Abstract
Purpose
To systematically review studies focused on screening programs for renal cell carcinoma (RCC) and provide an exhaustive overview on their clinical impact, potential benefits, and harms.
Methods
A systematic review of the recent English-language literature was conducted according to the European Association of Urology guidelines and the PRISMA statement recommendations (PROSPERO ID: CRD42021283136) using the MEDLINE, Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov databases. Risk-of-bias assessment was performed according to the QUality In Prognosis Studies (QUIPS) tool.
Results
Overall, nine studies and one clinical trials were included. Eight studies reported results from RCC screening programs involving a total of 159 136 patients and four studies reported screening cost-analysis. The prevalence of RCC ranged between 0.02 and 0.22% and it was associated with the socio-demographic characteristics of the subjects; selection of the target population decreased, overall, the screening cost per diagnosis.
Conclusions
Despite an increasing interest in RCC screening programs from patients and clinicians there is a relative lack of studies reporting the efficacy, cost-effectiveness, and the optimal modality for RCC screening. Targeting high-risk individuals and/or combining detection of RCC with other health checks represent pragmatic options to improve the cost-effectiveness and reduce the potential harms of RCC screening.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
The incidence of renal cell carcinoma (RCC) is increasing, with over 430.000 new cases diagnosed per year and over 175.000 new deaths per year in 2020 worldwide [1]. Risk factors for RCC are well established and include older age, male sex, smoking, hypertension, and obesity [2]. The persistent increase in incidence is most likely related to both an increase in risk factors prevalence in the society and to a higher incidence in incidental detection [3,4,5]; such epidemiological signature confirms the unmet need to reduce overdiagnosis and overtreatment in the future [6].
Although most RCCs are diagnosed at an early stage in asymptomatic patients [7] and up to 25% present with metastasis showing a 1-year and 5-year survival of 39% and 12% versus 96% and 86% in patients diagnosed with a stage I disease [8]. These figures make RCC one of the deadliest genitourinary tumors [9]. Moreover, if diagnosed at an advanced stage, RCC is not likely curable by surgery alone, increasing the complexity and costs of treatment, as well as a non-negligible risk of adverse events, with worse patient-reported outcomes.
Taken together, the increasing prevalence of RCC risk factors in the general population [10], coupled with a high proportion of asymptomatic patients and a high mortality rate make RCC suitable for screening programs. The ultimate objective of such programs should be to increase the detection of early stage tumors that deserve timely treatment, to improve survival outcomes, the patient’s quality of life, and to decrease healthcare costs, toward the concept of value-based healthcare [11].
Focused renal ultrasound (US) has been reported to be a cost-effective tool with a potential survival benefit associated with early detection through RCC screening [12, 13]. In addition, several liquid biomarkers, focusing on genetic or metabolic assays, and innovative imaging tools, have been recently tested for the detection of RCC [14]. Despite being attractive non-invasive diagnostic modalities, none of them have been validated or shown to have clinical utility to be implemented in the daily practice [14].
Overall, screening programs targeting high-risk individuals have the potential to be cost-effective strategies to improve RCC care. However, several uncertainties still remain, including the magnitude of the benefit of early treatment, the overall cost-effectiveness of the screening, the optimal screening modality and target population, as well as the potential harms of screening programs [15]. In fact, a possible drawback of any screening program is the risk of overdiagnosis, psychological distress, and financial toxicity for both individual patients and the whole society [12, 15].
The aim of this systematic review is to summarize the current evidence on available screening programs for RCC, focusing on their potential benefits, harms, and impact on current and future clinical practice.
Materials and methods
Evidence acquisition
This systematic review was conducted according to the principles highlighted by European Association of Urology (EAU) Guidelines Office [16] and the updated Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) recommendations [17].
