Abstract
Purpose
Bladder perforation (BP) is the most important intraoperative adverse event of transurethral resection of bladder tumor (TURBT). It is frequently underreported despite its impact on the postoperative course. There is no standardized classification of BP. The study aims to develop a classification of the depth of endoscopic bladder perforation during TURBT.
Methods
This is a sub-analysis of a prospective randomized trial enrolling 248 patients submitted to en-bloc vs conventional TURBT from 03/2018 to 06/2021. The DEpth of Endoscopic Perforation (DEEP) scale is as follows: “0” visible muscular layer with no perivesical fat; “1” visible muscle fibers with spotted perivesical fat; “2” exposition of perivesical fat; “3” intraperitoneal perforation. Logistic and linear regression models were used to investigate predictors of high-grade perforations (DEEP 2–3) and to assess whether the DEEP scale independently predicted patients' postoperative outcomes.
Results
A total of 146/248 (58.9%), 56/248 (22.6%), 41/248 (16.5%), 5/248 (2.0%) patients presented DEEP grade 0, 1, 2, and 3, respectively. Female gender [B coeff. 0.255 (95% CI 0.001–0.513); p = 0.05], tumor location [B coeff. 0.188 (0.026–0.339); p = 0.015], and obturator-nerve reflex [B coeff. 0.503 (0.148–0.857); p = 0.006] were independent predictors of DEEP. The scale predicted independently major complications [Odd Ratio (OR) 2.221 (1.098–4.495); p = 0.026], no post-operative chemotherapy intravesical instillation [OR 9.387 (2.434–36.200); p = 0.001], longer irrigation time [B coeff. 0.299 (0.166–0.441); p < 0.001] and hospital stay [B coeff. 0.315 (0.111–0.519); p = 0.003].
Conclusion
The DEEP scale provides a visual tool for grading bladder perforation during TURBT, which can help physicians standardize complication reporting and plan postoperative management accordingly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transurethral resection of bladder tumor (TURBT) is employed for the diagnosis of bladder cancer (BC). In non-muscle invasive BC (NMIBC), TURBT and adjuvant intravesical instillation are considered the gold standard treatment [1, 2]. Despite TURBT is a very common surgery in urology, it is not devoid of complications. Bleeding and bladder perforation (BP) are typical complications [3]. Moreover, the absence of BP is considered a quality indicator of TURBT, on par with the presence of detrusor muscle in the specimen [4]. Although BP is considered uncommon, reaching a 2.5–5% risk during procedure [5], several studies showed a non-negligible underdiagnosis and underreporting rates leading to a real frequency ranging up to 58.3% [6]. The absence of standardized methods to report intraoperative adverse events has been recognized as a major issue by the European Association of Urology, which created an ad hoc Complication Guideline Panel to propose a dedicated classification [7]. This may help identifying proper measures of benchmarking, to compare surgeons, institutions and surgical techniques, to characterize surgical morbidity and report it accurately to patients [7]. Moreover, a universal standard reporting system of intraoperative adverse events is being developed through a Delphi Consensus (ICARUS project) [8]. In TURBT, the resection depth is the most conditioning factor, either intraoperatively or postoperatively. Depending on resection depth, the surgeon may decide to interrupt the procedure and/or to avoid immediate intravesical instillation of chemotherapy to limit drug extravasation [6].
Thus, a standardized classification of resection depth is necessary to identify the preoperative risk factors and analyze the post-operative consequences. The aim of this study is to provide a novel classification describing the depth of resection to provide a standard and reproducible tool to the urological community.
Materials and methods
Study population
The study was designed within a single-center randomized, controlled, non-inferiority trial comparing patients subjected to en-bloc versus conventional TURBT for BC (NCT04712201). Inclusion criteria comprehended patients affected by primary or recurrent BC, located anywhere in the bladder, with a maximum of 3 separated lesions and/or with a maximum size of 3 cm per each lesion. As part of the secondary endpoints of the study, an ad-hoc classification of BP was created and prospectively applied between April 2018 and June 2021. A total of 248 patients were included in the final analysis. The study was suspended between March 2020 and September 2020 due to SARS-CoV-2 pandemic and in this period of time no patient was considered for eligibility. This study respected the principles of the Declaration of Helsinki and was approved by the Institutional Review Board (2017/09c). All participants were adequately informed and provided a written consent.
