Abstract
Purpose
The treatment landscape in metastatic renal cell carcinoma (mRCC) has evolved dramatically in recent years. Within the German guideline committee for RCC we evaluated current medical treatments and gave recommendations.
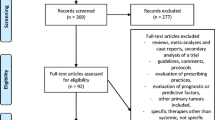
Methods
A systematic review of published evidence for medical treatment of mRCC was performed (July 2016–August 2019) to cover the duration from last guideline update in 2016. Evidence was graded according to SIGN (http://www.sign.ac.uk/pdf/sign50.pdf). Recommendations were made on the basis of a nominal group work with consensus approach and included patient advocates and shareholder of the German RCC treatment landscape. Each recommendation was graded according to its strength as strong recommendation (A) or recommendation (B). Expert statements were given, where appropriate.
Results
Strong first-line recommendations (IA) exist for axitinib + pembrolizumab (all risk categories) and ipilimumab + nivolumab (intermediate or poor risk only). Axitinib + avelumab is a recommended first-line treatment across patients with any risk category (IB). In patients who are not candidates for immune check point inhibitor (ICI) combinations, targeted agents should be offered as an alternative treatment. Subsequent treatment after ICI-based combinations remain ill-defined and no standard of care can be formulated.
Conclusion
ICI-based combinations are the first-line standard of care and should be considered accordingly. There is an unmet medical need for pivotal studies that define novel standards in patients with failure of ICI-based combinations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The landscape for systemic therapy in metastatic renal cell carcinoma (mRCC) has changed dramatically in recent years. Today, tyrosine kinase inhibitors (TKI), inhibitors of the mammalian target of rapamycin (mTORi) and immune checkpoint inhibitors (ICI) as single agent or combination therapies built the backbone of medical treatment. As a tribute to the rapid development novel combinations with 3rd generation TKI have reported positive results and are 1st line candidates for approval. These trials reported after the search period for our systematic review and are not subject for consideration. Our analysis was performed with the intention to build an evidence-based approach for agents currently licensed by the European Medicines Agency (EMA) at the time of literature search. The German version of treatment recommendations can be accessed online.Footnote 1
First-line therapy in clear cell RCC
Treatment recommendations are based on the International Metastatic RCC Database Consortium (IMDC) risk categories [1]. Individual disease parameters are subjective and therefore will not be discussed in this article. However, they are considered appropriate for individualization of treatment options in the clinic. Given the existing differences among these first line studies, advantages and disadvantages of a given treatment should be weighed in the context of the therapeutic aim (such as long-term outcome or symptom control) for individualized treatment selection.
CM214 was the first immune combination (ipilimumab + nivolumab) that reported improved clinical outcome parameters when compared with sunitinib, which is the trial with the most mature data today. However, the primary endpoint was based on patients with at least 1 risk factor only and reflects therefore a selection of patients with worse prognosis. In contrary, JR101 and KN426 trials considered all risk categories for their primary analysis appropriate and compared axitinib with either avelumab or pembrolizumab to sunitinib. These three trials are considered milestones in the development of ICI-based combinations in mRCC and their key parameter are listed in Table 1. Differences between trial populations exist and do not warrant direct comparison between trials. Therefore, Table 1 should be considered as reference of key parameters of these trial only.
Based on these findings, recommendations considered axitinib + pembrolizumab and ipilimumab + nivolumab standard first-line options (both IA recommendations), which showed OS benefit (Table 2) [2, 3]. Axitinib + avelumab is considered as another option, but the pivotal trial did not report a statistically significant OS benefit in the interim analysis (Table 2) [4]. The principle activity of this regimen supports its use, but the lack of OS advantage has led to a IB recommendation.
The choice between treatments should take the pros and cons of each option into account and also consider patient and tumor parameters to individualize therapy to the needs of a patient. A therapeutic aim should be formulated and the most appropriate regimen chosen. For instance, high tumor burden or critical anatomical location as well as symptomatic disease have a short-term aim of disease- and symptom-control. This may favor regimens with the highest chance for response, such as axitinib + avelumab (ORR: 52.5%) or pembrolizumab (ORR: 60.2%) [2, 4]. On the contrary, ipilimumab + nivolumab has reported favorable long-term results, with a median follow-up of 55 months, indicating durable responses for this TKI-free regimen [5]. Differences in the tolerability profile exist between regimen (Table 1), which may contribute to differences in health-related quality of life (HR-QoL) or symptom scale measures. Axitinib-based combinations require chronic TKI exposure, these agents did not report benefit in patient reported outcomes (PRO) [6]. On the contrary, the TKI-free combination of ipilimumab + nivolumab was associated with an improvement in FKSI-19 (total score), when compared to sunitinib [7].
More recently, 3rd generation TKI reported positive phase III trials in first-line treatment. Cabozantinib + nivolumab reported a HR for OS of 0.60 (98.9%CI 0.40–0.89; P = 0.001) and was recently approved by EMA as a novel first line option [8]. Moreover, Lenvatinib + pembrolizumab achieved a HR for OS of 0.66 (95%CI 0.49–0.88; P = 0.005), thereby underscoring the relevance of the 3rd generation TKI as combination partners [9]. These agents will be formally discussed within the next update of the German guideline.
