Abstract
Purpose
This study aims to investigate urinary symptoms (continence and stoma care), health-related quality of life (HRQoL) and psychosocial distress (PD) in the early postoperative period after radical cystectomy (RC) and urinary diversion for ileal conduit (IC) and ileal neobladder (INB) to obtain a better basis for patient counseling.
Methods
Data for 842 bladder cancer patients, who underwent 3 weeks of inpatient rehabilitation (IR) after RC and urinary diversion (447 IC, 395 INB) between April 2018 and December 2019 were prospectively collected. HRQoL, PD, and urinary symptoms were evaluated by validated questionnaires at the beginning (T1) and the end of IR (T2). In addition, continence status and micturition volume were objectively evaluated in INB patients by 24-h pad test and uroflowmetry, respectively.
Results
Global HRQoL was severely impaired at T1, without significant difference between the two types of urinary diversion. All functioning and symptom scales of HRQoL improved significantly from T1 to T2. In INB patients, all continence parameters improved significantly during IR, while patients with an IC reported fewer problems concerning urostomy management. The proportion of patients suffering from high PD decreased significantly from 50.7 to 34.9%. Age ≤ 59 years was the only independent predictor of high PD. Female patients and patients ≤ 59 years were more likely to use individual psycho-oncological counseling.
Conclusion
HRQoL, PD and urinary symptoms improved significantly in the early recovery period after RC. Patients with urinary continence reported higher HRQoL and less PD. Psychosocial support should be offered especially to younger patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical cystectomy (RC) has seen an increase of 28% in cases between 2006 and 2019 in Germany. Ileal conduit (IC) and ileal neobladder (INB) are the most common types of urinary diversion [1]. Up to 35% of patients show clinical symptoms of depression after RC and are more likely to commit suicide than the general population [2, 3]. But even before surgery, up to 45% of patients suffer from high psychosocial distress (PD). Advanced tumor stage was associated with high distress, while sex, age, and type of urinary diversion were not identified as predictors of high PD in patients with bladder cancer [4, 5].
In patients with an INB, urinary continence is an independent prognostic factor for a high quality of life (QoL) post-surgery, while incontinence may lead to impaired emotional function [6, 7]. Data comparing QoL in patients with an INB and an IC is conflicting [8,9,10]. Overall, RC leads to a diminished body image, but patients with an INB are usually more content with their choice of urinary diversion [11]. Health-related QoL (HRQoL) has been identified to predict overall survival in several tumor entities [12, 13].
Supporting patients for reaching the important goal of reintegration into daily life, German social laws entitle cancer patients to an average of three weeks of inpatient rehabilitation (IR). The guideline of the German Society of Urology recommends that all patients be offered several weeks of IR after RC for bladder cancer to minimize functional disorders, reduce PD and improve HRQoL [14]. The design of our study allows us to report on urinary symptoms, QoL and PD in the early postoperative period in a large number of patients after RC in a recent period and in a multi-institutional approach.
Methods
This prospective study is based on clinical data of patients with urothelial carcinoma of the bladder who underwent RC with creation of IC or INB in various hospitals across Germany and who were treated in a specialized center for urological rehabilitation (Kliniken Hartenstein, Bad Wildungen, Germany) between April 2018 and December 2019. The study protocol was approved by an institutional research committee (research authorization number FF30/2017). At the beginning (T1) and the end (T2) of IR, HRQoL, PD and, urinary symptoms were measured by validated questionnaires (EORTC QLQ-C30, EORTC QLQ-BLM30, QSC-R10, ICIQ-SF; Supplement 1). Furthermore, incontinence and micturition volume in patients after creation of an INB were objectively assessed by 24-h pad test and uroflowmetry, respectively. Social continence was defined as the use ≤ 1 pad per 24 h. Baseline characteristics comprised patients’ age, Karnofsky performance status, body mass index (BMI), the existence of cardiovascular disease and/or diabetes, tumor stage, method of surgery and utilization of neoadjuvant chemotherapy. Since age is known to influence functional outcomes (e.g., urinary continence) and PD, patients were categorized in three age categories (≤ 59; 60–69; ≥ 70 years) [15,16,17]. Normative data on the HRQoL of the general German population were used for comparison [18].
