However, investigation of detailed values of lactate levels, AKI and renal replacement therapy was beyond the scope of this study.
An ICD remains the most effective treatment for primary and secondary prevention of sudden cardiac death (SCD) [24]. Interestingly, presence of an activated ICD was effective only among OHCA survivors. OHCA patients suffered significantly more often from AMI with consecutive ventricular tachyarrhythmias representing a potentially reversible disease after coronary angiography and revascularization. IHCA patients, on the other hand, suffered more often from hypoxia, sepsis and septic shock as possible underlying reason for need of resuscitation constituting a complex pathology with protracted hospitalization. Furthermore, higher rates of comorbidities such as arterial hypertension, diabetes mellitus, prior HF and CAD as well as lower cardiac interventions such as defibrillation were present among IHCA patients and OHCA survivors presented higher rates of ICD implantation after cardiac arrest. Especially increased rates of pre-existing CAD among IHCA were persistent even after propensity score matching. CAD was counted with evidence of at least one coronary arterial stenosis > 50% in at least one coronary artery or a history of percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). However, it was beyond the scope of the study to investigate the severity and distribution of CAD. Altogether, increased mortality among IHCA patients might be due to increased preexisting conditions compared to OHCA patients. In addition, univariate and multivariate analysis support this hypothesis, since mortality rates in IHCA patients were mainly driven by CKD, but not by previous existing CAD.
This study demonstrates increased long-term all-cause mortality at 2.5 years in IHCA survivors compared to OHCA survivors presenting consecutively with ventricular tachyarrhythmias on admission. Increasing all-cause mortality was already present after 6 months of follow-up. Multivariate Cox regression demonstrated an adverse effect of CKD both in OHCA and IHCA. It might be speculated, whether kidney disease may serve as a marker of hypoxia duration.
In summary, despite better in-hospital survival for IHCA patients compared to OHCA survivors, long-term prognosis of IHCA patients seems to be very poor highlighting the need for a better standardized follow-up therapy of this vulnerable patient cohort. Regarding the higher rates of long-term mortality, we propose a broad diagnostic for IHCA patients in combination with guideline-directed ICD implantation and close follow-up examinations. In addition, diagnostic and treatment of pre-existing non-cardiac conditions should move into cardiologist’s focus. However, this still needs to be reevaluated in future prospective randomized trials.
Study limitations
This observational and retrospective registry-based single centre analysis reflects a realistic picture of consecutive health-care supply of high-risk patients presenting with ventricular tachyarrhythmias. In addition, heterogeneity within the study population was controlled by a stepwise statistical approach including multivariable adjustment for several important comorbidities and risk factors, both within the entire and propensity matched cohorts. However, some factors among both groups were still present, especially increased rates of previous CAD among IHCA survivors, possibly influencing worse long-term survival, especially because decreased long-term survival was driven by prior AMI (but not by previous CAD). Furthermore, cofounding may still be present due to missing data regarding CPR (i.e., duration until return of spontaneous circulation, pH, neurological status or hypoxia). Only all-cause mortality rates were documented, detailed analyses about definite cause of death were beyond the scope of the study. Among OHCA survivors there is a survival bias, since OHCA patients must have survived both to hospital admission and to discharge without any further episode of ventricular tachyarrhythmia, whereas IHCA survivors “only” had to survive to discharge. Hospital admissions were only documented within our own institution.
Conclusions
In patients presenting with ventricular tachyarrhythmias, IHCA survivors had a higher risk for all-cause mortality after 6 months and 2.5 years compared to OHCA survivors after discharge from hospital.
References
Grasner JT, Lefering R, Koster RW, Masterson S, Bottiger BW, Herlitz J, Wnent J, Tjelmeland IB, Ortiz FR, Maurer H, Baubin M, Mols P, Hadzibegovic I, Ioannides M, Skulec R, Wissenberg M, Salo A, Hubert H, Nikolaou NI, Loczi G, Svavarsdottir H, Semeraro F, Wright PJ, Clarens C, Pijls R, Cebula G, Correia VG, Cimpoesu D, Raffay V, Trenkler S, Markota A, Stromsoe A, Burkart R, Perkins GD, Bossaert LL, Collaborators EONE (2016) EuReCa ONE-27 Nations, ONE Europe, ONE registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation 105:188–195
Tranberg T, Lippert FK, Christensen EF, Stengaard C, Hjort J, Lassen JF, Petersen F, Jensen JS, Bäck C, Jensen LO, Ravkilde J, Bøtker HE, Terkelsen CJ (2017) Distance to invasive heart centre, performance of acute coronary angiography, and angioplasty and associated outcome in out-of-hospital cardiac arrest: a nationwide study. Eur Heart J 38(21):1645–1652
