Abstract
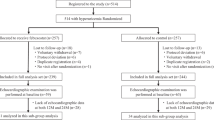
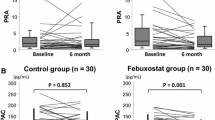
Both hypertension and hyperuricemia are closely associated with the morbidity and mortality of heart failure. This study was designed to evaluate the influences of long-term xanthine oxidase inhibitor (febuxostat) prescription on left ventricular hypertrophy (LVH), left ventricular (LV) diastolic function, and new-onset heart failure with preserved ejection fraction (HFpEF) in these patients. Using a propensity score matching of 1:2 ratio, this retrospective claims database study compared febuxosatat prescription (n = 96) and non-urate-lowering therapy (n = 192) in patients with hypertensive left ventricular hypertrophy (LVH) and asymptomatic hyperuricemia. With a follow-up of 36 months, febuxostat significantly decreased the level of serum uric acid as well as generated more prominent improvement in LVH and LV diastolic function. Besides, the new-onset symptomatic HFpEF occurred in 2 of 96 patients in febuxostat group and 13 of 192 patients in non-urate-lowering group (P = 0.091). No increased risk for major adverse cardiovascular events in patients prescribed with febuxostat was noted. In conclusion, long-term febuxostat exposure was associated with protective effects in terms of LVH or LV diastolic dysfunction in patients with hypertensive LVH and asymptomatic hyperuricemia. Febuxostat also displayed a trend for reduced risk of new-onset HFpEF in this population.


Similar content being viewed by others
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18:891–975
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C (2017) 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure. J Am Coll Cardiol 70:776–803
Fukuta H, Goto T, Wakami K, Kamiya T, Ohte N (2019) Effects of mineralocorticoid receptor antagonists on left ventricular diastolic function, exercise capacity, and quality of life in heart failure with preserved ejection fraction: a meta-analysis of randomized controlled trials. Heart Vessels 34:597–606
Biscaglia S, Ceconi C, Malagù M, Pavasini R, Ferrari R (2016) Uric acid and coronary artery disease: an elusive link deserving further attention. Int J Cardiol 213:28–32
Doehner W, Jankowska EA, Springer J, Lainscak M, Anker SD (2016) Uric acid and xanthine oxidase in heart failure—emerging data and therapeutic implications. Int J Cardiol 213:15–19
Volterrani M, Iellamo F, Sposato B, Romeo F (2016) Uric acid lowering therapy in cardiovascular diseases. Int J Cardiol 213:20–22
Gu J, Fan YQ, Zhang HL, Zhang JF, Wang CQ (2018) Serum uric acid is associated with incidence of heart failure with preserved ejection fraction and cardiovascular events in patients with arterial hypertension. J Clin Hypertens (Greenwich) 20:560–567
Gu J, Fan YQ, Bian L, Zhang HL, Xu ZJ, Zhang Y, Chen QZ, Yin ZF, Xie YS, Wang CQ (2016) Long-term prescription of beta-blocker delays the progression of heart failure with preserved ejection fraction in patients with hypertension: a retrospective observational cohort study. Eur J Prev Cardiol 23:1421–1428
Gu J, Fan YQ, Han ZH, Fan L, Bian L, Zhang HL, Xu ZJ, Yin ZF, Xie YS, Zhang JF, Wang CQ (2016) Association between long-term prescription of aldosterone antagonist and the progression of heart failure with preserved ejection fraction in hypertensive patients. Int J Cardiol 220:56–60
Sakata K, Hashimoto T, Ueshima H, Okayama A, NIPPON DATA 80 Research Group (2001) Absence of an association between serum uric acid and mortality from cardiovascular disease: NIPPON DATA 80, 1980–1994. National integrated projects for prospective observation of non-communicable diseases and its trend in the aged. Eur J Epidemiol 17:461–468
Choi HK, Atkinson K, Karlson EW, Curhan G (2005) Obesity, weight change, hypertension, diuretic use, and risk of gout in men: the health professionals follow-up study. Arch Intern Med 165:742–748