Inpatient rehabilitation (IR)
During IR, patients were treated daily by specialized nurses and physiotherapists regarding urinary continence and stoma care, respectively. The multimodal continence therapy includes osteopathic physiotherapy, external urethral sphincter exercises, and educational training on neobladder management and care (e.g., micturition diary with instruction to empty the neobladder initially every 2–3 h during the day as well as at night; careful increase of neobladder volume to achieve sensitivity concerning neobladder volume; and prevention of residual urine volume with special mechanisms for emptying the [19] neobladder). Osteopathic physiotherapy is based on three pillars: (a) visceral techniques to lower intraabdominal pressure and increase arterial circulation and venous and lymphatic drainage, respectively, (b) parietal techniques for myofascial relaxation, and (c) craniosacral techniques aiming at neuronal plasticity resulting in improved function of the external urethral sphincter. Therapy sessions consist of a kinesthetic treatment followed by specific sensorimotor training enabling the patient to differentiate between muscle groups of the pelvis and to isolate the external urethral sphincter. For patients without improvement in daytime continence within 2 weeks of therapy, video-assisted biofeedback-sphincter training via transurethral endoscopy may be performed [15]. Pressure spikes in the reservoir due to increased nightly peristalsis have been identified as one cause of nocturnal urinary incontinence [19]. Patients suffering from severe nocturnal incontinence were, therefore, given anticholinergic drugs at night to reduce neobladder peristalsis [20]. Psychosocial interventions were carried out by physicians, nurses, physiotherapists, psychologists, and social workers. The program includes information on bladder cancer and aftercare, individual, group, and couple psychotherapy, relaxation training, and psychoeducation.
Statistical analysis
Descriptive statistics for categorical variables included frequencies and proportions, while for continuous variables, medians and interquartile ranges (IQR) or means and standard deviations (SD) were reported. Between-group comparisons were analyzed using the Mann–Whitney U test or Chi-square test (Pearson) as appropriate. The Wilcoxon test was used to compare changes in quantitative variables, while the Chi-square test (McNemar) was used to compare changes in proportions. Multivariable logistic regression analyses were performed to identify predictors of high distress or use of individual psychotherapy. Significance was considered at p < 0.05. Data were analyzed by SPSS version 29.0 (IBM, Chicago).
Results
A total of 842 bladder cancer patients underwent IR after RC and urinary diversion (447 IC, 395 INB) in 135 different hospitals in Germany. This being a German cohort, Hautmann INB was chosen in most patients [21]. IR started at a median of 28 days (interquartile range (IQR) 23–35) and ended with a median of 54 days (IQR 48–62) after surgery. The median age was 68 years (IQR 62–75). Men were significantly more likely to receive an INB (52.3 vs 47.7%, p < 0.001), while women were far more likely to receive an IC (76.1% vs 23.9%, p < 0.001). Patients with an IC were significantly older than patients with an INB (73 years (IQR 67–78) vs 64 years (IQR 58–69); p < 0.001). Furthermore, locally advanced disease (≥ pT3; 41.4% vs 24.1%; p < 0.001) and lymph node metastases (19.9% vs 11.8%; p = 0.002) were significantly more often present in patients with an IC (Table 1).
Urinary continence (Table 2)
Median loss of urine per 24 h decreased by 55% (440 g (IQR 94–1131) vs 199 g (IQR 21–645); p < 0.001), while median micturition volume increased by 71% (115 ml (IQR 31–176) vs 197 ml (IQR 101–290); p < 0.001) during IR. Median ICIQ-scores significantly decreased during IR (15 (IQR 12–18) vs 11 (IQR 8–15); p < 0.001). The percentage of patients with social continence increased from 19.8% at T1 to 33.0% at T2 (p < 0.001). At T2, compared to incontinent patients, patients with social continence reported higher global HRQoL (mean 61.2 vs 53.5; p < 0.001) and lower PD (median 7 vs 9; p = 0.030). Data on continence differentiated by sex can be found in Supplement 2a-b.
Quality of life
EORTC QLQ-C30
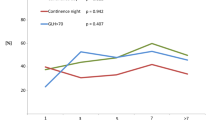
Mean global HRQoL was significantly impaired at T1, but improved significantly during IR (39.7 vs 55.8; p < 0.001). No significant differences were detected between the two types of urinary diversion at both timepoints. All functioning scales (physical, role, emotional, cognitive and social functioning) improved significantly from T1 to T2 (Table 3). Significant improvements were also detected in all symptom scales and single items except financial difficulties. Patients with an IC were more impacted by fatigue, nausea and vomiting, and constipation at T1 and T2. Meanwhile, patients with an INB suffered significantly more from financial difficulties at both T1 and T2 (Supplement 3).