Surgical procedure
The patient was placed in the standard lithotomy position under spinal or general anesthesia. Conventional TURBT was performed with standard monopolar and bipolar loops. En-bloc TURBT was carried out with monopolar Collins loop, bipolar rectangular loop (Karl Storz, Tuttlingen, Germany) or 550-µm fiber connected to a thulium laser generator (Revolix Duo, LisaLaser, Katlenburg-Lindau, Germany) set to 10–20 W power. En-bloc TURBT technique provided for a circular incision around the base of the lesion with a margin of 5–10 mm of healthy mucosa. The lesion was then bluntly dissected form the bladder wall at the desired depth. After specimen extraction either through the resectoscope or with a Toomey evacuator, a careful hemostasia of the resection bed was carried out. A 20–22 Ch three-way bladder catheter was inserted at the end of the procedure, and continuous bladder irrigation was started. In accordance with our institution's protocol, six additional biopsies were performed to detect subclinical carcinoma in situ in patients with primo-resection, recurrence with positive cytology and/or prior high-grade BC.
TURBTs were performed by experienced, dedicated, surgeons or resident under the direct supervision of a senior surgeon. When the procedure was performed by a resident, intraoperative assessment of resection depth and DEEP grade was performed and recorded by the senior surgeon. All tumor samples were examined by a dedicated uropathologist (F.A.). Early postoperative instillation of 40 mg mitomycin C or 50 mg epirubicin was administered according to current guidelines. The postoperative course and follow-up protocol were planned according to the institutional protocol. The complications were evaluated at 30 days according to Clavien–Dindo classification [9].
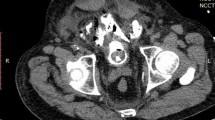
DEpth of Endoscopic Perforation (DEEP) scale
Four grades of vesical endoscopic perforation during TURBT were defined (Fig. 1). Grade 0 indicates that, after the resection, the vesical muscular layer is visible with no sign of perivesical fat. In grade 1, the vesical muscular layer is visible with some spots of perivesical fat. Grade 2 identifies those cases where the muscular layer was completely resected with the exposition of the perivesical fat (extraperitoneal perforation). Grade 3 indicates the resection of muscular layer, perivesical fat and peritoneum (intraperitoneal perforation). Grade 2 (extraperitoneal) and grade 3 (intraperitoneal) perforations were defined as high-grade complications as they could significantly affect the postoperative course of patients.
Grades of DEEP scale: (0) vesical muscular layer is visible with no sign of perivesical fat, (1) the vesical muscular layer is visible with some spots of perivesical fat, (2) the muscular layer is completely resected with the exposition of the perivesical fat (extraperitoneal perforation) (3) muscular layer, perivesical fat and peritoneum are perforated (intraperitoneal perforation)
Statistical analysis
Data were represented by descriptive statistical analysis. The quantitative variables were reported as median and interquartile range (IQR). The qualitative variables were described as absolute number and frequency. Differences between study groups in variables were analyzed with Chi-square test in categorical or nominal variables (or Fisher test) and with T Test in continuous variables. Variables with p < 0.20 in univariate analysis were included in multivariate logistic and linear regression (MVA) models to assess predictors of high-grade perforation according to the DEEP scale (Table 2) and predictors of major postoperative complications (Clavien–Dindo classification > 2) (Supplementary Table 1), administration of intravesical chemotherapy (Supplementary Table 2), postoperative irrigation time (Supplementary Table 3), length of stay (Supplementary Table 4), and catheterization time (Supplementary Table 5). All the tests were conducted at a significance level p = 0.05. Statistical analyses were performed using SPSS v.26 (IBM Corp., Armonk, NY).
