Abstract
Purpose
Although active surveillance (AS) is recommended for low- to favorable intermediate-risk prostate cancer (PCa), risk of upgrading at radical prostatectomy (RP) is not negligible. Available studies based on systematic transrectal ultrasound biopsy might not be applicable to contemporary cohorts diagnosed with MRI-targeted biopsy (TB). The aim of the present study is to explore rates and risk factors for adverse outcomes (AO) at RP in patients with ISUP ≤ 2 PCa detected at TB with concomitant systematic biopsy (SB).
Methods
Multicenter, retrospective analysis of 475 consecutive patients with ISUP ≤ 2 PCa at MRI-TB + SB is treated with RP. AO were defined as ISUP upgrading, adverse pathology (upgrading to ISUP ≥ 3 and/or ≥ pT3 at RP, and/or pN1) (AP) or biochemical recurrence (BCR) in men with follow-up (n = 327).
Results
The rate of ISUP upgrading, upgrading ≥ 3, and AP were 39%, 21%, and 43%. Compared to ISUP2, men with ISUP1 PCa had a higher rate of overall upgrading (27 vs. 67%, p < 0.001), but less upgrading to ≥ 3 (27 vs. 10%, p < 0.001). AP was more common when ISUP2 was detected with a combined MRI-TB + SB approach compared to considering TB (p = 0.02) or SB (p = 0.01) alone. PSA, PSA density, PI-RADS, ISUP at TB, overall biopsy ISUP and EAU classification were predictors of upgrading to ISUP ≥ 3 and AP. The 1 year BCR-free survival was 94% with no differences in BCR rates between subgroups.
Conclusion
Upgrading in ISUP ≤ 2 PCa remains prevalent even in men diagnosed in the MRI era. The use of MRI-TB with concomitant SB allows for the accurate identification of ISUP2 PCa and predicts the risk of AO at RP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the introduction of PSA [1], overdiagnosis and overtreatment represent main issues in prostate cancer (PCa) management. Multiparametric magnetic resonance imaging (mpMRI) has been introduced in the clinical practice [2,3,4] and can be used as a triage test to identify men with clinical suspicion of PCa who should receive a prostate biopsy. The routine use of mpMRI in the diagnostic pathway of PCa might allow for the identification of aggressive disease requiring radical therapy and theoretically miss indolent cancers who could ideally be considered for active surveillance (AS). Surveillance has been widely accepted as recommended treatment for low-risk PCa [5] with equivalent oncological outcomes compared to definitive therapy at medium-term follow-up [6, 7]. Moreover, more than half of the established AS protocols allow for the inclusion of patients with intermediate-risk features [8]. Nonetheless, the risk of unfavorable pathology at radical prostatectomy (RP) is substantials up to 78% AS candidates managed with RP harbored adverse disease features at final pathology [9]. However, these observations derive from cohorts diagnosed with random transrectal ultrasound (TRUS) biopsy. Due to the higher accuracy for the identification of clinically significant PCa by MRI-guided biopsy [2,3,4], the generalizability of these findings in the mpMRI era is not warranted.
We hypothesized that mpMRI and MRI-targeted biopsy would allow for the reliable identification of AS candidates thus resulting in a lower risk of upgrading and adverse pathology (AP) in low- and favorable intermediate-risk patients undergoing RP. We aimed at reporting the rate and at identifying predictors of upgrading and early biochemical recurrence (BCR) in men with mpMRI/TRUS-fusion biopsy diagnosed ISUP 1 and 2 PCa and managed with RP.