Review protocol
The methods for this systematic review were summarized following the PRISMA for Protocols 2015 (PRISMA-P 2015) statement recommendations (www.equator-network.org/reporting-guidelines/prisma-protocols/) [18]. The protocol was registered in the International Prospective Register of Ongoing Systematic Reviews (PROSPERO, http://www.crd.york.ac.uk/prospero) on December 20th, 2021 (registration ID: CRD42021283136).
Search strategy
A systematic review of the English-language literature was performed according to the PRISMA criteria [17] using the Medline, Web of Science and Embase databases in November 2021. In addition, ClinicalTrials.gov was searched on December 15th, 2021 for potential clinical trials on RCC screening.
The literature search used both free text and MeSH terms (keywords: “screening” OR “cancer screening” AND “renal cell carcinoma” OR “renal neoplasm” OR “renal cancer” OR “kidney cancer” OR “kidney neoplasm”). A detailed overview of the search strategy is available in the Appendix. The search strategy was adapted for the databases other than MEDLINE, as appropriate. An updated search was performed on December 15th, 2021 to identify additional relevant records. A manual search of bibliographies from included studies and previous systematic reviews was also performed.
Eligibility criteria
A specific population (P), intervention (I), comparator (C), and outcome (O) framework defined the study eligibility, as recommended [16, 19]. In brief, studies were considered eligible if they fulfilled the following criteria:
-
(P): adult (> 18 years) healthy subjects or adult individuals at higher risk of developing renal cell carcinoma (RCC) based on established risk factors (age, male gender, family history, smoking, obesity, diabetes, hypertension) with no prior history of RCC (or prior imaging showing a renal mass) and no prior history of diseases increasing the risk of RCC (including genetic syndromes);
-
(I): any screening intervention (opportunistic or population screening), including any type of medical test (liquid biomarkers, non-invasive imaging, renal biopsy);
-
(C): either comparative or non-comparative studies;
-
(O): cost-effectiveness of the screening program (detection rate of histologically confirmed RCC vs costs of the screening program).
-
Studies assessing the impact of screening programs on the detection of renal masses of undetermined nature (with no histopathological data) were excluded. Studies with insufficient reporting of the PICOS criteria were also excluded.
Study selection
Mendeley reference software removed duplicate records identified. The title and abstract of all retrieved records were screened independently by two review authors to identify records reporting the use of biomarkers or imaging tests for screening of RCC. Disagreement was solved by a third party, who supervised the review process. The list of articles judged highly relevant was reviewed by all co-authors until final consensus was reached. Three independent review authors checked the study eligibility after full-text assessment. Separate screening forms were created for each selection phase. Disagreement was solved by a third party. The records not meeting the PICO framework of this review were finally excluded. The flowchart depicting the overall review process according to the PRISMA statement recommendations [19] is shown in Fig. 1.
Data collection and risk of bias assessment
Data from the studies included in the review were extracted by two authors in a a-priori developed data extraction form. The reliability and completeness of data extraction was crosschecked by another member of the review team. When more than one article was based on the same study population, we included the most recent report.
The same authors independently performed a formal risk of bias assessment using the QUality In Prognosis Studies (QUIPS) tool [20]. A third reviewer acted as an arbitrator. The QUIPS tool provides a measure of the risk of bias over six domains of interest (Supplementary Table 1).
The overall quality of evidence was assessed according to Grading of Recommendations Assessment, Development, and Evaluation (GRADE) recommendations (https://www.gradeworkinggroup.org; www.handbook.cochrane.org).
A narrative format was used for evidence synthesis. Due to the quality and heterogeneity of the included studies, a quantitative synthesis of the evidence was not performed.
Results
Study selection
The literature search identified 31,561 records and 82 clinical trials. Of these, 30,749 studies were excluded by title and abstract screening, with a further 797 and 81 clinical trials excluded after full-text assessment. Of the records screened, 9 studies and one clinical trial focused on RCC screening and fulfilling all the PICO criteria and were, therefore, included in the qualitative analysis (Table 1). Only four studies (Table 2) analyzed the costs of a RCC screening program. The study selection process is summarized in the PRISMA flowchart (Fig. 1).