EORTC QLQ-BLM30
Both micturition problems (61.1 vs 45.3; p < 0.001) and urostomy care (38.4 vs 27.9; p < 0.001) improved significantly during IR. At T2, 82.8% of patients were autonomously managing their urostomy vs 32.7% at T1 (p < 0.001). Future perspective, abdominal bloating/flatulence, and self-esteem/body image all improved significantly in the whole cohort. At T2, patients with an IC were more concerned regarding the future than patients with an INB (47.7 vs 42.8; p = 0.043) and suffered more from abdominal bloating and flatulence at both T1 (43.6 vs 36.7; p < 0.001) and T2 (31.3 vs 26.3; p = 0.003). Results of QLQ-BLM30 domains can be found in Supplement 4.
Psychosocial distress (QSC-R10)
PD decreased significantly during IR (15 points (IQR 8–23) vs 10 points (IQR 4–18); p < 0.001). The proportion of patients suffering from high PD (QSC-R10 ≥ 15 points) decreased significantly from 50.7% at T1 to 34.9% at T2 (p < 0.001). Patients with an INB were significantly more likely to receive individual psychological treatment during IR (41.3% vs 34.5%; p = 0.042). Results of the QSC-R10 are shown in Supplement 5.
Multivariable logistic regression analysis identified age ≤ 59 years as the only independent predictor for high PD (odds ratio (OR) 2.198; 95% confidence interval (CI) 1.472–3.282; p < 0.001) at T1. Age ≤ 59 years (OR 1.964; 95% CI 1.330–2.899; p < 0.001) and female sex (OR 1.799; 95% CI 1.236–2.616; p = 0.002) were identified as independent predictors for the use of psychological counseling during IR (Table 4). Type of urinary diversion, surgical approach (open vs. robot assisted), neoadjuvant chemotherapy, tumor stage ≥ pT3, and presence of lymph node metastases did neither predict high PD nor use of psychologic counseling during IR.
Discussion
Our contemporary, prospective study of 842 bladder cancer patients from 135 primary hospitals from all over Germany reveals a moderate to high impairment of HRQoL in the early postoperative period after RC and urinary diversion [18, 22]. These results contradict data from an American single high-volume tertiary center, which did not reveal a strong decrease of HRQoL in a follow-up period of 3 to 24 months after RC and urinary diversion [23]. Fortunately, in our cohort, all functioning and symptom scales of HRQoL improved significantly during IR, but remained diminished nonetheless. Lower HRQoL and impaired physical and emotional functioning in the early postoperative period have been reported by Singer et al. [24]. According to a recent study by Abozaid et al., recovery of both symptom and functioning scales can be expected within 6 and 12 months, respectively [25]. A higher incidence of diarrhea in INB patients and constipation in patients with an IC were also reported by Tyson et al. [26]. A higher burden of financial worries in patients with an INB may sufficiently be explained by their mean younger age. Since a successful return to work after cancer therapy signals successful disease management and may alleviate financial difficulties, employment after cancer therapy is linked to higher HRQoL [27, 28]. Results related to QoL should be interpreted with caution, as the patient cohorts are heterogenous in terms of baseline characteristics. Our cohort mostly underwent open RC (89.0%). Recent data from a prospective randomized single-center trial comparing open RC and robot-assisted RC have shown that HRQoL does not differ between surgical approaches [29]. A bias in our results due to an overrepresentation of patients after more invasive open RC remains possible, but appears to be unlikely.
Urinary continence after the creation of an INB is an important factor for good HRQoL [6, 7]. The assessment of urinary continence after creation of an INB mainly occurs ≥ 1 year after RC and usually includes pad use and incontinence questionnaires [30]. At this point, up to 90% of patients report using ≤ 1 pad/24 h [31]. In our cohort, urinary continence improved significantly during IR. A recent study by our group highlighted the significant influence of younger age and nerve-sparing surgery and the absence of diabetes mellitus or obesity on early continence after creation of an INB [15]. However, female patients still suffer from severe urinary incontinence both at the end of IR, which is consistent with the literature [32]. The importance of urinary continence is further highlighted by patients with social continence reporting both improved HRQoL and lower PD at the end of IR. In this cohort, 27.3% of men and 44.0% of women reported persistent severe urinary incontinence 1 year after RC [33]. Further evaluations, such as urodynamics, could identify further therapeutic options for these patients (e.g., intensified urethral sphincter exercises and biofeedback training).