Patients and methods
Study population
Retrospective databases from seven European tertiary referral centers were taken. Board approval was obtained according to each institution’s policy. We identified 475 patients that underwent RP for ISUP ≤ 2 PCa on mpMRI/TRUS-fusion biopsy between the years 2016 and 2021. mpMRIs were performed according to each institutions protocol and scored by expert genitourinary radiologists using PI-RADS v2 [10]. MRI-targeted fusion biopsy (TB) with concomitant systematic (SB) was performed by experienced urologists using their preferred biopsy technique including cognitive or software supported biopsy. All patients were treated with robot-assisted or open RP. Histopathology was reviewed in each center according to clinical routine by expert dedicated urogenital pathologist. Follow-up data were available for 327 patients. Data were reported according to the Standards of Reporting for MRI-Targeted Biopsy Studies (START) [11].
Outcome measurements and predictors
Adverse outcomes (AO) were defined as ISUP upgrading or adverse pathology (AP = upgrading to ISUP ≥ 3 and/or ≥ pT3 at RP, and/or N1). BCR was defined as two consecutive PSA values ≥ 0.2 ng/mL. Patients were stratified according to EAU low-risk and favorable intermediate-risk (ISUP 2, PSA < 10 ng/ml and ≤ T2).
Age, digital rectal examination (DRE), prostate volume, PSA, PSA-Density, PI-RADS, targeted lesion volume, extracapsular extension (ECE) on mpMRI, number of TB cores, percentage of positive TB cores, ISUP at TB, number of SB cores, percentage of positive SB cores, ISUP at SB, number of overall cores, percentage of positive cores, overall ISUP and EAU classification group were analyzed as variables predicting AO and all of the above plus ISUP at RP, ISUP upgrading, upgrading to ISUP ≥ 3, a ≥ pT3, any AO and positive surgical margins were analyzed as variables predicting BCR.
Statistical analysis
Differences between groups were assessed by using chi-square test for categorial and T test for continuous variables. Logistic and COX regression analyses determined predictive factors. Due to the relatively small number of events, univariable analyses were used to assess predictors of outcomes. Results were considered statistically significant for p < 0.05. Analyses were conducted using SPSS version 27 (IBM, Armonk, NY, USA).
Results
Baseline patient characteristics
Baseline patient demographics and clinical characteristics for all patients and stratified to subgroups are shown in Table 1.
Incidence of adverse outcomes characterized by biopsy approach
Analyzing the combined SB and TB approach, 185 (39%) and 101 (21%) patients experienced any ISUP upgrading and upgrading to ISUP ≥ 3, respectively. Biopsy ISUP 1 was upgraded in 98 (67%) patients, but only in 14 (10%) to ISUP ≥ 3. Biopsy ISUP 2 was upgraded in 87 (27%) patients and downgraded in 9 (3%) patients (Supplementary Table 1A). The combined biopsy approach correctly identified 84% of ISUP 1 PCa at RP, which would not have been different using a SB only approach identifying 81% of ISUP 1 PCa (p = 0.6). A TB only approach on the other hand would have correctly predicted significantly less ISUP 1 PCa (p < 0.001). Eighteen men without cancer at TB harbored ISUP ≥ 3 cancers. Compared to ISUP at RP, the combined approach correctly characterized 73% of ISUP 2 PCa, which is significantly more (p < 0.001) than either SB with 52% or TB with 58% alone would have detected (SB vs. TB: p = 0.1, Supplementary Table 1). Similar detection rates were found for favorable intermediate-risk only Fig. 1A, where the combined biopsy approach detected significantly more ISUP 2 PCa than TB or SB alone (p = 0.001 and p < 0.001, respectively).