Patients who are not candidates for ICI combinations should receive a VEGF targeted therapy as an alternative treatment. Based on previous studies in mRCC a differential recommendation for VEGF targeting agents exists. IMDC risk categories were used to categorize these recommendations and are depicted in Table 3. While these VEGF targeting agents received a stronger recommendation in patients with favorable risk (IA), they may also be offered in patients with at least one risk factor (IB).
Treatment of patients with favorable risk
Ipilimumab + nivolumab was not superior to sunitinib treatment neither in regard to efficacy parameters nor OS and is therefore not recommended in favorable risk patients (Tables 2 and 4) [5]. Treatment choices consider ICI combinations as the mainstay of therapy, which may consist of axitinib + pembrolizumab or avelumab (Table 2). For both pivotal trials data remains still immature for the subgroup of patients with a favorable risk profile. In these patients, a higher anti-tumor activity was detected compared to sunitinib, but no significant OS benefit was noted between groups (Table 4) [10, 11]. Hence, overall superiority for ICI combinations over sunitinib could not be shown in this group of patients. However, the low event rate renders this analysis immature and no conclusive statement in regard to OS can be given. In spite of these limitations, single agent TKI treatment may be offered to patients who are not candidates for surveillance and do not require the higher chance for response or PFS advantage, which is associated with axitinib-based combinations.
Treatment of patients with intermediate or poor risk
Patients with at least 1 risk factor derive a substantial treatment benefit from ICI-based combinations and reflect therefore the standard of care (Table 2). Superiority for overall survival was consistent across all ICI-combinations (Table 4) although effect size in efficacy parameter varied between studies. The choice between ipilimumab + nivolumab, axitinib + pembrolizumab or avelumab should be made according to individual patient parameters, as outlined above.
Second line therapy in clear cell RCC
A high level of evidence exists after the failure of monotherapy with a TKI. In this uncommon clinical scenario, cabozantinib or nivolumab are considered standards of care and receive the strongest recommendation (IA) (Table 5) [12, 13]. Lenvatinib + everolimus has randomized phase II data supporting its use after TKI failure, which renders it a treatment option but with a weaker recommendation (IB) (Table 5) [14].
With the rapidly changing first-line landscape, data remains scarce for subsequent therapies after ICI-based combinations. The paucity of randomized clinical data in this treatment scenario was prohibitive to formulate a standard of care. Instead, statements of expert opinions were formulated to guide the treatment choice. Given the principle activity of TKIs after ICI-based therapies in retrospective series, a TKI-based therapy was considered appropriate after ipilimumab + nivolumab or axitinib + pembrolizumab or avelumab (Table 6) [15, 16]. In the rare event that first-line therapy consisted of an mTOR inhibitor, either a TKI-or based therapy or nivolumab are considered appropriate (Table 6).
Third line therapy
There is no standard of care defined and no specific recommendation can be given. Given the differences in the mechanism of action or kinase inhibitory profile, the subsequent therapy should consist of an agent that has not been used in previous therapies (Table 7).
Non-clear cell renal cell carcinomas
Non-clear cell histologies resemble a heterogenous group of patients and they account for about 20–25% of RCC [17]. Today, there is an increasing body of evidence that supports the classification of these tumors as distinct entities. The molecular diversity of these cancers paved the way for a differential drug development and renders the summation of these tumors as one heterogenous group of RCCs obsolete. However, clinical data remains scarce and the current guideline version does not include specific recommendations for these rare entities. This section is subject for recommendations in future versions of our guideline.
Of note, the term sarcomatoid RCC is frequently used, but this does not represent a classified group of RCC. Instead it is an advert biologic feature, which may occur in any RCC entity [18]. Clinical data for medical treatment of this subgroup is mainly derived from randomized clinical trials, which included ccRCC only. Hence, the majority of clinical data for treatment represent ccRCC with a sarcomatoid component, which should be differentiated from other sarcomatoid RCC (non-clear) entities. Furthermore, pure mesenchymal renal tumors represent a distinct class of renal malignancies and should be reported and treated accordingly.
Availability of data and materials
NA.
Code availability
NA.