Results
A total of 140 patients underwent en-bloc TURBT and 108 conventional TURBT. Population and operative characteristics are summarized in Table 1. After resection, 146/248 (58.9%), 56/248 (22.6%), 41/248 (16.5%), 5/248 (2.0%) patients presented a DEEP grade 0, 1, 2, and 3, respectively. All cases of intraperitoneal bladder perforation were treated conservatively with prolonged catheterization (5–7 days) and no surgical repair was ultimately required.
Preoperative predicting factors
Pre-operative variables distributed by DEEP grades are shown in Table 2. High-grade DEEP (grade 2–3) were more frequent in case of tumors located at the lateral walls (17.7% and 3.1% for grade 2 and 3, respectively) of the bladder and anterior wall/dome/neck (23.1% and 0% for grade 2 and 3, respectively) in respect to lesions found in the trigone and posterior walls (11.4% and 1.3% for grade 2 and 3, respectively).
A linear regression analysis was performed to investigate the pre- and intra-operative variables that could be correlated with higher grade of DEEP scale (Table 2). At MVA, female gender [B coeff. 0.255; 95% CI 0.001–0.513; p = 0.05], tumor location [B coeff. 0.188 (0.026–0.339); p = 0.015], and obturator nerve reflex [B coeff. 0.503(0.148–0.857); p = 0.006] were independent predictors of higher DEEP grades.
Post-operative variables
Post-operative variables distributed by DEEP grades are reported in Table 3. The rate of post-operative intravesical mitomycin administration was lower in high-grade perforations (p < 0.001), while the rate of complications (p = 0.019) and major complications (p < 0.001), length of irrigation (p < 0.001), length of catheterization (p = 0.017), and hospitalization time (p = 0.002) were higher compared to grade 0–1 perforations.
In UVA, DEEP grade was significantly associated with the absence of post-operative intravesical instillation (OR = 5.579; p < 0.001), major complications (OR = 2.105; p = 0.035), length of irrigation (OR = 0.316; p < 0.001) and hospitalization time (OR = 0.385; p < 0.001). In MVA, DEEP scale remained an independent predictor of major complication [OR = 2.221 (1.098–4.495); p = 0.026], adjusted for age and surgeon experience (Supplementary table 1–5). DEEP scale [OR = 9.387 (2.434–36.20); p = 0.001] and female gender [OR = 6.727 (1.029–44.001); p = 0.047] were associated with no post-operative intravesical instillation in MVA adjusted for age, technique, and surgeon experience. DEEP scale [B. coeff 0.299 (0.166–0.441); p < 0.001] and age [B. coeff 0.019 (0.008–0.029); p = 0.001] independently predicted length of irrigation in MVA adjusted for surgical duration. DEEP scale [B. coeff 0.315 (0.111–0.519); p = 0.003], duration of surgery [B. coeff 0.013 (0.001–0.024); p = 0.036], and age [B. coeff 0.035 (0.020–0.050); p < 0.001] were independent predictors for hospital stay in MVA adjusted for history of BC and tumor size. The length of catheterization was not associated DEEP scale (p = 0.11).
Discussion
In this prospective study, we developed a novel classification of bladder perforation during TURBT, reporting the predictors of DEEP perforation and the implication of this classification in the postoperative course. The rate of extraperitoneal (grade 2) and intraperitoneal (grade 3) perforations were 16.5% and 2.0%, respectively. These findings are in line with previous published data from our Institution where extraperitoneal perforation represented up to 83% of all BP. However, the perforation rate was lower than in the current study (1.3% vs 18.5%)[10]. This result may be influenced by several factors. It is acknowledged that the intraoperative complications are underreported due to lack of proper definition and, possibly, to a certain fear of consequential lawsuit [8]. The prospective fashion of this study increases the completeness of data recording in comparison to retrospective reports. Finally, the primary endpoint of this randomized-controlled trial was the presence of detrusor muscle, which may have led the surgeons to provide a muscle sampling higher than in routinary practice. The location of the bladder tumor was independent predictor of BP, as for the obturator nerve reflex. These results are expected, since it is technically easier to perform a trigone/posterior bladder wall resection and the obturator nerve reflex determines a leg adduction that may result in uncontrolled bladder resections. The female gender was an independent predictor of bladder perforation. This may reflect the bladder wall thickness of female patients, which is usually thinner than the male bladder wall due to the absence of bladder outlet obstruction.
