Abstract
Introduction
In 2020, bladder cancer (BC) was the seventh most prevalent cancer in the world, with 5-year prevalence of more than 1.7 million cases. Due to the main risk factors—smoking and chemical exposures—associated with BC, it is considered a largely preventable and avoidable cancer. An overview of BC mortality can allow an insight not only into the prevalence of global risk factors, but also into the varying efficiency of healthcare systems worldwide. For this purpose, this study analyzes the national mortality estimates for 2020 and projected future trends up to 2040.
Materials and methods
Age-standardized mortality rates per 100,000 person-years of BC for 185 countries by sex were obtained from the GLOBOCAN 2020 database, operated by the International Agency for Research on Cancer (IARC). Mortality rates were stratified according to sex and Human Development Index (HDI). BC deaths were projected up to 2040 on the basis of demographic changes, alongside different scenarios of annually increasing, stable or decreasing mortality rates from the baseline year of 2020.
Results
In 2020, nearly three times more men died from BC than women, with more than 210,000 deaths in both sexes combined, worldwide. Regardless of gender, more than half of the total BC deaths were from countries with a very high HDI. According to our projections, while the number of deaths for men can only increase up to 54% (from 159 to around 163–245 thousand), for women it is projected to increase two- to three-fold (from 50 to around 119–176 thousand) by 2040. The burden of BC mortality in countries with a very high HDI versus high HDI appears to converge by 2040 for both sexes.
Conclusion
Opposite mortality trends by gender highlight the urgent need for immediate interventions to expand anti-tobacco strategies, especially for women. The implementation of more strict occupational health and safety regulations could also prevent exposures associated with BC. Improving the ability to detect BC earlier and access to treatment can have a significant positive impact on reducing mortality rates, minimizing economic costs, and enhancing the quality of life for patients.
Similar content being viewed by others
Introduction
In 2020, over 573 thousand new bladder cancer (BC) cases and around 212 thousand BC deaths were estimated to occur worldwide [1], representing approximately 3% of all new cancer cases and more than 2% of cancer deaths. BC ranks as the tenth most common cancer diagnosed, and the 13th most common cause of cancer mortality, worldwide and it is effectively treatable when diagnosed early with relatively high survival with 5-year relative survival rates of around 77%observed in the US [2] and 68% reported in Europe [3].
The main risk factor for BC is tobacco smoking; male smokers have a 3.3, women smokers have a 2.2 times higher risk of BC compared to nonsmokers [4], and thus is a highly avoidable cancer. Additionally, experience derived from the global smoking epidemic can be applied to obtain a better understanding of the background trends, gender differences and possible future scenarios of BC, especially in higher income settings [5, 6]. At the same time, occupational and environmental toxins may also contribute to the development of this disease [7].
This study aims to describe the burden of BC mortality across different world regions in 2020 based on GLOBOCAN estimates from the International Agency for Research on Cancer (IARC). Our paper also examines the gender-based BC mortality distribution in terms of geographic variation and Human Development Index (HDI), as well as projecting the future burden up to 2040. These disparities can express differences in healthcare systems, treatment protocols, or varying levels of access to diagnosis and treatment facilities, particularly between countries at different levels of development. Understanding these patterns can inform public health experts on ways of reducing the global burden of BC and improving health outcomes.
Materials and methods
The number of deaths from cancers of the bladder, International Classification of Diseases, 10th revision (ICD-10): C67 was extracted from the GLOBOCAN 2020 database for 185 countries or territories, by sex and 18 age groups (0–4, 5–9, 10–14…75–79, 80–84, 85, and over) [8,9,10]. Corresponding population data for 2020 were extracted from the United Nations (UN) website [11]. The data sources and hierarchy of methods used in compiling the cancer estimates have been described in detail elsewhere [9]. In brief, the GLOBOCAN estimates are assembled at the national level using the best available sources of cancer incidence and mortality data within a given country. The methods used to derive the 2020 estimates correspond to those used for previous years [12,13,14]; where applicable, priority is given to short-term predictions and modeled mortality to incidence (M:I) ratios, while validity is dependent on the degree of representativeness and quality of the source information [9].