Ishizaka N, Ishizaka Y, Toda E, Nagai R, Yamakado M (2005) Association between serum uric acid, metabolic syndrome, and carotid atherosclerosis in Japanese individuals. Arterioscler Thromb Vasc Biol 25:1038–1044
Taniguchi Y, Hayashi T, Tsumura K, Endo G, Fujii S, Okada K (2001) Serum uric acid and the risk for hypertension and Type 2 diabetes in Japanese men: The Osaka Health Survey. J Hypertens 19:1209–1215
Milionis HJ, Kakafika AI, Tsouli SG, Athyros VG, Bairaktari ET, Seferiadis KI, Elisaf MS (2004) Effects of statin treatment on uric acid homeostasis in patients with primary hyperlipidemia. Am Heart J 148:635–640
Catena C, Colussi G, Capobianco F, Brosolo G, Sechi LA (2014) Uricaemia and left ventricular mass in hypertensive patients. Eur J Clin Invest 44:972–981
Liu CW, Chen KH, Tseng CK, Chang WC, Wu YW, Hwang JJ (2019) The dose-response effects of uric acid on the prevalence of metabolic syndrome and electrocardiographic left ventricular hypertrophy in healthy individuals. Nutr Metab Cardiovasc Dis 29:30–38
Cuspidi C, Facchetti R, Bombelli M, Sala C, Tadic M, Grassi G, Mancia G (2017) Uric acid and new onset left ventricular hypertrophy: findings from the PAMELA population. Am J Hypertens 30:279–285
Verdecchia P, Schillaci G, Reboldi G, Santeusanio F, Porcellati C, Brunetti P (2000) Relation between serum uric acid and risk of cardiovascular disease in essential hypertension The PIUMA study. Hypertension 36:1072–1078
Weiss K, Schär M, Panjrath GS, Zhang Y, Sharma K, Bottomley PA, Golozar A, Steinberg A, Gerstenblith G, Russell SD, Weiss RG (2017) Fatigability, exercise intolerance, and abnormal skeletal muscle energetics in heart failure. Circ Heart Fail 10:e004129
Mátyás C, Németh BT, Oláh A, Török M, Ruppert M, Kellermayer D, Barta BA, Szabó G, Kökény G, Horváth EM, Bódi B, Papp Z, Merkely B, Radovits T (2017) Prevention of the development of heart failure with preserved ejection fraction by the phosphodiesterase-5A inhibitor vardenafil in rats with type 2 diabetes. Eur J Heart Fail 19:326–336
Choi YS, de Mattos AB, Shao D, Li T, Nabben M, Kim M, Wang W, Tian R, Kolwicz SC Jr (2016) Preservation of myocardial fatty acid oxidation prevents diastolic dysfunction in mice subjected to angiotensin II infusion. J Mol Cell Cardiol 100:64–71
Shimizu T, Yoshihisa A, Kanno Y, Takiguchi M, Sato A, Miura S, Nakamura Y, Yamauchi H, Owada T, Abe S, Sato T, Suzuki S, Oikawa M, Yamaki T, Sugimoto K, Kunii H, Nakazato K, Suzuki H, Saitoh S, Takeishi Y (2015) Relationship of hyperuricemia with mortality in heart failure patients with preserved ejection fraction. Am J Physiol Heart Circ Physiol 309:H1123–H1129
Palazzuoli A, Ruocco G, De Vivo O, Nuti R, McCullough PA (2017) Prevalence of hyperuricemia in patients with acute heart failure with either reduced or preserved ejection fraction. Am J Cardiol 120:1146–1150
Gromadziński L, Januszko-Giergielewicz B, Pruszczyk P (2015) Hyperuricemia is an independent predictive factor for left ventricular diastolic dysfunction in patients with chronic kidney disease. Adv Clin Exp Med 24:47–54
Nogi S, Fujita S, Okamoto Y, Kizawa S, Morita H, Ito T, Sakane K, Sohmiya K, Hoshiga M, Ishizaka N (2015) Serum uric acid is associated with cardiac diastolic dysfunction among women with preserved ejection fraction. Am J Physiol Heart Circ Physiol 309:H986–H994
Tang ZH, Fang Z, Zeng F, Li Z, Zhou L (2013) Association and interaction analysis of metabolic syndrome and serum uric acid on diastolic heart failure. J Endocrinol Invest 36:579–583
Cingolani HE, Plastino JA, Escudero EM, Mangal B, Brown J, Pérez NG (2006) The effect of xanthine oxidase inhibition upon ejection fraction in heart failure patients: La Plata Study. J Card Fail 12:491–498
Hare JM, Mangal B, Brown J, Fisher C Jr, Freudenberger R, Colucci WS, Mann DL, Liu P, Givertz MM, Schwarz RP, Investigators OPT-CHF (2008) Impact of oxypurinol in patients with symptomatic heart failure. Results of the OPT-CHF study. J Am Coll Cardiol 51:2301–2309
Kaufman M, Guglin M (2013) Uric acid in heart failure: a biomarker or therapeutic target? Heart Fail Rev 18:177186
