Abstract
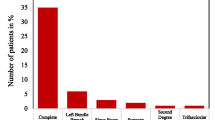
Rates of permanent pacemaker (PPM) implantation following transcatheter aortic valve implantation (TAVI) are higher than following surgery and are dependent on patient factors and valve type. There is an increasing trend towards pre-emptive PPM insertion in patients with significant conduction disease prior to TAVI. We report results from the British Cardiovascular Intervention Society (BCIS) on pre- and post-procedural PPM implantation in the TAVI population. All centres in the United Kingdom performing TAVI are required to submit data on all TAVI procedures to the National database which are then reported annually. During 2015, there were 2373 TAVI procedures in the UK. 22.4% of TAVI patients had a PPM implanted either pre-procedure (including the distant past), or during the in-hospital procedural episode. Of these, 7.9% were pre-procedure and 14.5% post-procedure. Overall PPM rates were Edwards Sapien (13.5%), Medtronic CoreValve (28.2%) and Boston Lotus (42.1%; p < 0.01). Pre-procedure pacing rates were Edwards Sapien (6.0%), Medtronic CoreValve (9.1%) and Boston Lotus (12.3%; p < 0.01). Pre-procedural pacing rates for the Boston Lotus valve have risen year-on-year from 5.8% (2013) to 8.6% (2014) to 12.3% (2015). The UK TAVI Registry demonstrates a pre-procedural permanent pacing bias amongst patients receiving transcatheter valves with higher post-procedure pacing rates. Pre-emptive permanent pacing is likely to be responsible for this difference.




Similar content being viewed by others
References
Barbanti M, Petronio AS, Ettori F, Latib A, Bedogni F, De Marco F, Poli A, Boschetti C, De Carlo M, Fiorina C, Colombo A, Brambilla N, Bruschi G, Martina P, Pandolfi C, Giannini C, Curello S, Sgroi C, Gulino S, Patanè M, Ohno Y, Tamburino C, Attizzani GF, Immè S, Gentili A, Tamburino C (2015) 5-year outcomes after transcatheter aortic valve implantation with corevalve prosthesis. JACC Cardiovasc Interv 8(8):1084–1091
Dizon JM, Nazif TM, Hess PL, Biviano A, Garan H, Douglas PS, Kapadia S, Babaliaros V, Herrmann HC, Szeto WY, Jilaihawi H, Fearon WF, Tuzcu EM, Pichard AD, Makkar R, Williams M, Hahn RT, Xu K, Smith CR, Leon MB, Kodali SK (2015) Chronic pacing and adverse outcomes after transcatheter aortic valve implantation. Heart 101(20):1665–1671
Young ML, Chilakamarri SY, Chava S, Lawrence DL (2015) Mechanisms of heart block after transcatheter aortic valve replacement–cardiac anatomy, clinical predictors and mechanical factors that contribute to permanent pacemaker implantation. Arrhythm Electrophysiol Rev 4(2):81–85
Erdogan HB, Kayalar N, Ardal H, Omeroglu SN, Kirali K, Guler M, Akinci E, Yakut C (2006) Risk factors for requirement of permanent pacemaker implantation after aortic valve replacement. J Card Surg 21(3):211–215
Keefe DL, Griffin JC, Harrison DC, Stinson EB (1985) Atrioventricular conduction abnormalities in patients undergoing isolated aortic or mitral valve replacement. Pacing Clin Electrophysiol 8(3 Pt 1):393–398
Totaro P, Calamai G, Montesi G, Barzaghi C, Vaccari M (2000) Continuous suture technique and impairment of the atrioventricular conduction after aortic valve replacement. J Card Surg 15(6):418–422
De Torres-Alba F, Kaleschke G, Diller GP, Vormbrock J, Orwat S, Radke R, Reinke F, Fischer D, Reinecke H, Baumgartner H (2016) Changes in the pacemaker rate after transition from edwards SAPIEN XT to SAPIEN 3 transcatheter aortic valve implantation: the critical role of valve implantation height. JACC Cardiovasc Interv 9(8):805–813
Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363(17):1597–1607
Ruparelia N, Latib A, Kawamoto H, Buzzatti N, Giannini F, Figini F, Mangieri A, Regazzoli D, Stella S, Sticchi A, Tanaka A, Ancona M, Agricola E, Monaco F, Spagnolo P, Chieffo A, Montorfano M, Alfieri O, Colombo A (2016) A comparison between first-generation and second-generation Transcatheter Aortic Valve Implantation (TAVI) devices: a propensity-matched single-center experience. J Invasive Cardiol 28(5):210–216