We present tables and figures based on the estimated number of deaths, as well as two summary measures using direct standardization, namely, the age-standardized mortality rate (ASR) per 100,000 person-years based on the 1966 Segi–Doll World standard population [15, 16], and the cumulative risk of developing or dying from cancer before the age of 75 years expressed as a percentage, assuming the absence of competing causes of death [17]. These measures allow comparisons between populations adjusted for differences in age structures. We also provide a prediction of the future number of BC deaths worldwide for the year 2040 applying uniformly increasing (+ 3%, + 2%, + 1%), stable (0%), or decreasing (− 1%, − 2%, − 3%) mortality rates from the baseline year of 2020 to the estimations of UN population data.
The possible impact of the COVID-19 pandemic was not taken into consideration in the calculations. The results are presented by country, and aggregated, across 20 UN-defined world regions [11], and according to the UN’s four-tier Human Development Index (HDI) in 2020 [18], the latter being a means to assess the cancer burden at varying levels of development (low, medium, high and very high HDI). Throughout we use the terms transitioning, emerging and lower HDI countries/economies as synonyms for nations classified as low or medium HDI, and transitioned or higher HDI countries/economies for those classified as high or very high HDI.
The Global Cancer Observatory (GCO, https://gco.iarc.fr) includes facilities for the tabulation and graphical visualization of the GLOBOCAN database, including explorations of the current [8] and future [19] burden for 36 cancer types, and all cancers combined, including non-melanoma skin cancer (ICD-10 C44 excluding basal cell carcinomas).
Results
Bladder cancer mortality—national rankings 2020
According to the GLOBOCAN estimates for 2020, nearly three times more men died due to BC than women worldwide, with more than 210 thousand deaths combined (Table 1).
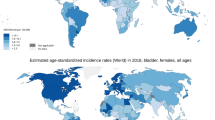
Male (age-standardized) mortality rates are the highest in Northern Africa and Eastern Europe (especially Egypt, with rates of more than 14 per 100,000 and Slovakia, at nearly 10 per 100,000), Southern Europe (particularly Cyprus) and Western Asia, while rates are the lowest in Western and Middle Africa, and Central America (Figs. 1 and 2). Female mortality rates are the highest in Northern Africa, Northern Europe, Eastern Africa, and Western Europe, specifically Egypt, Denmark, Malawi, and the Netherlands, respectively. Somewhat lower rates are observed in South-Eastern Asia, Central America, and Southern Asia. Gender differences, are the greatest in Northern Africa, Eastern Europe, Western Asia, and Southern Europe, and the smallest differences observed in Central America and Middle and Western Africa.
Bladder cancer mortality burden by 2040
If the current mortality rates were to remain constant over the next two decades i.e., assuming the 0% forecast scenario, nearly 300 thousand male BC deaths are predicted to occur in 2040, compared to 159 thousand in 2020 (Fig. 3). For women, the corresponding deaths are approximately a third of their male counterparts, yielding a predicted increase from 50,000 deaths in 2020 to around 100 thousand in 2040. The projection also considered varying rates of change between − 3% and + 3% per year for BC mortality. Considering the presumed scenarios of the smoking epidemic in the short-term future, a significant increase in BC mortality for women is to be expected, compared to a general decline in men’s figures, with national or regional exceptions. The projected number of BC deaths among men will likely range between 163 and 245 thousand (scenarios with decreasing rates of change at − 3%, − 2%, − 1% per year) and for women between 119 and 176 thousand (scenarios with increasing rates of change at 1%, 2%, 3% per year) by 2040. Under all scenarios, the burden of BC mortality in very high versus high HDI countries will converge noticeably for both sexes by 2040. The disease burden in medium- and low-HDI countries is expected to remain low.
Discussion
Our study reports the current mortality status of BC worldwide and describes its increasing global burden up to 2040 by sex and HDI levels based on demographic projections.
Due to the association between smoking and BC, the global smoking epidemic serves as useful input to our understanding of the present and future epidemiology of BC. While smoking prevalence for men has been declining in high and very high-income settings, e.g., in Northern America, Europe and Australia, and New Zealand concerns remain among women in low-income countries (for instance mostly in Asian and African countries) where presently low levels of cigarette consumption are already on the rise. In an era where women’s spending power is increasing, cigarettes are becoming affordable and women are more exposed to the marketing strategies of tobacco companies, in an environment where cultural constraints are weakening and female-specific quitting programs are rare [20,21,22].