Study characteristics and risk of bias
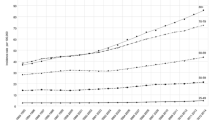
Overall, eight studies reported a study population and involved a total of 159,136 patients (Table 1). Four studies performed a cost-analysis of a RCC screening program; three of these included a specific study population (Table 2) and one study was focused on a detailed cost analysis based on a decision model evaluating screening in asymptomatic individuals using focused US. Risk-of-bias assessment according to the QUIPS tool [20] is shown in Supplementary Table 1 and Fig. 2; the study confounding domain had the highest proportion of studies with high risk of bias (55.6%). The overall quality of evidence according to GRADE was low.
Qualitative evidence synthesis
A detailed overview of the results of the studies assessing the benefits and harms of available RCC screening programs reporting a clear target population is shown in Table 1. Regarding the imaging modality for RCC screening, five studies employed ultrasound (US), one computed tomography (CT) scans, one positron emission tomography (PET), and one both CT scan and US.
Ono et al. [21] investigated the detection rate of a variety of cancers using whole-body PET for screening 3426 asymptomatic individuals, focusing on their clinical and pathological stages. Overall, the authors found one stage IV RCC in the PET positive group, while one stage I RCC and one stage III RCC in the PET negative group.
Malaeb et al. [22] investigated the power of US for screening 6678 consecutive patients in conjunction with the Aneurysm Detection and Management study. Overall, 817 (12.3%) renal anomalies were found, including a solid renal mass in 22 (0.32%) patients. Confirmatory CT or MRI was used in the 22 patients with solid renal masses. Histopathological confirmation after surgery could only be obtained in 15 RCC as five patients were lost during the follow-up and two were poor surgical candidates. The tumors were staged pT1 in 10 cases and pT3 in five cases; of the latter, two patients had a node positive disease and one had metastases at diagnosis. The histological classification included 13 cases of clear cell carcinoma, one of granular tumor and one of papillary tumor.
Mizuma et al. [23] investigated the findings of the first sonographic screening of 16,024 healthy subjects to assess the validity of US-based screening for abdominal cancers in an asymptomatic population. Four patients were diagnosed with RCC through the screening program and one was missed by US. All patients diagnosed with RCC by screening US underwent curable resection; the only case that was missed could not undergo surgery, because RCC presented with a bone metastasis 3 months later.
Haliloglu et al. [24] retrospectively reviewed the reports of 18.686 consecutive urinary US examinations of 18 203 patients were evaluated. 35 of the remaining 74 patients were diagnosed as angiomyolipoma by US, and confirmed by CT. Three renal masses that could not be classified by US were proved to be benign with other imaging techniques.
Thirty-six of the 74 patients with preoperative diagnosis of RCC and in one of them two pulmonary nodules were detected. After undergoing surgery, the renal masses underwent histopathological examination. Only the Fuhrman grading system of the RCC was reported in the study: four patients (11.2%) were classified as grade I, 19 patients (52.7%) were grade II, and 13 patients (36.1%) were grade III; no grade IV were reported.
Tsuboi et al. [25] analyzed 60,604 subjects undergoing a general health checkup employing US.
Of these, 97 were diagnosed as having a renal tumor or suspected renal tumor by transabdominal US screening and underwent re-examination by US or CT scan. Twenty-four patients (4 men and 20 women) were diagnosed as having AML, with a fatty component detected within the mass by plain CT, and two patients as having renal calcification. Contrast CT enabled diagnosis of a renal cyst in two patients and a renal tumor in 14 patients (nine men and five women). All 14 patients diagnosed as having RCC except one underwent nephrectomy, which gave pathologic evidence supporting the diagnosis of RCC. The remaining one patient refused to undergo the operation and was then followed up at regular intervals. No pathological report was shown in the study.