High perioperative PD in patients undergoing RC has previously been reported by Palapattu et al. [4]. Fear of disease progression has been identified as a major contributor to PD [34]. Worse emotional functioning in patients with an IC in our cohort may thus be explained by a more advanced tumor stage and a higher proportion of lymph node metastases. Psychosocial interventions by a multi-professional rehabilitation team, improving urinary continence, and increasing ability to autonomously care for the urostomy may contribute to significantly decreasing PD in our study. Multivariable logistic regression analysis identified age ≤ 59 years as the only independent predictor for high PD. Age ≤ 59 years and female sex were identified as independent predictors for the use of individual psychological counseling during IR. Female sex as a predictor for psychological counseling during IR is corroborated by studies from Herschbach et al. and Zabora et al. [35, 36]. According to Linden et al., anxiety is highly abundant in younger cancer patients, further supporting our findings [37]. PD should be monitored closely in all patients after RC, but especially so in younger patients at risk, as identified in this study. Referral to self-help groups and psycho-oncologic counseling should be considered if the need arises.
Neoadjuvant chemotherapy (NAC) can significantly prolong survival in patients with muscle-invasive bladder cancer (MIBC) [38, 39] and is recommended by international guidelines [40, 41]. Therefore, it is surprising that NAC was administered in only 9.9% of patients in this cohort. Studies investigating the underlying issues of a widespread administration of NAC in German MIBC-patients are urgently needed.
There are several limitations to our study. As patients from 135 primary hospitals were included in this study, surgical experience may have influenced the choice of urinary diversion and functional outcomes, as reported by Maurice et al. [42]. In our analysis, we did not differ between high-volume and low-volume centers. Furthermore, due to the study design, we could not assess HRQoL prior to RC. IR is specific to the German healthcare system and no control group outside of IR was included in this study. Based on many years of experience in treating patients after RC, it is assumed that almost all patients after RC undergo IR. However, data in this regard are lacking. But the need for close surveillance in the immediate period after RC (e.g., in an IR-setting) is stressed by a recent publication by our group, which showed a complication rate of > 96% in the early recovery period after RC [43].
Overall, this study reports a significant improvement in HRQoL, urinary continence, urostomy management, and PD in a recent cohort of patients in the early postoperative period after RC. Patient-reported outcome measures allow for an individual need assessment, may guide treatment decisions, and should be surveyed regularly during aftercare. Despite its limitations, this study provides important insight into challenges arising during the early postoperative period after RC.
Conclusion
HRQoL, urinary continence, and PD improved significantly during inpatient rehabilitation after RC and urinary diversion. At the end of IR, patients with social continence reported both better global HRQoL and less PD than patients without social continence. In addition, the percentage of patients able to manage their urostomy independently increased significantly during IR. Psychosocial support should be offered especially to younger patients.
Availability of data and materials
Data and materials are not publicly available, but are available by the corresponding author upon reasonable request.
Abbreviations
- RC:
-
Radical cystectomy
- IC:
-
Ileal conduit
- INB:
-
Ileal neobladder
- QoL:
-
Quality of life
- HRQoL:
-
Health-related quality of life
- PD:
-
Psychosocial distress
- IR:
-
Inpatient rehabilitation
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- NAC:
-
Neoadjuvant chemotherapy
- MIBC:
-
Muscle-invasive bladder cancer
References
Flegar L, Kraywinkel K, Zacharis A, Aksoy C, Koch R, Eisenmenger N et al (2022) Treatment trends for muscle-invasive bladder cancer in Germany from 2006 to 2019. World J Urol 40:1715–1721
Henningsohn L, Wijkstrom H, Pedersen J, Ahlstrand C, Aus G, Bergmark K et al (2003) Time after surgery, symptoms and well-being in survivors of urinary bladder cancer. BJU Int. 91:325–30