Women are typically diagnosed with more advanced cancer and have a worse prognosis than men [23]. Reasons for this may be anatomical differences, different time lags from first symptoms to diagnosis and variations in hormone receptors [24]. However, women were more likely to be treated for voiding complaints or possible urinary tract infections without further evaluation or referral to urology than men [25]. As a result, a higher proportion of women may appear in the healthcare system with more advanced stage and more extensive metastases [26]. Other researchers suggest that hormonal factors, such as menopausal status and age at menopause, alongside smoking, may play a role in modifying BC risk among women [27]. All of this contributes to a further closing of the gender gap in BC mortality in future for high and very high-income HDI settings: as reported by our study, while the number of deaths for men could only increase by about 50%, for women, it could double or triple by 2040, according to the most probable scenarios, calculated with decreasing annual percentages of mortality change: − 3%, − 2%, − 1% per year for men and increasing by + 1%, + 2%, + 3% per year for women.
Besides tobacco consumption, occupational or environmental toxins may also contribute greatly to the burden of this disease. A previous cohort study from Denmark investigated how air, sea and ground pollution caused by a chemical factory contributed to an increased cancer risk [28]. Exposure to aromatic amines and other chemicals affecting workers in the painting, rubber, or aluminum industries have been confirmed as risk factors of bladder cancer [29]. Moreover according to an EU-wide investigation, long-term exposure to disinfection by-products in drinking water (trihalomethanes) has been consistently associated with an increased risk of BC [30]. In summary, the main risk factor for BC is tobacco smoking, which is responsible for more than half of BC cases and occupational or environmental toxins contributing to approximately one-fifth of all cases [31]. However, the precise proportion can be difficult to estimate as BC develops decades after exposure, even if the exposure only lasted several years. Schistosomiasis infection is also a common cause of this disease triggering related squamous cell carcinoma in regions of Africa and the Middle East, which infers a poorer prognosis in comparison to urothelial carcinoma. With approximately four-fifth of cases attributable to known modifiable risk factors, BC can be considered as largely preventable and greatly benefit from targeted prevention strategies [31].
Differences in healthcare systems, treatment protocols, or varying levels of access to diagnosis and treatment facilities, particularly between countries at different levels of development, can also partly explain the differences observed in BC survival and mortality rates between countries [3, 32]. Furthermore, BC is one of the most challenging and expensive cancers to diagnose and treat: its diagnosis relies on cystoscopy, an invasive and expensive procedure that might not be easily accessible in low-resource settings [23, 33]. In light of these facts, one result of our research has particular importance: the decreasing difference of the BC mortality burden between very high versus high HDI countries. Reasons for this could include the aging population, changing behaviors in tobacco consumption, the modification of other risk factors and diversity in treatment availability, where generally, very high HDI countries have better regulations and enforcement of environmental standards than lower HDI countries. Further in-depth researches would be necessary to examine and reveal the exact role of these factors, because most of them (e.g., impact of smoking or environmental risk factors) were not applied in our prediction model. In addition, the modest changes indicated by our projections in medium and low-HDI countries may be misleading, because these can be influenced to a large degree by the changing exposure to tobacco consumption and environmental hazards.
Various social–political interventions might alleviate the global burden of BC in future. The end of smoking may be achieved with well-known anti-smoking strategies, such as raising the value-added tax (VAT), a gradual ban on cigarette use in the community, and effectively targeted anti-cigarette campaigns, can significantly decrease the risk of BC [31]. In order to achieve this, it would be particularly necessary to target women around the world, especially in middle- and low-income populations. Besides this, stricter occupational health, safety regulations and the right targeting of preventive interventions could also reduce exposures which can cause BC.
Improving the ability to detect, for example through improving access to cystoscopy, and monitor BC can have a significant positive impact on reducing mortality rates, minimizing economic costs, and enhancing the quality of life for patients. Women should be a target population, as they generally are more likely to receive a diagnosis at advanced stages and have a poor prognosis.
The limitations of this study include the wide degree of variability in local data recording practices and the quality of BC causes of death data from death registries i.e., low rates observed in some regions could reflect difficulties in ascertaining and certifying causes of death. For instance, most African and some Asian countries have weak mortality statistics systems. In GLOBOCAN, in countries where mortality series were not available from national vital registration sources, the predominant means of the estimation of rates were from corresponding national incidence estimates via modeling, using incidence-to-mortality ratios derived from cancer registries in neighboring countries. However, higher rates in other regions may be affected to an unknown extent by the proportion of autopsies performed among the deceased. Our prediction model does not consider the changing smoking prevalence in the past as a key determinant of present and future BCs. However, we provide possible scenarios on the basis of uniform increases or decreases in rates that may help provide a realistic overview of the changing future burden of BC.