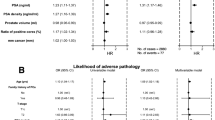
Radical prostatectomy outcomes of patients with favorable intermediate-risk disease. A Upgrading and downgrading stratified by biopsy approach; B Upgrading and downgrading based on ISUP 2 detecting biopsy approach (ISUP 2 at TB&SB n = 131, ISUP 2 at TB only n = 72, ISUP 2 at SB only n = 53), C Adverse pathology findings based on ISUP 2 detecting biopsy approach (ISUP 2 at TB&SB n = 131, ISUP 2 at TB only n = 72, ISUP 2 at SB only n = 53), TB targeted biopsies, SB systematic biopsies, ISUP International Society of Urological Pathology, AP adverse pathology, RP radical prostatectomy
Compared to the RP specimen, the least upgrading was found when ISUP 2 was present in TB only. Patients with ISUP 2 at TB only had a significantly lower upgrading rate (15%) compared to ISUP 2 at TB and SB (31%) (p = 0.01). No significant differences were found comparing upgrading rates of ISUP 2 at SB only (19%) to ISUP 2 at TB and SB (p = 0.1) or ISUP 2 at TB only (p = 0.555) Fig. 1B. Similarly, men with favorable intermediate-risk disease demonstrated significantly more AP on RP when ISUP 2 features were present in both TB and SB compared to the presence of ISUP 2 features in TB (p = 0.021) or SB (p = 0.005) only Fig. 1C. In men diagnosed with low-risk Pca, there was significantly less upgrading and less AP if ISUP 1 was only present in SB and not in both SB and TB (p = 0.008 and p 0.024) Supplementary Fig. 1.
Incidence of adverse outcomes and biochemical recurrence stratified by subgroups
RP outcomes and incidences of AO and BCR are shown in Table 1. Between the low-risk and the favorable intermediate-risk group, there were significant differences regarding ISUP at RP, RP pT, ISUP upgrading and AP. With 65% overall, including upgrading to ISUP 2, upgrading rates were considerably higher in the low-risk group compared to the favorable intermediate-risk group with 24%. For the 327 patients with available follow-up, the 1 year BCR-free survival was 94%. Neither time of follow-up nor BCR rate did significantly differ between the subgroups.
Predictors of adverse outcomes and biochemical recurrence
Predictors of AO and BCR are shown in Table 2. Higher PSA, higher PSA density, PI-RADS, ISUP at TB, overall biopsy ISUP and EAU classification were all predictors for upgrading to ISUP ≥ 3 and AP. Additionally, number of SB and overall biopsies and ISUP at SB were predictive for upgrading to ISUP ≥ 3. For pT3, percentage of positive overall biopsies, SBs and TBs were positive predictors and number of overall biopsies and SBs were negative predictors, too. For AP, ISUP at SB and percentage of positive overall and TBs were predictive in addition to the variables described above. None of the primary mpMRI/TRUS-fusion biopsy variables, but all AOs including any ISUP upgrading, upgrading to ISUP ≥ 3, adverse pT (≥ pT3) at RP and AP as well as ISUP at RP were predictors for BCR. Predictors of AO for the subgroups are shown in Supplementary Table 2.
Discussion
In this multicenter cohort 39% of men with MRI/TRUS-fusion diagnosed ISUP ≤ 2 PCa were upgraded on RP and 21% harbored disease of ISUP ≥ 3. Higher PSA, higher PSA density, PI-RADS, ISUP at TB, overall biopsy ISUP and EAU classification were all predictors for upgrading to ISUP ≥ 3, pT ≥ 3 and AP. The 1 year BCR-free survival was 94% and did not differ between low-risk and favorable intermediate-risk. Any ISUP upgrading, upgrading to ISUP ≥ 3, pT ≥ 3 at RP and AP as well as ISUP at RP were predictors for BCR.
Despite the modern MRI/TRUS-fusion technique used for diagnosis, more than 1 in 5 patients were upgraded to ISUP ≥ 3 and 4 out of 10 patients demonstrated AP on RP. Although we initially hypothesized that the introduction of MRI and TB may result in a better preoperative characterization, these findings highlight that the risk of harboring an ISUP 3 disease with poorer prognosis is still relevant in contemporary patients who could have been considered for AS [12]. Of note, our study represents the first assessment of AP and BCR in a large cohort diagnosed with MRI-targeted biopsy and undergoing RP. As such, comparing our results to cohorts not relying on MRI/TRUS-fusion is complex due to heterogenous populations. Moreover, our data are too immature to draw any final conclusions regarding the correlation of AP and long-term outcomes like metastatic progression and survival.