The use of DEEP scale may be beneficial as high-grade perforations have proven to impact the clinical and surgical outcomes. In particular, the administration of immediate intravesical chemotherapy depended on the grade of DEEP. This is a crucial point, since it has been demonstrated that in low-risk bladder cancers, the postoperative instillation of chemotherapeutic agents decreases bladder cancer recurrence. Comploj et al. reported that the BP influences the natural history of superficial bladder cancer, resulting in a higher rate of bladder recurrence with no impact on overall and cancer-specific survival [11]. The authors postulated that the recurrence could depend on two factors: tumor seeding or implantation and inadequate initial tumor resection due to BP [11]. It should also be acknowledged the risk of intraperitoneal seeding, which occurrence may be considered anecdotical [12,13,14].
Furthermore, the rate of major postoperative complication, the irrigation time and the hospital stay were related to DEEP. Thus, the systematic use of DEEP scale might help to direct the postoperative management of the patients, adapting the postoperative strategies to the depth of endoscopic perforation.
The study is not devoid of limitations. First, we could not separate the patients treated with en-bloc and conventional TURBT due to paucity of high-grade perforations. However, the DEEP scale was designed to report the depth of endoscopic perforation independently from the type of resection or the energy source used. Therefore, the use of this classification should apply to any kind of TURBT. Second, as our study was not designed a priori to assess the reproducibility of the scale, future studies are warranted to assess inter- and intra-observer agreement. Third, this a result of a single-center randomized trial. The DEEP scale should be externally validated before clinical implementation. However, the present study demonstrated that this classification provides a standardized tool to classify the most important intraoperative complication of TURBT, that affects the clinical postoperative course. Its use could be implemented in daily practice.
Conclusion
Female gender, tumor located in anterior wall/neck or dome, and obturator nerve reflex are independent predictors of intra/extraperitoneal perforation. The DEEP scale is an independent predictor of postoperative clinical course, such as post-operative intravesical instillation, the risk of major complication, the irrigation time and hospital stay. This scale provides a standardized tool to classify the most important intraoperative complication of TURBT, that affects clinical postoperative course.
Abbreviations
- BP:
-
Bladder perforation
- cTURBT:
-
Conventional transurethral resection of bladder tumor
- EAU:
-
European Association of Urology
- ERBT:
-
En-bloc resection of bladder tumor
- MVA:
-
Multivariate regression analysis
- NMIBC:
-
Non-muscle invasive bladder cancer
- TURBT:
-
Transurethral resection of bladder tumor
- UVA:
-
Univariate regression analysis
References
Babjuk M, Burger M, Capoun O, Cohen D, Compérat EM, Dominguez Escrig JL et al (2022) European association of urology guidelines on non-muscle-invasive bladder cancer (Ta, T1, and Carcinoma in Situ). Eur Urol 81:75–94. https://doi.org/10.1016/j.eururo.2021.08.010
Horwich A, Babjuk M, Bellmunt J, Bruins HM, De Reijke TM, De Santis M et al (2019) EAU-ESMO consensus statements on the management of advanced and variant bladder cancer-an international collaborative multi-stakeholder effort: under the auspices of the EAU and ESMO Guidelines Committees†. Ann Oncol 30:1697–1727. https://doi.org/10.1093/annonc/mdz296
Cornu JN, Herrmann T, Traxer O, Matlaga B (2016) Prevention and management following complications from endourology procedures. Eur Urol Focus 2:49–59. https://doi.org/10.1016/j.euf.2016.03.014