Filipas et al. [26] reported the results form a screening program of 9959 volunteers participated in the screening program in the first year and of these participants, 79% returned for re-examination in the second year. Thirteen (0.1%) subjects were found to have a renal mass, of which nine were RCC, one was leiomyoma, one a oncocytoma, and two were followed by imaging without undergoing surgery. RCC stage was reported: one T1N0M0, five T2N0M0, one pT3bN0M0, and two M1 (T3bN1 and T3bN2).
Mitchell et al. [27]m reported in a single-center study a population of 11,932 healthy asymptomatic subjects undergoing electron beam CT scan and a diagnosis of solid renal tumor was made for 26 patients and underwent resection of the renal mass. Overall, Nineteen renal cell carcinomas, three oncocytomas, two angiomyolipomas (AML), and one cystic nephroma were identified. Of the 22 classifiable tumors, 20 were T1N0M0, 1 was T2N0M0, and 1 was T3aN0M0. One patient was found to have adrenal hemorrhage and thrombosis without renal pathology. One patient died of surgical complications. Twenty-five patients are clinically well and without evidence of recurrent disease at 1–41 months (mean 17 months) postoperatively.
Feldstein et al. [28] reported 32,310 healthy subjected undergoing an executive health program employing both US and CT scan. 18 RCCs were detected and of these, 13 (72%) were detected by the screening program and five (28%) were missed. Of the detected RCC, 12 were T1N0M0 and 1 was T2N0M0; of the undetected RCC, one T1N0M0, one T2N0M0, one T3aN0M0, and two were M1 (T1Nx and T2N0).
Overall, the prevalence of renal masses/RCC diagnosed by imaging among the screened individuals ranged between 0.02% and 0.22% across the included studies (Table 1); of note, the prevalence of disease was inherently associated with the socio-demographic characteristics of the subjects included in the screening programs.
Cost-analysis of RCC screening programs
A detailed overview of the results of the four studies assessing the costs of RCC screening programs is reported in Table 2.
Malaeb et al. [22] presented a limited cost analysis as not comprehensive of all expenses. Cost for US and CT with contrast medium were $107 and $337, respectively. However, they did not include several cost items, such as the radiologist’s fee, the office visits, loss of work and patient anxiety. At these rates the minimum cost of detecting one RCC was $32,480, which does not include additional studies derived from false-positive results requiring abdominal CT or MRI.
Mizuma et al. [23] reported a screening program comprehending 16,024 subjects undergoing US examinations; 762 patients underwent further diagnostic workup to detect 11 RCCs. Assuming a cost of $200 for US or subsequent testing, the expenditure was $3,357,200 for a total of 16,786 examinations and $305,200 for each screening-detected RCC.
Rossi et al. [12] conducted a study to determine whether current evidence suggests that screening is potentially cost-effective and, if so, in which age/gender groups. A decision model was developed evaluating screening in asymptomatic individuals in the UK, adopting a National Health Service perspective. The authors assessed the potential benefit and cost of a single focused renal US scan compared with standard of care (no screening). A comprehensive cost-analysis per gender and age groups was performed, proving that cost-effectiveness improves as the prevalence of RCC increases and the cost of US decreases. Overall, given a prevalence of RCC of 0.34% (0.18–0.54%), screening 60-year-old men resulted in an incremental cost-effectiveness ratio (ICER) of £18,092/quality-adjusted life years (QALY) (€22,843/QALY). Given a prevalence of RCC of 0.16% (0.08–0.25%), screening 60-year-old women resulted in an ICER of £37 327/ QALY (€47 129/QALY). In the male population, the authors reported a RCC prevalence of 0.14%, 0.23%, and 0.34% for patients > 40, > 50, and > 60 years, respectively, with an incremental cost for the health system of £47.06, £45.69, and £44.55, respectively. Similarly, but reflecting the lower prevalence, in the female population they reported a RCC prevalence of 0.07%, 0.09%, and 0.16% for patients > 40, > 50, and > 60 years, respectively, with an incremental cost of £47.61, £46.99, and £46.56. The authors concluded that current evidence suggests that one-off screening of 60-year-old men is potentially cost-effective and that further research into this topic would be of value to society.
