Abstract
Purpose
Frailty is reportedly associated with poorer outcomes among surgical patients. Using a coding-based frailty tool, we investigated the impact of frailty on clinical outcomes and resource utilization for urolithiasis hospitalizations.
Methods
A cohort study using the 2018 National Inpatient Sample database. All adult elective hospitalizations for urolithiasis were included in the study. The study population was categorized into FRAIL and non-frail (nFRAIL) cohorts using the Johns Hopkins Adjusted Clinical Groups frailty clusters. The association between frailty and clinical and financial outcomes was evaluated using multivariate regression models.
Results
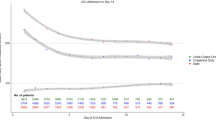
About 1028 (14.9%) out of 6900 total hospitalizations were frail. Frailty was not associated with a significant increase in the odds of in-hospital mortality (adjusted odds ratio (aOR) 1.73, 95% CI 0.15–20.02) or length of hospital stay, but was associated with a lower chance of surgery within 24 h of admission (aOR 0.65, 95% CI 0.48–0.90, P = 0.008). A higher Charlson index was independently associated with an over 100% increase in the odds of in-hospital mortality (aOR 2.091, 95% CI 1.53–2.86, P < 0.001). Frail patients paid $15,993 higher in total hospital costs and had a higher likelihood of non-home discharges (aOR 4.29, 95% CI 2.74–6.71, P < 0.001) and peri-operative complications (aOR 1.77, 95% CI 1.14–2.73, P = 0.01).
Conclusion
Frailty was correlated with unfavorable outcomes, except mortality and prolonged hospital stay. Incorporating frailty evaluation into risk models has the potential to enhance patient selection and preparation for urolithiasis intervention.

Similar content being viewed by others
Data availability
In compliance with the copyright restrictions set by the AHRQ pertaining to the distribution of HCUP databases, the database utilized in this research will not be made publicly available by the authors. However, all NIS datasets are publicly available through the authorized HCUP central distributor upon request at https://hcup-us.ahrq.gov/tech_assist/centdist.jsp.
References
Johnson CM, Wilson DM, O’Fallon WM, Malek RS, Kurland LT (1979) Renal stone epidemiology: a 25-year study in Rochester, Minnesota. Kidney Int 16(5):624–631. https://doi.org/10.1038/ki.1979.173
Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC (2003) Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int 63(5):1817–1823. https://doi.org/10.1046/j.1523-1755.2003.00917.x
Whitehurst L, Jones P, Somani BK (2019) Mortality from kidney stone disease (KSD) as reported in the literature over the last two decades: a systematic review. World J Urol 37(5):759–776. https://doi.org/10.1007/s00345-018-2424-2
Miller NL, Lingeman JE (2007) Management of kidney stones. BMJ 334(7591):468–472. https://doi.org/10.1136/bmj.39113.480185.80
Vermillion SA, Hsu FC, Dorrell RD, Shen P, Clark CJ (2017) Modified frailty index predicts postoperative outcomes in older gastrointestinal cancer patients. J Surg Oncol 115(8):997–1003. https://doi.org/10.1002/jso.24617
Chao CT, Wang J, Huang JW, Hung KY, Chien KL (2020) Frailty predicts a higher risk of incident urolithiasis in 525,368 patients with diabetes mellitus: a population-based study. BMJ Open Diabetes Res Care 8(1):e000755. https://doi.org/10.1136/bmjdrc-2019-000755
Healthcare Cost and Utilization Project (2008) NIS database documentation. https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2018.jsp. Accessed 26 Jan 2023
Kaiser Family Foundation Medicare Advantage (2022) Medicare advantage in 2022: Enrolment update and key trends. www.kff.org/medicare/fact-sheet/medicare-advantage/ exit disclaimer. Accessed 26 Jan 2023
Healthcare Cost & Utilization Project (2022) Methods series. https://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. Accessed 26 Jan 2023
Park MG, Haro G, Mabeza RM et al (2022) Association of frailty with clinical and financial outcomes of esophagectomy hospitalizations in the United States. Surg Open Sci 9:80–85. https://doi.org/10.1016/j.sopen.2022.05.003
The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System (2022) Frailty assessment calculator. https://www.johnshopkinssolutions.com/solution/frailty. Accessed 26 Jan 2022
Pylväläinen J, Talala K, Murtola T et al (2019) Charlson comorbidity index based on hospital episode statistics performs adequately in predicting mortality, but its discriminative ability diminishes over time. Clin Epidemiol 11:923–932. https://doi.org/10.2147/CLEP.S218697
Daniel N, Minot N (1996) An introduction to statistics and data analysis using Stata®. SAGE Publications Inc. https://www.pdfdrive.com/an-introduction-to-statistics-and-data-analysis-using-stata-from-research-design-to-final-report-e191513302.html. Accessed 26 Jan 2023
Dobaria V, Hadaya J, Sanaiha Y, Aguayo E, Sareh S, Benharash P (2021) The pragmatic impact of frailty on outcomes of coronary artery bypass grafting. Ann Thorac Surg 112(1):108–115. https://doi.org/10.1016/j.athoracsur.2020.08.028
Hadaya J, Sanaiha Y, Juillard C, Benharash P (2021) Impact of frailty on clinical outcomes and resource use following emergency general surgery in the United States. PLoS ONE 16(7):e0255122. https://doi.org/10.1371/journal.pone.0255122
Roche JJ, Wenn RT, Sahota O, Moran CG (2005) Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 331(7529):1374. https://doi.org/10.1136/bmj.38643.663843.55
Nielsen PR, Andreasen J, Asmussen M, Tønnesen H (2008) Costs and quality of life for prehabilitation and early rehabilitation after surgery of the lumbar spine. BMC Health Serv Res 8:209. https://doi.org/10.1186/1472-6963-8-209
Rombey T, Eckhardt H, Quentin W (2019) Cost-effectiveness of prehabilitation prior to elective surgery compared to usual preoperative care: protocol for a systematic review of economic evaluations. BMJ Open 10:e040262. https://doi.org/10.1136/bmjopen-2020-04026
Durrand J, Singh SJ, Danjoux G (2019) Prehabilitation. Clin Med (Lond) 19(6):458–464. https://doi.org/10.7861/clinmed.2019-0257
Karunungan KL, Hadaya J, Tran Z et al (2021) Frailty is independently associated with worse outcomes after elective anatomic lung resection. Ann Thorac Surg 112(5):1639–1646. https://doi.org/10.1016/j.athoracsur.2020.11.004
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by FU, VO, FM, and OA. FU, VO, NC and CI performed project development. The first draft of the manuscript was written by NC, CI, LE, OO, MB, and BA, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no relevant financial or non-financial interests to disclose.
Ethical approval for retrospective studies
This study complies with the ethical standards set by the US government through the Agency for Healthcare Research and Quality (AHRQ) which manages and regulates the use of the NIS.
Informed consent
This was a retrospective study based on the Nationwide Inpatient Sample (NIS). The NIS is devoid of both patient and hospital-level identifiers which makes obtaining informed consent impossible. Nonetheless, this study conforms to the standards prescribed by the Agency for Healthcare Research and Quality which manages and regulates the use of the NIS.
Research involving human participants, their data, or biological materials
This research did not involve any human subjects, and no biological material was collected at any stage of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Uwumiro, F., Okpujie, V., Madu, F. et al. Impact of frailty on clinical outcomes and resource utilization of hospitalizations for renal stone surgery. World J Urol 41, 2519–2526 (2023). https://doi.org/10.1007/s00345-023-04511-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04511-y