Conclusion
BC is a significant public health issue globally, with mortality rates showing geographical variation and higher rates among men than women at present. However, estimates indicate that mortality rates will increase for women in the future, with the burden of BC in high HDI countries converging to very high HDI countries for both men and women. Treatment protocols, healthcare systems, and access to diagnosis and treatment facilities can partly explain the differences observed in BC survival and mortality rates between different regions. This study recommends social and political interventions to alleviate the global burden of BC in future. It suggests smoking cessation according to well-known anti-smoking strategies and campaigns, and effective workplace safety practices. Improving the ability to detect, monitor and treat BC can have a significant positive impact on reducing mortality rates, minimizing economic costs, and enhancing the quality of life for patients.
Data availability
Data are available in a public, open access repository.
References
Cancer Today (n.d.). http://gco.iarc.fr/today/home. Accessed April 13, 2022
Survival Rates for Bladder Cancer (n.d.). https://www.cancer.org/cancer/bladder-cancer/detection-diagnosis-staging/survival-rates.html. Accessed May 20, 2021
Marcos-Gragera R, Mallone S, Kiemeney LA, Vilardell L, Malats N, Allory Y, Sant M, Hackl M, Zielonke N, Oberaigner W, Van Eycken E, Henau K, Valerianova Z, Dimitrova N, Sekerija M, Zvolský M, Dušek L, Storm H, Engholm G, Mägi M, Aareleid T, Malila N, Seppä K, Velten M, Troussard X, Bouvier V, Launoy G, Guizard AV, Faivre J, Bouvier AM, Arveux P, Maynadié M, Woronoff AS, Robaszkiewicz M, Baldi I, Monnereau A, Tretarre B, Bossard N, Belot A, Colonna M, Molinié F, Bara S, Schvartz C, Lapôtre-Ledoux B, Grosclaude P, Meyer M, Stabenow R, Luttmann S, Eberle A, Brenner H, Nennecke A, Engel J, Schubert-Fritschle G, Kieschke J, Heidrich J, Holleczek B, Katalinic A, Jónasson JG, Tryggvadóttir L, Comber H, Mazzoleni G, Bulatko A, Buzzoni C, Giacomin A, Sutera Sardo A, Mazzei A, Ferretti S, Crocetti E, Manneschi G, Gatta G, Sant M, Amash H, Amati C, Baili P, Berrino F, Bonfarnuzzo S, Botta L, Di Salvo F, Foschi R, Margutti C, Meneghini E, Minicozzi P, Trama A, Serraino D, Zucchetto A, De Angelis R, Caldora M, Capocaccia R, Carrani E, Francisci S, Mallone S, Pierannunzio D, Roazzi P, Rossi S, Santaquilani M, Tavilla A, Pannozzo F, Busco S, Bonelli L, Vercelli M, Gennaro V, Ricci P, Autelitano M, Randi G, Ponz De Leon M, Marchesi C, Cirilli C, Fusco M, Vitale MF, Usala M, Traina A, Zarcone M, Vitale F, Cusimano R, Michiara M, Tumino R, Giorgi Rossi P, Vicentini M, Falcini F, Iannelli A, Sechi O, Cesaraccio R, Piffer S, Madeddu A, Tisano F, Maspero S, Fanetti AC, Zanetti R, Rosso S, Candela P, Scuderi T, Stracci F, Rocca A, Tagliabue G, Contiero P, Dei Tos AP, Tognazzo S, Pildava S, Smailyte G, Calleja N, Micallef R, Johannesen TB, Rachtan J, Gózdz S, Mezyk R, Blaszczyk J, Kepska K, Bielska-Lasota M, Forjaz de Lacerda G, Bento MJ, Antunes L, Miranda A, Mayer-da-Silva A, Nicula F, Coza D, Safaei Diba C, Primic-Zakelj M, Almar E, Mateos A, Errezola M, Larrañaga N, Torrella-Ramos A, Díaz García JM, Marcos-Navarro AI, Marcos-Gragera R, Vilardell L, Sanchez MJ, Molina E, Navarro C, Chirlaque MD, Moreno-Iribas C, Ardanaz E, Galceran J, Carulla M, Lambe M, Khan S, Mousavi M, Bouchardy C, Usel M, Ess SM, Frick H, Lorez M, Ess SM, Herrmann C, Bordoni A, Spitale A, Konzelmann I, Visser O, Aben K, Coleman M, Allemani C, Rachet B, Verne J, Easey N, Lawrence G, Moran T, Rashbass J, Roche M, Wilkinson J, Gavin A, Fitzpatrick D, Brewster DH, Huws DW, White C, Otter R (2015) Urinary tract cancer survival in Europe 1999–2007: results of the population-based study EUROCARE-5. Eur J Cancer 51:2217–2230. https://doi.org/10.1016/j.ejca.2015.07.028