Klaassen Z, DiBianco JM, Jen RP, Harper B, Yaguchi G, Reinstatler L et al (2016) The impact of radical cystectomy and urinary diversion on suicidal death in patients with bladder cancer. J Wound Ostomy Continence Nurs 43:152–157
Palapattu GS, Haisfield-Wolfe ME, Walker JM, BrintzenhofeSzoc K, Trock B, Zabora J et al (2004) Assessment of perioperative psychological distress in patients undergoing radical cystectomy for bladder cancer. J Urol 172:1814–1817
Draeger DL, Sievert KD, Hakenberg OW (2018) Psychosocial distress in bladder cancer stratified by gender, age, treatment, and tumour stage. Urol Int 101:31–37
Grimm T, Grimm J, Buchner A, Schulz G, Jokisch F, Stief CG et al (2019) Health-related quality of life after radical cystectomy and ileal orthotopic neobladder: effect of detailed continence outcomes. World J Urol 37:2385–2392
Kretschmer A, Grimm T, Buchner A, Stief CG, Karl A (2016) Prognostic features for quality of life after radical cystectomy and orthotopic neobladder. Int Braz J Urol 42:1109–1120
Kretschmer A, Grimm T, Buchner A, Jokisch F, Ziegelmuller B, Casuscelli J et al (2020) Midterm health-related quality of life after radical cystectomy: a propensity score-matched analysis. Eur Urol Focus 6:704–710
Gerharz EW, Mansson A, Hunt S, Skinner EC, Mansson W (2005) Quality of life after cystectomy and urinary diversion: an evidence based analysis. J Urol 174:1729–1736
Ali AS, Hayes MC, Birch B, Dudderidge T, Somani BK (2015) Health related quality of life (HRQoL) after cystectomy: comparison between orthotopic neobladder and ileal conduit diversion. Eur J Surg Oncol 41:295–299
Hedgepeth RC, Gilbert SM, He C, Lee CT, Wood DP Jr (2010) Body image and bladder cancer specific quality of life in patients with ileal conduit and neobladder urinary diversions. Urology 76:671–675
Coates A, Porzsolt F, Osoba D (1997) Quality of life in oncology practice: prognostic value of EORTC QLQ-C30 scores in patients with advanced malignancy. Eur J Cancer 33:1025–1030
Roychowdhury DF, Hayden A, Liepa AM (2003) Health-related quality-of-life parameters as independent prognostic factors in advanced or metastatic bladder cancer. J Clin Oncol 21:673–678
Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft DK, AWMF). S3-Leitlinie Früherkennung, Diagnose, Therapie und Nachsorge des Harnblasenkarzinoms, Langversion 2.0, (2020) AWMF-Registrierungsnummer 032/038OL, https://www.leitlinienprogramm-onkologie.de/leitlinien/harnblasenkarzinom/. Accessed 16 Apr 2023
Erdogan B, Berg S, Noldus J, Muller G (2021) Early continence after ileal neobladder: objective data from inpatient rehabilitation. World J Urol 39:2531–2536
Kozaris R, Hanske J, von Landenberg N, Berg S, Roghmann F, Brock M et al (2021) Psychosocial distress in the early recovery period after radical prostatectomy. Urol Int. https://doi.org/10.1159/000519483
Hammerer P, Michl U, Meyer-Moldenhauer WH, Huland H (1996) Urethral closure pressure changes with age in men. J Urol 156:1741–1743
Waldmann A, Schubert D, Katalinic A (2013) Normative data of the EORTC QLQ-C30 for the German population: a population-based survey. PLoS ONE 8:e74149
El Bahnasawy MS, Osman Y, Gomha MA, Shaaban AA, Ashamallah A, Ghoneim MA (2000) Nocturnal enuresis in men with an orthotopic ileal reservoir: urodynamic evaluation. J Urol 164:10–13
El-Bahnasawy MS, Shaaban H, Gomha MA, Nabeeh A (2008) Clinical and urodynamic efficacy of oxybutynin and verapamil in the treatment of nocturnal enuresis after formation of orthotopic ileal neobladders. A prospective, randomized, crossover study. Scand J Urol Nephrol. 42:344–51
Hautmann RE, Egghart G, Frohneberg D, Miller K (1988) The ileal neobladder. J Urol 139:39–42
Osoba D, Rodrigues G, Myles J, Zee B, Pater J (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16:139–144
Clements MB, Atkinson TM, Dalbagni GM, Li Y, Vickers AJ, Herr HW et al (2022) Health-related quality of life for patients undergoing radical cystectomy: results of a large prospective cohort. Eur Urol 81:294–304
Singer S, Ziegler C, Schwalenberg T, Hinz A, Gotze H, Schulte T (2013) Quality of life in patients with muscle invasive and non-muscle invasive bladder cancer. Support Care Cancer 21:1383–1393
Abozaid M, Tan WS, Khetrapal P, Baker H, Duncan J, Sridhar A et al (2022) Recovery of health-related quality of life in patients undergoing robot-assisted radical cystectomy with intracorporeal diversion. BJU Int 129:72–79
Tyson MD 2nd, Barocas DA (2018) Quality of life after radical cystectomy. Urol Clin North Am 45:249–256
Kennedy F, Haslam C, Munir F, Pryce J (2007) Returning to work following cancer: a qualitative exploratory study into the experience of returning to work following cancer. Eur J Cancer Care (Engl) 16:17–25