Finally, Filipas et al. [26] evaluated cost-effectiveness as a critical issue for evaluating any screening program. They evaluated renal US as widely available and low cost (US $6 per investigation) favoring its use as a potential screening tool for RCC. However, the study stated that the low incidence of RCC compared with other screened cancers raises doubts about the economic benefit of screening a population of ≥ 40 years. In addition, no comprehensive evaluation has been performed as many expenses have not been investigated (i.e., cost of treatment of metastatic RCC and the prevalence of incurable disease).
Current clinical trials on RCC screening
Only one clinical trial on RCC screening is currently ongoing (Yorkshire Kidney Screening Trial [YKST); NCT05005195), sponsored by the University of Leeds in U.K. This is a non-randomized open label feasibility study for a RCC screening program in patients enrolled in the Yorkshire Lung Screening Trial that offers subjects at high risk for lung cancer aged 55–80 a CT scan as part of a lung health check. The study started on May 10th, 2021 and the estimated tudy completion date is February 28th, 2023. To perform a correct RCC screening, additional low-dose abdominal CT scan slices are performed to achieve a correct visualization of the kidney. Primary Outcome Measures include: the proportion of individuals who take up the offer of an abdominal CT scan; the acceptability of the combined lung and RCC screening approach to participants by non-contrast CT scanning; the acceptability of the combined lung and RCC screening approach to healthcare professionals; and the additional time required for the combined screening approach, including the time to provide information, consent participants, and perform the lengthier CT scan, the time needed by radiologists for reporting the CT scans, and the additional time to review abdominal CT findings. Secondary outcomes include the proportion of participants found to have an RCC to provide an estimate of the prevalence of RCC at non-contrast CT screening in 55–80 year smokers and ex-smokers; the stage distribution of all RCCs identified; the proportion of participants found to have incidental renal findings (cysts, anatomical variants) on non-contrast CT scanning; and the proportion of participants with non-renal findings (i.e., abdominal aortic aneurysms, pancreatic and liver lesions on non-contrast CT scanning).
Discussion
As no premalignant conditions can be identified and treated in a timely fashion before development of RCC, the aim of a RCC screening program is still to reduce deaths by the identification of tumors at an early and treatable stage [15]. In this systematic review we provided an updated summary on the available evidence on the currently available screening programs for RCC, focusing on their potential clinical impact and cost-effectiveness.
After decades of research on screening for RCC, a number of studies and clinical trials are now attempting to redesign the concept of RCC early detection [15]. The rationale behind a screening program for RCC is clear, given the high cancer-specific mortality, the increase prevalence of established RCC risk factors in the general population and the adverse consequences of late diagnosis and treatment at more advanced stages [29]. Notably, there is an increasing interest within the international Urology Community in evaluating the optimal strategy for earlier diagnosis of this ‘silent’ cancer, which is largely curable if identified at an early stage; this priority has also been recognized by patients with kidney cancer, caregivers and expert clinicians [30, 31]. In fact, the epidemiologic signature of the disease (i.e., increasing incidence, high proportion of asymptomatic individuals at diagnosis and high mortality rate) allows RCC to fulfil many of the Wilson and Jungner criteria for suitability for screening [32], although a number of key uncertainties still remain and require further research [15, 33]. In addition, while the “preclinical period” (defined as the time during which an individual has RCC but has not yet received a diagnosis) and consequently the time during which a screening program could be effective is estimated to be between 3.7 and 5.8 years in an asymptomatic screening population, whether detecting RCC during the preclinical period is ultimately beneficial is still controversial [2, 15].