Rodríguez-Olivares R, van Gils L, El Faquir N, Rahhab Z, Di Martino LFM, van Weenen S, de Vries J, Galema TW, Geleijnse ML, Budde RPJ, Boersma E, de Jaegere PP, Van Mieghem NM (2016) Importance of the left ventricular outflow tract in the need for pacemaker implantation after transcatheter aortic valve replacement. Int J Cardiol 216:9–15
Urena M, Webb JG, Tamburino C, Munoz-Garcia AJ, Cheema A, Dager AE, Serra V, Amat-Santos IJ, Barbanti M, Imme S, Alonso Briales JH, Benitez LM, Al Lawati H, Cucalon AM, Garcia del Blanco B, Lopez J, Dumont E, De Larochelliere R, Ribeiro HB, Nombela-Franco L, Philippon F, Rodes-Cabau J (2014) Permanent pacemaker implantation after transcatheter aortic valve implantation: impact on late clinical outcomes and left ventricular function. Circulation 129(11):1233–1243
Urena M, Webb JG, Eltchaninoff H, Muñoz-García AJ, Bouleti C, Tamburino C, Nombela-Franco L, Nietlispach F, Moris C, Ruel M, Dager AE, Serra V, Cheema AN, Amat-Santos IJ, Sandoli de Brito F, Alves Lemos P, Abizaid A, Sarmento-Leite R, Ribeiro HB, Dumont E, Barbanti M, Durand E, Alonso Briales JH, Himbert D, Vahanian A, Immè S, Garcia E, Maisano F, del Valle R, Benitez LM, García del Blanco B, Gutiérrez H, Perin MA, Siqueira D, Bernardi G, Philippon F, Rodés-Cabau J (2015) Late cardiac death in patients undergoing transcatheter aortic valve replacement: incidence and predictors of advanced heart failure and sudden cardiac death. J Am Coll Cardiol 65(5):437–448
Meredith IT, Walters DL, Dumonteil N, Worthley SG, Tchétché D, Manoharan G, Blackman DJ, Rioufol G, Hildick-Smith D, Whitbourn RJ, Lefèvre T, Lange R, Müller R, Redwood S, Feldman TE, Allocco DJ, Dawkins KD (2016) 1-year outcomes with the fully repositionable and retrievable lotus transcatheter aortic replacement valve in 120 high-risk surgical patients with severe aortic stenosis: results of the REPRISE II Study. JACC Cardiovasc Interv 9(4):376–384
Siontis GC, Jüni P, Pilgrim T, Stortecky S, Büllesfeld L, Meier B, Wenaweser P, Windecker S (2014) Predictors of permanent pacemaker implantation in patients with severe aortic stenosis undergoing TAVR: a meta-analysis. J Am Coll Cardiol 64(2):129–140
Nazif TM, Dizon JM, Hahn RT, Xu K, Babaliaros V, Douglas PS, El-Chami MF, Herrmann HC, Mack M, Makkar RR, Miller DC, Pichard A, Tuzcu EM, Szeto WY, Webb JG, Moses JW, Smith CR, Williams MR, Leon MB, Kodali SK (2015) Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: the PARTNER (Placement of Aortic Transcatheter Valves) trial and registry. JACC Cardiovasc Interv 8(1):60–69
Baan J, Yong ZY, Koch KT, Henriques JPS, Bouma BJ, Vis MM, Cocchieri R, Piek JJ, de Mol BAJM (2010) Factors associated with cardiac conduction disorders and permanent pacemaker implantation after percutaneous aortic valve implantation with the corevalve prosthesis. Am Heart J 159(3):497–503
Mautner RK, Phillips JH (1980) Atrioventricular and intraventricular conduction disturbances in aortic valvular disease. South Med J 73(5):572–578
Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, Brott TG, Cohen DJ, Cutlip DE, van Es GA, Hahn RT, Kirtane AJ, Krucoff MW, Kodali S, Mack MJ, Mehran R, Rodés-Cabau J, Vranckx P, Webb JG, Windecker S, Serruys PW, Leon MB (2012) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur Heart J 33(19):2403–2418
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no financial relationships or conflicts of interest regarding the content herein. All persons gave their consent prior to inclusion in the study.
Ethical standards
All human and animal studies have been appropriately approved, in line with 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hilling-Smith, R., Smethurst, J., Cockburn, J. et al. Pre-procedural pacing bias among transcatheter aortic valves with higher post-procedure pacing rates: evidence from the UK TAVI Registry. Heart Vessels 36, 408–413 (2021). https://doi.org/10.1007/s00380-020-01703-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-020-01703-z