In a large population-based cohort of patients treated in the 2010s, upgrading was seen in 43–61% of biopsy GS 6 [13]. Schiffmann et al. evaluated more than 1000 patients with very low-risk and low-risk disease and found upgrading rates of 55% and 78%, respectively [9]. Other studies focused on patients with favorable intermediate-risk PCa. In a series of over 10,000 patients, Yang et al. found a 33% incidence of upgrading or upstaging [14]. One study including intermediate-risk disease has found AP outcomes in 36% of patients [15]. However, in men with biopsy GS 3 + 4 and cT1–2 stage, Ploussard et al. reported that the rate of GS upgrading was 25% [16]. In another cohort including low- and intermediate-risk patients, Gandaglia et al. reported 33% of patients with unfavorable disease defined as non-organ confined or ISUP ≥ 3 disease at RP [17].
Our data support recent evidence suggesting that compared to an SB approach upfront MRI, an TB detect equal or even more intermediate-risk PCa, while decreasing the detection rate of low-risk PCa [3, 18,19,20]. However, we also show that compared to the combined approach, a TB only approach would have characterized significantly less ISUP ≥ 2 PCa correctly. This adds to the debate on whether TB alone is sufficient to diagnose higher grade PCa accurately or whether additional SB is still necessary. In the favorable intermediate-risk subgroup, ISUP 2 disease diagnosed at TB only was most concordant to RP and had a significantly lower risk of upgrading compared to ISUP 2 detected both at TB and SB. Men with IUSP 2 features on both SB and TB had a higher likelihood of experiencing AP compared to ISUP 2 features in either TB or SB alone. To the best of our knowledge, this is the first time demonstrating that upgrading and AP in favorable intermediate-risk disease depends on the biopsy approach detecting ISUP 2 features. Based on this, considering patients with favorable intermediate-risk PCa for AS seems more justifiable when the diagnosis was made by a combined biopsy approach and ISUP 2 features are limited to a small amount of positive cores in TB or SB only. Further strategies to improve TB performance are currently evaluated and have already been shown to increase the accuracy of higher grade PCa detection. These include extending the number of TB and target saturation biopsies including the perilesional penumbra [19, 21,22,23].
Previous studies identified multiple factors for upgrading and AO at RP, including but not limited to age, PSA, cT, number and percentage of positive cores, tumor involvement per core, and perineural invasion [9, 13,14,15,16,17, 24]. Although we describe similar predictors, some findings should be further discussed. PI-RADS was identified as a predictor for upgrading to ISUP ≥ 3 and AP as previously reported in a single-institution study by Pham et al. [25]. Moreover, ECE on mpMRI predicted AP in the subgroup with low-risk PCa and lesion volume predicted upgrading to ISUP ≥ 3 in the subgroup with favorable intermediate-risk PCa. This emphasizes the role mpMRI findings should play when counseling our patients. Indeed, patients eligible for AS were more likely to experience upgrading at RP when suspect lesions were identified on mpMRI compared to unsuspicious mpMRIs [26,27,28]. The fact that a rising number of SB and overall biopsies is predictive for upgrading to ISUP ≥ 3 seems counterintuitive. This could be explained with a sampling error oversampling Gleason 3 pattern and non-cancerous tissue with extensive systematic biopsies. To fully address this question, histopathology result and sampling location of each individual core would need to be analyzed. At present, our data confirm the updated EAU guidelines position, that saturation biopsy is not being significantly more conclusive than 10–12 cores.