The prevalence of asymptomatic RCC in previous studies including subjects receiving CT screening for coronary artery disease, lung cancer, colon cancer or as self-referred screenees ranged from 0.11 to 0.76% (pooled prevalence of 0.21%; 95% CI, 0.14–0.28%) [34]. Interestingly, the prevalence of renal masses and RCC detected in studies from Western Countries (Europe and North America) are more than double those in studies from Asia (0.17% versus 0.06%, respectively) [35]. These finding not only highlight a non-negligible variability in the estimates of RCC prevalence in asymptomatic individuals across Countries, but also underline that the concept of screening for “(small) renal masses” (of undetermined nature) does not necessarily equal the concept of screening for histologically defined RCC. To provide an overview of the available studies addressing the clinical utility of RCC screening programs, in this work we explicitly excluded from the analysis studies reporting on screening programs for “renal masses” without histopathological confirmation of RCC nature.
The ideal screening modality for RCC is yet to be elucidated. A recent systematic review on liquid biomarkers and innovative imaging modalities for RCC diagnosis found that none of the proposed tests were ready for prime time; as such, despite the promising role of miRNAs, metabolites and CT- or MRI-based radiomics features coupled with machine-learning algorithms, the current evidence appears premature to recommend integration of noninvasive diagnostic modalities in routine clinical practice [14]. For a standalone RCC screening program, US of the kidney has been proposed as an effective option. Our review found that the most commonly investigated screening modalities were indeed focused renal US followed by CT scan. US holds the advantages of being a widely available modality all over the world, to be highly cost-effective, and to be non-invasive in terms of radiations; nonetheless, its limitations is mostly linked to the operator-dependency of the technique (that can be performed by radiologists or urologists depending on several logistical issues within organizations and Countries) as well as to the variety of patient-related factors potentially impacting on US quality (such as obesity). Ultrasound RCC detection rates also depend on the size of renal lesions: while it enables the detection of 85–100% tumors > 3 cm in size, only 67–82% of tumors 2–3 cm in size can be diagnosed [36, 37]. Therefore, ultrasound screening for RCC has the potential to lead to false-negative results in masses < 3 cm in size. Finally, detection of a (small) renal mass at renal US does not necessarily mean detection of RCC, due to the non-negligible rate of benign renal masses in such patient populations [38]. On the contrary, abdominal contrastenhanced CT is still the goldstandard method of detecting a renal mass. CT scan yields the advantage of being objective and more precise in depicting abdominal organs; at the same time, despite the high sensibility and specificity, CT scan leads to higher costs, invasiveness, and risk of adverse events. As such, CT might not be appropriate for national screening due to several caveats, including the relatively low prevalence of renal masses in the general population, the high cost, and potential risks [15]. Yet, combining RCC CT scanning with other CTscanbased health check programs might be an option to increase the value and cost-effectiveness of such screening programs; this concept is indeed currently being explored in the Yorkshire Kidney Screening Trial (NCT05005195). There are a few studies exploring RCC screening in conjunction with other screening programs, such as abdominal aortic aneurism [22] or lung cancer [39], with the aim to decrease costs, invasiveness and to increase the diagnosis of a pathological finding, since these diseases have a low prevalence in the healthy population.