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health, The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General, Centers for Disease Control and Prevention (US), Atlanta (GA), 2014. http://www.ncbi.nlm.nih.gov/books/NBK179276/. Accessed April 14, 2022
Lopez AD, Collishaw NE, Piha T (1994) A descriptive model of the cigarette epidemic in developed countries. Tob Control 3:242–247. https://doi.org/10.1136/tc.3.3.242
Thun M, Peto R, Boreham J, Lopez AD (2012) Stages of the cigarette epidemic on entering its second century. Tob Control 21:96–101. https://doi.org/10.1136/tobaccocontrol-2011-050294
Jubber I, Ong S, Bukavina L, Black PC, Compérat E, Kamat AM, Kiemeney L, Lawrentschuk N, Lerner SP, Meeks JJ, Moch H, Necchi A, Panebianco V, Sridhar SS, Znaor A, Catto JWF, Cumberbatch MG (2023) Epidemiology of bladder cancer in 2023: a systematic review of risk factors. Eur Urol 84:176–190. https://doi.org/10.1016/j.eururo.2023.03.029
Jacques Ferlay, Morten Ervik, Frederik Lam, Murielle Colombet, Les Mery, Marion Pineros, Ariana Znaor, Isabelle Soerjomataram, Freddie Bray, Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer (n.d.). https://gco.iarc.fr/today
Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Piñeros M, Znaor A, Bray F (2021) Cancer statistics for the year 2020: an overview. Int J Cancer 149:778–789. https://doi.org/10.1002/ijc.33588
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
UNSD—Methodology (n.d.). https://unstats.un.org/unsd/methodology/m49/. Accessed April 15, 2022
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, Znaor A, Bray F (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 144:1941–1953. https://doi.org/10.1002/ijc.31937
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359-386. https://doi.org/10.1002/ijc.29210
Ferlay J, Shin H-R, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127:2893–2917. https://doi.org/10.1002/ijc.25516
Cancer Mortality for Selected Sites in 24 Countries (1950–57)—ScienceOpen (n.d.). https://www.scienceopen.com/document?vid=d36053cb-ebfe-4b4c-a7ca-05447aa3cd19. Accessed April 15, 2022
Schneiderman MA (1968) Cancer incidence in five continents: a technical report. In: Doll R, Payne P, Waterhouse J (eds) Springer, New York, 1966. 244 pp. $9.50, Cancer Research, 28 (1968) 804
Day NE (1992) Cancer incidence in five continents. Cumulative rate and cumulative risk, IARC Sci Publ., pp 862–864
Human Development Reports | United Nations Development Programme (n.d.). https://hdr.undp.org/. Accessed April 15, 2022
Jacques Ferlay, Mathieu Laversanne, Morten Ervik, Frederik Lam, Murielle Colombet, Les Mery, Marion Pineros, Ariana Znaor, Isabelle Soerjomataram, Freddie Bray, Global Cancer Observatory: Cancer Tomorrow (n.d.). https://gco.iarc.fr/tomorrow
Amos A (1996) Women and smoking. Br Med Bull 52:74–89. https://doi.org/10.1093/oxfordjournals.bmb.a011534
Amos A, Haglund M (2000) From social taboo to “torch of freedom”: the marketing of cigarettes to women. Tob Control 9:3–8. https://doi.org/10.1136/tc.9.1.3
Wensink M, Alvarez J-A, Rizzi S, Janssen F, Lindahl-Jacobsen R (2020) Progression of the smoking epidemic in high-income regions and its effects on male-female survival differences: a cohort-by-age analysis of 17 countries. BMC Public Health 20:39. https://doi.org/10.1186/s12889-020-8148-4
International Agency for Research on Cancer, Improving Early Detection and Clinical Management of Bladder Cancer—A promising urine test (uTERTpm) (2022). https://www.iarc.who.int/wp-content/uploads/2022/05/IARC_Evidence_Summary_Brief_3.pdf
Wolff I, Brookman-May S, May M (2015) Sex difference in presentation and outcomes of bladder cancer: Biological reality or statistical fluke? Curr Opin Urol 25:418. https://doi.org/10.1097/MOU.0000000000000198