Despite being the first study assessing rate and predictors of AP and BCR in the MRI-targeted biopsy era, our study is not devoid of limitations. There is a selection bias, as information on which factors influenced physicians’ and patients’ decision toward RP is missing. There was no central radiology or pathology review and variations in the interpretation of findings might have influenced the results. No distinction was made between transrectal and perineal as well as cognitive and software-based fusion biopsy. Some information on known predictors of unfavorable outcomes like PCa core percentage or perineural invasion were not available for all institutions and therefore not incorporated into the analysis. Last, the study is subject to the usual limitations of retrospective studies.
Conclusions
Pathological upgrading in patients diagnosed with ISUP ≤ 2 PCa remains prevalent in the era of MRI/TRUS-fusion biopsy. Although a TB only approach reduces the diagnosis of low-risk PCa, a combined SB and TB approach more accurately characterizes ISUP 2 and risk of AP at RP. Thus, AS for patients with favorable intermediate-risk PCa seems more justifiable when the diagnosis was made by a combined biopsy approach and ISUP 2 features are limited to a small amount of positive cores in TB or SB, only.
Data availability statement
The data that support the findings of this study are available from the corresponding author, Claudia Kesch, upon reasonable request.
References
Stamey TA, Yang N, Hay AR, McNeal JE, Freiha FS, Redwine E (1987) Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N Engl J Med 317:909–916. https://doi.org/10.1056/NEJM198710083171501
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389:815–822. https://doi.org/10.1016/S0140-6736(16)32401-1
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 378:1767–1777. https://doi.org/10.1056/NEJMoa1801993
Eklund M, Jäderling F, Discacciati A, Bergman M, Annerstedt M, Aly M et al (2021) MRI-targeted or standard biopsy in prostate cancer screening. N Engl J Med 385:908–920. https://doi.org/10.1056/NEJMoa2100852
Tosoian JJ, Mamawala M, Epstein JI, Landis P, Wolf S, Trock BJ et al (2015) Intermediate and longer-term outcomes from a prospective active-surveillance program for favorable-risk prostate cancer. J Clin Oncol 33:3379–3385. https://doi.org/10.1200/JCO.2015.62.5764
Klotz L (2012) Active surveillance: the Canadian experience. Curr Opin Urol 22:222–230. https://doi.org/10.1097/MOU.0b013e328352598c
Bul M, Zhu X, Valdagni R, Pickles T, Kakehi Y, Rannikko A et al (2013) Active surveillance for low-risk prostate cancer worldwide: the PRIAS study. Eur Urol 63:597–603. https://doi.org/10.1016/j.eururo.2012.11.005
Willemse P-PM, Davis NF, Grivas N, Zattoni F, Lardas M, Briers E et al (2021) Systematic review of active surveillance for clinically localised prostate cancer to develop recommendations regarding inclusion of intermediate-risk disease, biopsy characteristics at inclusion and monitoring, and surveillance repeat biopsy strategy. Eur Urol. https://doi.org/10.1016/j.eururo.2021.12.007
Schiffmann J, Wenzel P, Salomon G, Budäus L, Schlomm T, Minner S et al (2015) Heterogeneity in D’Amico classification-based low-risk prostate cancer: differences in upgrading and upstaging according to active surveillance eligibility. Urol Oncol 33(329):e13-19. https://doi.org/10.1016/j.urolonc.2015.04.004
Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ et al (2016) PI-RADS prostate imaging—reporting and data system: 2015, version 2. Eur Urol 69:16–40. https://doi.org/10.1016/j.eururo.2015.08.052