References
Heng DYC, Xie W, Regan MM et al (2009) Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol 27:5794–5799
Rini BI, Plimack ER, Stus V et al (2019) (2019) Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med 380:oa1816714
Motzer RJ, Tannir NM, McDermott DF et al (2018) Nivolumab plus Ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med 380:oa1712126
Motzer RJ, Penkov K, Haanen J et al (2019) Avelumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med 3880:oa1816047
Albiges L, Tannir NM, Burotto M et al (2020) Nivolumab plus ipilimumab versus sunitinib for first-line treatment of advanced renal cell carcinoma: extended 4-year follow-up of the phase III CheckMate 214 trial. Esmo Open 5:e001079
Jens B, Brian R, Elisabeth P, et al (2020) Health-related quality-of-life (HRQoL) analysis from KEYNOTE-426: pembrolizumab (pembro) plus axitinib (axi) vs sunitinib for advanced renal cell carcinoma (RCC) [Internet], in virtual, 2020, p Virtual room 1. https://resource-centre.uroweb.org/resource-centre/EAU20V/212868/Abstract/. Accessed 12 Apr 12 2021
Cella D, Grünwald V, Escudier B et al (2019) Patient-reported outcomes of patients with advanced renal cell carcinoma treated with nivolumab plus ipilimumab versus sunitinib (CheckMate 214): a randomised, phase 3 trial. Lancet Oncol 20:297–310
Choueiri TK, Powles T, Burotto M et al (2021) Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. New Engl J Med 384:829–841
Motzer R, Alekseev B, Rha S-Y et al (2021) Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. https://doi.org/10.1056/NEJMoa2035716
Powles T, Plimack ER, Soulières D et al (2020) Pembrolizumab plus axitinib versus sunitinib monotherapy as first-line treatment of advanced renal cell carcinoma (KEYNOTE-426): extended follow-up from a randomised, open-label, phase 3 trial. Lancet Oncol 21:1563–1573
Choueiri T, Motzer R, Rini B et al (2020) Updated efficacy results from the JAVELIN Renal 101 trial: first-line avelumab plus axitinib versus sunitinib in patients with advanced renal cell carcinoma. Ann Oncol. https://doi.org/10.1016/j.annonc.2020.04.010
Choueiri TK, Escudier B, Powles T et al (2015) Cabozantinib versus everolimus in advanced renal-cell carcinoma. N Engl J Med 373:1814–1823
Motzer RJ, Escudier B, McDermott DF et al (2015) Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med 373:1803–1813
Motzer RJ, Hutson TE, Glen H et al (2015) Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial. Lancet Oncol 16:1473–1482
Albiges L, Fay AP, Xie W et al (2015) Efficacy of targeted therapies after PD-1/PD-L1 blockade in metastatic renal cell carcinoma. Eur J Cancer 51:2580–2586
Nadal R, Amin A, Geynisman DM et al (2016) Safety and clinical activity of vascular endothelial growth factor receptor (VEGFR)–tyrosine kinase inhibitors after programmed cell death 1 inhibitor treatment in patients with metastatic clear cell renal cell carcinoma. Ann Oncol 27:1304–1311
Moch H, Cubilla AL, Humphrey PA et al (2016) The 2016 WHO classification of tumours of the urinary system and male genital organs-part a: renal, penile, and testicular tumours. Eur Urol 70:93–105
Cimadamore A, Cheng L, Scarpelli M et al (2020) Towards a new WHO classification of renal cell tumor: what the clinician needs to know: a narrative review. Transl Androl Urol 10:1501520–1506520
Acknowledgements
Heidrun Rexer, who assembled the German RCC Guideline. Christian Doehn and Susanne Krege who chaired the German RCC Guideline.
Funding
Open Access funding enabled and organized by Projekt DEAL. The German treatment guideline received financial support through the German Guidelines in Oncology Program of the German Cancer Aid.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception, design and development of recommendations. The first draft of the manuscript was written by Viktor Grünwald and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
VG: received research support, personal fees from Astra Zeneca, Bristol-Myers Squibb, MSD Sharp & Dohme, Ipsen, Pfizer. Personal fees from Merck Serono, EUSAPharm, Novartis, Lilly, Eisai, Roche, Janssen-Cilag. LB: no conflicts of interest to declare that are relevant to the content of this article. BB: received personal fees from BMS, Novartis, Pfizer.BE: received personal fees from GSK, Pfizer. TG: received personal fees from BMS, Merck Serono, MSD, Ipsen, Novartis, EISAI. GG: received personal fees from Ipsen, AstraZeneca, BMS. JG: received personal fees from Bayer, Roche, MSD, Janssen, Amgen, BMS. KK: no conflicts of interest to declare that are relevant to the content of this article. MJ: received personal fees from Pfizer, BMS, Janssen-Cilag, Hexal, EISAI, Sanofi, Bayer, Novartis, Astellas, Medac, Roche. TK: received personal fees from Janssen-Cilag, Bayer, Astellas, Pfizer, BMS, Novartis. CP: received personal fees from MSD. MS: no conflicts of interest to declare that are relevant to the content of this article. MStae: received personal fees from Pfizer, GSK, Novartis, Bayer, Roche, Aveo, EUSAPharm, Astellas, Ipsen, Exelexis, Pelleton, EISAI.
Research involving human participants, their data or biological material
This is a systematic review and consensus approach that assessed the value of existing data in regard to its clinical applicability. All data comes from published evidence from trials that followed current ethical standards. We did not generate new data at any stage of our process. This paper does not apply to an ethics committee approval. There is no indication for an informed consent of patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grünwald, V., Bergmann, L., Brehmer, B. et al. Systemic therapy in metastatic renal cell carcinoma (mRCC): an evidence-based recommendation of the German interdisciplinary RCC guidelines group. World J Urol 40, 2381–2386 (2022). https://doi.org/10.1007/s00345-022-04015-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-04015-1