Akand M, Muilwijk T, Raskin Y, De Vrieze M, Joniau S, Van Der Aa F (2019) Quality control indicators for transurethral resection of non-muscle-invasive bladder cancer. Clin Genitourin Cancer 17:e784–e792. https://doi.org/10.1016/j.clgc.2019.04.014
Traxer O, Pasqui F, Gattegno B, Pearle MS (2004) Technique and complications of transurethral surgery for bladder tumours. BJU Int 94:492–496. https://doi.org/10.1111/j.1464-410X.2004.04990.x
Lonati C, Esperto F, Scarpa RM, Papalia R, Gómez Rivas J, Alvarez-Maestro M et al (2021) Bladder perforation during transurethral resection of the bladder: a comprehensive algorithm for diagnosis, management and follow up. Minerva Urol Nephrol. https://doi.org/10.23736/S2724-6051.21.04436-0
Biyani CS, Pecanka J, Rouprêt M, Jensen JB, Mitropoulos D (2020) Intraoperative Adverse Incident Classification (EAUiaiC) by the European association of urology ad hoc complications guidelines panel. Eur Urol 77:601–610. https://doi.org/10.1016/j.eururo.2019.11.015
Cacciamani G, Sholklapper T, Sotelo R, Desai M, Gill I (2021) A protocol for the development of the intraoperative complications assessment and reporting with universal standards criteria: the ICARUS project. Int J Surg Protoc 25:160–164. https://doi.org/10.29337/ijsp.155
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Collado A, Chéchile GE, Salvador J, Vicente J (2000) Early complications of endoscopic treatment for superficial bladder tumors. J Urol 164:1529–1532
Comploj E, Dechet CB, Mian M, Trenti E, Palermo S, Lodde M et al (2014) Perforation during TUR of bladder tumours influences the natural history of superficial bladder cancer. World J Urol 32:1219–1223. https://doi.org/10.1007/s00345-013-1197-x
Ohguchi N, Sakaida N, Okamura A, Kawakita S, Kawamura H, Matsuda T (1997) Extravesical tumor implantation caused by perforation during transurethral resection of a bladder tumor: a case report. Int J Urol 4:516–518. https://doi.org/10.1111/j.1442-2042.1997.tb00296.x
Kim JH, Yang WJ (2014) Delayed spontaneous perforation of urinary bladder with intraperitoneal seeding following radical transurethral resection of invasive urothelial cancer: a case report. BMC Res Notes 7:167. https://doi.org/10.1186/1756-0500-7-167
Skolarikos A, Chrisofos M, Ferakis N, Papatsoris A, Dellis A, Deliveliotis C (2005) Does the management of bladder perforation during transurethral resection of superficial bladder tumors predispose to extravesical tumor recurrence? J Urol 173:1908–1911. https://doi.org/10.1097/01.ju.0000158450.71497.ae
Author information
Authors and Affiliations
Contributions
AB: protocol/project development, manuscript editing. AG: protocol/project development, data analysis, manuscript writing. PD: data collection, data analysis, manuscript writing. MF: data collection. AT: data collection, data analysis, manuscript editing. JG: data collection, data analysis. ÓR-F: data collection, data analysis. JH: data collection. AP: data collection. PV: data collection, manuscript editing. MB: manuscript editing. JA: data collection, manuscript writing. FA: data collection, data analysis. JP: project development.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Research involving human participants and/or animals
This study respected the principles of the Declaration of Helsinki and was approved by the Institutional Review Board (2017/09c).
Informed consent
All participants were adequately informed and provided a written consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Breda, A., Gallioli, A., Diana, P. et al. The DEpth of Endoscopic Perforation scale to assess intraoperative perforations during transurethral resection of bladder tumor: subgroup analysis of a randomized controlled trial. World J Urol 41, 2583–2589 (2023). https://doi.org/10.1007/s00345-022-04052-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-04052-w