Moore CM, Kasivisvanathan V, Eggener S, Emberton M, Fütterer JJ, Gill IS et al (2013) Standards of reporting for MRI-targeted biopsy studies (START) of the prostate: recommendations from an International Working Group. Eur Urol 64:544–552. https://doi.org/10.1016/j.eururo.2013.03.030
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA et al (2016) The 2014 International society of urological pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 40:244–252. https://doi.org/10.1097/PAS.0000000000000530
Caster JM, Falchook AD, Hendrix LH, Chen RC (2015) Risk of pathologic upgrading or locally advanced disease in early prostate cancer patients based on biopsy Gleason score and PSA: a population-based study of modern patients. Int J Radiat Oncol Biol Phys 92:244–251. https://doi.org/10.1016/j.ijrobp.2015.01.051
Yang DD, Mahal BA, Muralidhar V, Nezolosky MD, Vastola ME, Labe SA et al (2019) Risk of upgrading and upstaging among 10 000 patients with Gleason 3 + 4 favorable intermediate-risk prostate cancer. Eur Urol Focus 5:69–76. https://doi.org/10.1016/j.euf.2017.05.011
Wong L-M, Tang V, Peters J, Costello A, Corcoran N (2016) Feasibility for active surveillance in biopsy Gleason 3 + 4 prostate cancer: an Australian radical prostatectomy cohort. BJU Int 117(4):82–87. https://doi.org/10.1111/bju.13460
Ploussard G, Isbarn H, Briganti A, Sooriakumaran P, Surcel CI, Salomon L et al (2015) Can we expand active surveillance criteria to include biopsy Gleason 3+4 prostate cancer? A multi-institutional study of 2323 patients. Urol Oncol 33(71):e1-9. https://doi.org/10.1016/j.urolonc.2014.07.007
Gandaglia G, van den Bergh RCN, Tilki D, Fossati N, Ost P, Surcel CI et al (2018) How can we expand active surveillance criteria in patients with low- and intermediate-risk prostate cancer without increasing the risk of misclassification? Development of a novel risk calculator. BJU Int 122:823–830. https://doi.org/10.1111/bju.14391
Rouvière O, Puech P, Renard-Penna R, Claudon M, Roy C, Mège-Lechevallier F et al (2019) Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): a prospective, multicentre, paired diagnostic study. Lancet Oncol 20:100–109. https://doi.org/10.1016/S1470-2045(18)30569-2
van der Leest M, Cornel E, Israël B, Hendriks R, Padhani AR, Hoogenboom M et al (2019) Head-to-head comparison of transrectal ultrasound-guided prostate biopsy versus multiparametric prostate resonance imaging with subsequent magnetic resonance-guided biopsy in biopsy-naïve men with elevated prostate-specific antigen: a large prospective multicenter clinical study. Eur Urol 75:570–578. https://doi.org/10.1016/j.eururo.2018.11.023
Drost F-JH, Osses DF, Nieboer D, Steyerberg EW, Bangma CH, Roobol MJ et al (2019) Prostate MRI, with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database Systematic Rev. https://doi.org/10.1002/14651858.CD012663.pub2
Calio BP, Sidana A, Sugano D, Gaur S, Maruf M, Jain AL et al (2018) Risk of upgrading from prostate biopsy to radical prostatectomy pathology-does saturation biopsy of index lesion during multiparametric magnetic resonance imaging-transrectal ultrasound fusion biopsy help? J Urol 199:976–982. https://doi.org/10.1016/j.juro.2017.10.048
Tschirdewahn S, Wiesenfarth M, Bonekamp D, Püllen L, Reis H, Panic A et al (2021) Detection of significant prostate cancer using target saturation in transperineal magnetic resonance imaging/transrectal ultrasonography-fusion biopsy. Eur Urol Focus 7:1300–1307. https://doi.org/10.1016/j.euf.2020.06.020
Brisbane WG, Priester AM, Ballon J, Kwan L, Delfin MK, Felker ER et al (2022) Targeted prostate biopsy: umbra, penumbra, and value of perilesional sampling. Eur Urol S0302–2838(22):00010. https://doi.org/10.1016/j.eururo.2022.01.008
Morlacco A, Cheville JC, Rangel LJ, Gearman DJ, Karnes RJ (2017) Adverse disease features in Gleason Score 3 + 4 “favorable intermediate-risk” prostate cancer: implications for active surveillance. Eur Urol 72:442–447. https://doi.org/10.1016/j.eururo.2016.08.043