Hoffman B (2005) Cancer survivors at work: a generation of progress. CA Cancer J Clin 55:271–280
Mastroianni R, Ferriero M, Tuderti G, Anceschi U, Bove AM, Brassetti A et al (2022) Open radical cystectomy versus robot-assisted radical cystectomy with intracorporeal urinary diversion: early outcomes of a single-center randomized controlled trial. J Urol 207:982–992
Clifford TG, Shah SH, Bazargani ST, Miranda G, Cai J, Wayne K et al (2016) Prospective evaluation of continence following radical cystectomy and orthotopic urinary diversion using a validated questionnaire. J Urol 196:1685–1691
Hautmann RE, Abol-Enein H, Davidsson T, Gudjonsson S, Hautmann SH, Holm HV et al (2013) ICUD-EAU International Consultation on Bladder Cancer 2012: Urinary diversion. Eur Urol 63:67–80
Gross T, Meierhans Ruf SD, Meissner C, Ochsner K, Studer UE (2015) Orthotopic ileal bladder substitution in women: factors influencing urinary incontinence and hypercontinence. Eur Urol 68:664–671
Bahlburg H, Schuster F, Tully KH, Butea-Bocu MC, Reike M, Roghmann F et al (2023) Prospective evaluation of functional outcomes in 395 patients with an ileal neobladder 1 year after radical cystectomy. World J Urol. https://doi.org/10.1007/s00345-023-04520-x
Dinkel A, Herschbach P (2018) Fear of progression in cancer patients and survivors. Recent Results Cancer Res 210:13–33
Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S (2001) The prevalence of psychological distress by cancer site. Psychooncology 10:19–28
Herschbach P, Britzelmeir I, Dinkel A, Giesler JM, Herkommer K, Nest A et al (2020) Distress in cancer patients: Who are the main groups at risk? Psychooncology 29:703–710
Linden W, Vodermaier A, Mackenzie R, Greig D (2012) Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord 141:343–351
Advanced Bladder Cancer Meta-analysis C (2005) Neoadjuvant chemotherapy in invasive bladder cancer: update of a systematic review and meta-analysis of individual patient data advanced bladder cancer (ABC) meta-analysis collaboration. Eur Urol. 48:202–5
Dalbagni G, Genega E, Hashibe M, Zhang ZF, Russo P, Herr H et al (2001) Cystectomy for bladder cancer: a contemporary series. J Urol 165:1111–1116
Witjes JA, Bruins HM, Cathomas R, Comperat EM, Cowan NC, Gakis G et al (2021) European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines. Eur Urol 79:82–104
Chang SS, Bochner BH, Chou R, Dreicer R, Kamat AM, Lerner SP et al (2017) Treatment of non-metastatic muscle-invasive bladder cancer: AUA/ASCO/ASTRO/SUO Guideline. J Urol 198:552–559
Maurice MJ, Kim SP, Abouassaly R (2017) Socioeconomic status is associated with urinary diversion utilization after radical cystectomy for bladder cancer. Int Urol Nephrol 49:77–82
Gotte M, Bahlburg H, Butea-Bocu MC, von Landenberg N, Tully K, Roghmann F et al (2022) Complications in the early recovery period after radical cystectomy-real data from impartial inpatient rehabilitation. Clin Genitourin Cancer 20:e424–e431
Acknowledgements
The authors would like to thank the patients for their participation in this study.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was funded by the “Nordrhein-Westfalen Association for the Fight Against Cancer, Germany.” The funder did not influence the study design, data collection, analysis, decision to publish, or preparation of the manuscript. Bahlburg, H: Funded by the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG) by grant BA 8185/1-1.
Author information
Authors and Affiliations
Contributions
HB and GM: drafted the manuscript. HB, MB, and GM: acquired the data. HB and GM: analyzed and interpreted data. GM: prepared the tables. JN and GM: designed the study and acquired the funding. KT, PB, MR, MB, FR, and JN: revised the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Ethical approval
The study protocol was approved by an institutional research committee (research authorization number FF30/2017).
Consent to publish
The authors confirm that consent to publish has been received from all the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bahlburg, H., Tully, K.H., Bach, P. et al. Improvements in urinary symptoms, health-related quality of life, and psychosocial distress in the early recovery period after radical cystectomy and urinary diversion in 842 German bladder cancer patients: data from uro-oncological rehabilitation. World J Urol 42, 111 (2024). https://doi.org/10.1007/s00345-024-04839-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-04839-z