Kim SC, Schneeweiss S, Choudhry N, Liu J, Glynn RJ, Solomon DH (2015) Effects of xanthine oxidase inhibitors on cardiovascular disease in patients with gout: a cohort study. Am J Med 128:653.e7–653.e16
Okafor ON, Farrington K, Gorog DA (2017) Allopurinol as a therapeutic option in cardiovascular disease. Pharmacol Ther 172:139–150
Yokota T, Fukushima A, Kinugawa S, Okumura T, Murohara T, Tsutsui H (2018) Randomized trial of effect of urate-lowering agent febuxostat in chronic heart failure patients with hyperuricemia (LEAF-CHF). Int Heart J 59:976–982
Faruque LI, Ehteshami-Afshar A, Wiebe N, Tjosvold L, Homik J, Tonelli M (2013) A systematic review and meta-analysis on the safety and efficacy of febuxostat versus allopurinol in chronic gout. Semin Arthritis Rheum 43:367–375
Sezai A, Soma M, Nakata K, Hata M, Yoshitake I, Wakui S, Hata H, Shiono M (2013) Comparison of febuxostat and allopurinol for hyperuricemia in cardiac surgery patients (NU-FLASH Trial). Circ J 77:2043–2049
Liu X, Wang H, Ma R, Shao L, Zhang W, Jiang W, Luo C, Zhai T, Xu Y (2019) The urate-lowering efficacy and safety of febuxostat versus allopurinol in Chinese patients with asymptomatic hyperuricemia and with chronic kidney disease stages 3–5. Clin Exp Nephrol 23:362–370
Sezai A, Soma M, Nakata K, Osaka S, Ishii Y, Yaoita H, Hata H, Shiono M (2015) Febuxostat inhibition of endothelial-bound XO: implications for targeting vascular ROS production. Comparison of febuxostat and allopurinol for hyperuricemia in cardiac surgery patients with chronic kidney disease (NU-FLASH trial for CKD). J Cardiol 66:298–303
Malik UZ, Hundley NJ, Romero G, Radi R, Freeman BA, Tarpey MM, Kelley EE (2011) Febuxostat inhibition of endothelial-bound XO: implications for targeting vascular ROS production. Free Radic Biol Med 51:179–184
Okamoto K, Eger BT, Nishino T, Kondo S, Pai EF, Nishino T (2003) An extremely potent inhibitor of xanthine oxidoreductase. Crystal structure of the enzyme-inhibitor complex and mechanism of inhibition. J Biol Chem 278:1848–1855
Nomura J, Busso N, Ives A, Matsui C, Tsujimoto S, Shirakura T, Tamura M, Kobayashi T, So A, Yamanaka Y (2014) Xanthine oxidase inhibition by febuxostat attenuates experimental atherosclerosis in mice. Sci Rep 4:4554
Choi H, Neogi T, Stamp L, Dalbeth N, Terkeltaub R (2018) New perspectives in rheumatology: implications of the cardiovascular safety of febuxostat and allopurinol in patients with gout and cardiovascular morbidities trial and the associated food and drug administration public safety alert. Arthritis Rheumatol 70:1702–1709
Kimura K, Hosoya T, Uchida S, Inaba M, Makino H, Maruyama S, Ito S, Yamamoto T, Tomino Y, Ohno I, Shibagaki Y, Iimuro S, Imai N, Kuwabara M, Hayakawa H, Ohtsu H, Ohashi Y, FEATHER Study Investigators (2018) Febuxostat therapy for patients with stage 3 CKD and asymptomatic hyperuricemia: a randomized trial. Am J Kidney Dis 72:798–810
Zhang M, Solomon DH, Desai RJ, Kang EH, Liu J, Neogi T, Kim SC (2018) Assessment of cardiovascular risk in older patients with gout initiating febuxostat versus allopurinol: Population-Based Cohort Study. Circulation 138:1116–1126
Funding
This study was supported by Clinical Research Program of 9th People’s Hospital affiliated to Shanghai Jiaotong University School of Medicine (JYLJ201803), research projects from Shanghai Science and Technology Commission (18411950500) and Shanghai Shenkang Hospital Development Center (16CR2034B).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors confirm that there are no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pan, Ja., Lin, H., Wang, Cq. et al. Association between long-term prescription of febuxostat and the progression of heart failure with preserved ejection fraction in patients with hypertension and asymptomatic hyperuricemia. Heart Vessels 35, 1446–1453 (2020). https://doi.org/10.1007/s00380-020-01619-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-020-01619-8