Sandroni C, Nolan J, Cavallaro F, Antonelli M (2007) In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med 33(2):237–245
Nolan JP, Soar J, Smith GB, Gwinnutt C, Parrott F, Power S, Harrison DA, Nixon E, Rowan K (2014) Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation 85(8):987–992
Akintoye E, Adegbala O, Egbe A, Olawusi E, Afonso L, Briasoulis A (2020) Association between Hospital volume of cardiopulmonary resuscitation for in-hospital cardiac arrest and survival to Hospital discharge. Resuscitation 148:25–31
Girotra S, Chan PS, Bradley SM (2015) Post-resuscitation care following out-of-hospital and in-hospital cardiac arrest. Heart 101(24):1943–1949
Patil KD, Halperin HR, Becker LB (2015) Cardiac arrest: resuscitation and reperfusion. Circ Res 116(12):2041–2049
Skrifvars MB, Varghese B, Parr MJ (2012) Survival and outcome prediction using the Apache III and the out-of-hospital cardiac arrest (OHCA) score in patients treated in the intensive care unit (ICU) following out-of-hospital, in-hospital or ICU cardiac arrest. Resuscitation 83(6):728–733
Raffee LA, Samrah SM, Al Yousef HN, Abeeleh MA, Alawneh KZ (2017) Incidence, characteristics, and survival trend of cardiopulmonary resuscitation following in-hospital compared to out-of-hospital cardiac Arrest in Northern Jordan. Indian J Crit Care Med 21(7):436–441
Priori SG, Blomstrom-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, Elliott PM, Fitzsimons D, Hatala R, Hindricks G, Kirchhof P, Kjeldsen K, Kuck KH, Hernandez-Madrid A, Nikolaou N, Norekval TM, Spaulding C, Van Veldhuisen DJ (2015) 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J 36(41):2793–2867
Perkins GD, Olasveengen TM, Maconochie I, Soar J, Wyllie J, Greif R, Lockey A, Semeraro F, Van de Voorde P, Lott C, Monsieurs KG, Nolan JP (2018) European Resuscitation Council Guidelines for Resuscitation: 2017 update. Resuscitation 123:43–50
Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, Brooks SC, de Caen AR, Donnino MW, Ferrer JM, Kleinman ME, Kronick SL, Lavonas EJ, Link MS, Mancini ME, Morrison LJ, O’Connor RE, Samson RA, Schexnayder SM, Singletary EM, Sinz EH, Travers AH, Wyckoff MH, Hazinski MF (2015) Part 1: executive summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132(18 Suppl 2):S315-367
Ferdinand D, Otto M, Weiss C (2016) Get the most from your data: a propensity score model comparison on real-life data. Int J Gen Med 9:123–131
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46(3):399–424
Fredriksson M, Aune S, Bang A, Thoren AB, Lindqvist J, Karlsson T, Herlitz J (2010) Cardiac arrest outside and inside hospital in a community: mechanisms behind the differences in outcome and outcome in relation to time of arrest. Am Heart J 159(5):749–756
Geri G, Dumas F, Bonnetain F, Bougouin W, Champigneulle B, Arnaout M, Carli P, Marijon E, Varenne O, Mira JP, Empana JP, Cariou A (2017) Predictors of long-term functional outcome and health-related quality of life after out-of-hospital cardiac arrest. Resuscitation 113:77–82
Riley LE, Mehta HJ, Lascano J (2020) Single-center in-hospital cardiac arrest outcomes. Indian J Crit Care Med 24(1):44–48
Weidner K, Behnes M, Schupp T, Rusnak J, Reiser L, Taton G, Reichelt T, Ellguth D, Engelke N, Bollow A, El-Battrawy I, Ansari U, Hoppner J, Nienaber CA, Mashayekhi K, Weiss C, Akin M, Borggrefe M, Akin I (2019) Prognostic impact of chronic kidney disease and renal replacement therapy in ventricular tachyarrhythmias and aborted cardiac arrest. Clin Res Cardiol 108(6):669–682
D’Arrigo S, Cacciola S, Dennis M, Jung C, Kagawa E, Antonelli M, Sandroni C (2017) Predictors of favourable outcome after in-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation 121:62–70
Storm C, Krannich A, Schachtner T, Engels M, Schindler R, Kahl A, Otto NM (2018) Impact of acute kidney injury on neurological outcome and long-term survival after cardiac arrest—a 10year observational follow up. J Crit Care 47:254–259
Storm C, Krannich A, Schachtner T, Engels M, Schindler R, Kahl A, Otto NM (2018) Impact of acute kidney injury on neurological outcome and long-term survival after cardiac arrest—a 10 year observational follow up. J Crit Care 47:254–259
Ma S, Evans RG, Iguchi N, Tare M, Parkington HC, Bellomo R, May CN, Lankadeva YR (2019) Sepsis-induced acute kidney injury: a disease of the microcirculation. Microcirculation 26(2):e12483
Shu S, Wang Y, Zheng M, Liu Z, Cai J, Tang C, Dong Z (2019) Hypoxia and hypoxia-inducible factors in kidney injury and repair. Cells 8(3):207
Lewis GF, Gold MR (2016) Safety and efficacy of the subcutaneous implantable defibrillator. J Am Coll Cardiol 67(4):445–454
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Müller, J., Behnes, M., Schupp, T. et al. Clinical outcome of out-of-hospital vs. in-hospital cardiac arrest survivors presenting with ventricular tachyarrhythmias. Heart Vessels 37, 828–839 (2022). https://doi.org/10.1007/s00380-021-01976-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-021-01976-y