Henning A, Wehrberger M, Madersbacher S, Pycha A, Martini T, Comploj E, Jeschke K, Tripolt C, Rauchenwald M (2013) Do differences in clinical symptoms and referral patterns contribute to the gender gap in bladder cancer? BJU Int 112:68–73. https://doi.org/10.1111/j.1464-410X.2012.11661.x
Bladder Cancer Survival: Women Better off in the Long Run—Science Direct (n.d.). https://www.sciencedirect.com/science/article/pii/S0959804918307081?via%3Dihub. Accessed March 13, 2023
McGrath M, Michaud DS, De Vivo I (2006) Hormonal and reproductive factors and the risk of bladder cancer in women. Am J Epidemiol 163:236–244. https://doi.org/10.1093/aje/kwj028
Lynge E, Holmsgaard HA, Holmager TLF, Lophaven S (2021) Cancer incidence in Thyborøn-Harboøre, Denmark: a cohort study from an industrially contaminated site. Sci Rep 11:13006. https://doi.org/10.1038/s41598-021-92446-y
Preventable Exposures Associated With Human Cancers | JNCI: Journal of the National Cancer Institute | Oxford Academic (n.d.). https://academic.oup.com/jnci/article/103/24/1827/937010. Accessed March 15, 2023
Evlampidou I, Font-Ribera L, Rojas-Rueda D, Gracia-Lavedan E, Costet N, Pearce N, Vineis P, Jaakkola JJK, Delloye F, Makris KC, Stephanou EG, Kargaki S, Kozisek F, Sigsgaard T, Hansen B, Schullehner J, Nahkur R, Galey C, Zwiener C, Vargha M, Righi E, Aggazzotti G, Kalnina G, Grazuleviciene R, Polanska K, Gubkova D, Bitenc K, Goslan EH, Kogevinas M, Villanueva CM (2020) Trihalomethanes in drinking water and bladder cancer burden in the European Union. Environ Health Perspect 128:017001. https://doi.org/10.1289/EHP4495
Saginala K, Barsouk A, Aluru JS, Rawla P, Padala SA, Barsouk A (2020) Epidemiology of bladder cancer. Med Sci 8:15. https://doi.org/10.3390/medsci8010015
Leal J, Luengo-Fernandez R, Sullivan R, Witjes JA (2016) Economic burden of bladder cancer across the European Union. Eur Urol 69:438–447. https://doi.org/10.1016/j.eururo.2015.10.024
Sievert KD, Amend B, Nagele U, Schilling D, Bedke J, Horstmann M, Hennenlotter J, Kruck S, Stenzl A (2009) Economic aspects of bladder cancer: What are the benefits and costs? World J Urol 27:295–300. https://doi.org/10.1007/s00345-009-0395-z
Acknowledgements
The project was implemented with the support from the National Research, Development and Innovation Fund of the Ministry of Culture and Innovation under the National Laboratories Program [National Tumor Biology Laboratory (2022-2.1.1-NL-2022-00010)] and the Hungarian Thematic Excellence Program (under project TKP2021-EGA-44) Grant Agreements with the National Research, Development and Innovation Office.
Funding
Open access funding provided by National Institute of Oncology. Where authors are identified as personnel of the International Agency for Research on Cancer/World Health Organization, the authors alone are responsible for the views expressed in this article, and they do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer/World Health Organization.
Author information
Authors and Affiliations
Contributions
AW: literature search, data analysis, writing – original draft; JV: methodology, figures, visualization; RS: writing—review and editing; EM: writing—review and editing; ML: methodology, figures, visualization; PN: writing—review and editing, funding acquisition; IK: writing—review and editing; AZ: writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethics approval
This study does not involve human participants and animal subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wéber, A., Vignat, J., Shah, R. et al. Global burden of bladder cancer mortality in 2020 and 2040 according to GLOBOCAN estimates. World J Urol 42, 237 (2024). https://doi.org/10.1007/s00345-024-04949-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-04949-8