Pham DM, Kim JK, Lee S, Hong SK, Byun S-S, Lee SE (2020) Prediction of pathologic upgrading in Gleason score 3+4 prostate cancer: who is a candidate for active surveillance? Investig Clin Urol 61:405–410. https://doi.org/10.4111/icu.2020.61.4.405
Schoots IG, Nieboer D, Giganti F, Moore CM, Bangma CH, Roobol MJ (2018) Is magnetic resonance imaging-targeted biopsy a useful addition to systematic confirmatory biopsy in men on active surveillance for low-risk prostate cancer? A systematic review and meta-analysis. BJU Int 122:946–958. https://doi.org/10.1111/bju.14358
Hamoen EHJ, Hoeks CMA, Somford DM, van Oort IM, Vergunst H, Oddens JR et al (2019) Value of serial multiparametric magnetic resonance imaging and magnetic resonance imaging-guided biopsies in men with low-risk prostate cancer on active surveillance after 1 yr follow-up. Eur Urol Focus 5:407–415. https://doi.org/10.1016/j.euf.2017.12.008
Fujihara A, Iwata T, Shakir A, Tafuri A, Cacciamani GE, Gill K et al (2021) Multiparametric magnetic resonance imaging facilitates reclassification during active surveillance for prostate cancer. BJU Int 127:712–721. https://doi.org/10.1111/bju.15272
Funding
Open Access funding enabled and organized by Projekt DEAL. None.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception, design and data collection. Analysis was performed by CK. The first draft of the manuscript was written by CK, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Claudia Kesch has received consulting fees from Apogepha; has received research funding from Advanced Accelerator Applications (Novartis), and curie therapeutics; and has received compensation for travel from Janssen Pharmaceuticals; Jan Philipp Radtke has received consulting fees from Saegeling Medizintechnik, Advanced Accelerator Applications (Novartis), Beckelmann, Astellas, Bayer, Janssen Pharmaceuticals, MedCom, Philips Invivo, Bender Gruppe, Apogepha, SPL Medical; and has received research funding from Advanced Accelerator Applications (Novartis), and Deutsche Krebshilfe; Boris Hadaschik has had advisory roles for ABX, Astellas, AstraZeneca, Bayer, Bristol Myers Squibb, Janssen R&D, Lightpoint Medical, Inc., and Pfizer; has received research funding from Astellas, Bristol Myers Squibb, German Research Foundation, Janssen R&D, Novartis and Pfizer; and has received compensation for travel from Astellas, AstraZeneca, and Janssen R&D. The other authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
345_2022_4236_MOESM1_ESM.pptx
Supplementary file1 Radical prostatectomy outcomes of patients with low-risk disease. B Upgrading and downgrading based on ISUP 1 detecting biopsy approach (ISUP 1 at TB&SB n = 56, ISUP 1 at TB only n = 13, ISUP 1 at SB only n = 43) C Adverse pathology findings based on ISUP 2 detecting biopsy approach (ISUP 1 at TB&SB n = 56, ISUP 1 at TB only n = 13, ISUP 1 at SB only n = 43), TB targeted biopsies, SB systematic biopsies, ISUP International Society of Urological Pathology, AP adverse pathology, RP radical prostatectomy (PPTX 877 KB)
345_2022_4236_MOESM3_ESM.docx
Supplementary file3 Predictors for upgrading to ISUP ≥ 3 and adverse pathology stratified by subgroups (univariate logistic regression) (DOCX 17 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kesch, C., Pantea, V., Soeterik, T. et al. Risk and predictors of adverse pathology after radical prostatectomy in patients diagnosed with IUSP 1–2 prostate cancer at MRI-targeted biopsy: a multicenter analysis. World J Urol 41, 427–434 (2023). https://doi.org/10.1007/s00345-022-04236-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-04236-4