In our review, the overall prevalence of renal masses/RCC diagnosed by imaging ranged between 0.02 and 0.22% across the included studies (Table 1). It is important to highlight that while the incidence of RCC increases with age, screening elderly individuals with potentially higher competing risks of death might not be beneficial. A recently published analysis of US showed that screening men aged 50–60 years was the most costeffective approach [12]. Costeffectiveness modelling is also highly sensitive to the prevalence of RCC (Table 2) [12]: targeted screening of higher risk individuals, selected from the general population by means of established risk-stratification tools [40] is likely to be the most costeffective strategy [41]. Any RCC screening program should indeed also aim to minimize potential harms to individual subjects and to the whole society, including worsening of quality of life, emotional distress, and incidental overdiagnosis (and overtreatment) of benign or slowly growing indolent renal masses; to achieve this goal, refinement of current decision-making schemes for patients with localized renal masses (including the role of renal tumor biopsy) are urgently warranted [42]. Screening programs for RCC will be effective only if subjects are willing to undergo screening. In this regard, in a recent online population‐based survey aiming to explore attitudes towards kidney cancer screening and factors influencing intention to attend a future screening programs, most participants were ‘very likely’ or ‘likely’ to undergo screening tests for RCC using urine-, blood-, US- or low‐dose CT-based tests, both within a RCC-specific program and in conjunction with lung cancer screening [43]. These findings support the ongoing research into RCC screening tests [15]: based on the available evidence, specific combinations of serum or urinary miRNAs, as well as other biomarkers, such as serum (or, less frequently, urinary) proteins, enzymes, metabolites, GAGs, and cell-free DNA, appear promising for discrimination between healthy controls and patients with histologically confirmed RCC. One clinical trial (NCT02923284) evaluated two biomarkers (urinary AQP1 and PLIN2) as a low-cost screening method to discriminate benign renal masses and patients with RCC from healthy controls [14]. Further research is needed to validate these biomarkers as efficient and cost-effective screening tools at a population-level and in clinical practice.
Our systematic review is not devoid of limitations. First, despite a rigorous review process and a well-defined PICO framework, our search strategy might have not retrieved all potentially relevant articles on RCC screening. Moreover, we limited our search to the English-language literature. Of note, we could not analyze the differential impact of available screening programs on the detection of indeterminate renal masses versus pathologically confirmed RCC, mainly due to limitations in the design of available studies. For the same reason, we could not analyze in detail the cost-effectiveness of all available RCC screening programs, nor perform a formal quantitative analysis from the studies included in the review.
Conclusions
Despite an increasing interest from patients and clinicians during the last decades, our systematic review found a relative lack of studies reporting the efficacy and cost-effectiveness of well-structured screening programs for RCC. There is no high-quality evidence to show that screening asymptomatic individuals by any biomarker- or imaging-based test would reduce RCC morbidity and/or mortality. Moreover, the optimal modality for RCC screening is still controversial. Targeting high-risk individuals and/or combining detection of RCC with other health checks such as lung cancer screening represent pragmatic options to improve the cost-effectiveness and reduce the potential harms of RCC screening. While waiting the results of prospective clinical trials, further research is needed to develop and validate accurate risk prediction models for RCC, define the most cost-effective screening population, explore the acceptability of a screening program in the population, and assess whether RCC screening might lead to a survival benefit without further increasing overdiagnosis and overtreatment of localized renal masses.
Change history
20 July 2022
Missing Open Access funding information has been added in the Funding Note
References
International Agency for Research on Cancer (World Health Organization) (2020) Kidney: Globocan 2020—the global cancer observatory. Globocan 2020. 419:1–2. https://gco.iarc.fr/today/data/factsheets/cancers/29-Kidney-fact-sheet.pdf
Rossi SH, Klatte T, Usher-Smith J, Stewart GD (2018) Epidemiology and screening for renal cancer. World J Urol 36(9):1341–1353. https://doi.org/10.1007/s00345-018-2286-7
Hock LM, Lynch J, Balaji KC (2002) Increasing incidence of all stages of kidney cancer in the last 2 decades in the united states: an analysis of surveillance, epidemiology and end results program data. J Urol 167(1):57–60. https://doi.org/10.1016/S0022-5347(05)65382-7
Lightfoot N, Conlon M, Kreiger N, Bissett R, Desai M, Warde P, Prichard HM (2000) Impact of noninvasive imaging on increased incidental detection of renal cell carcinoma. Eur Urol 37(5):521–527. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed8&NEWS=N&AN=30189819
Znaor A, Lortet-Tieulent J, Laversanne M, Jemal A, Bray F (2015) International variations and trends in renal cell carcinoma incidence and mortality. Eur Urol 67(3):519–530. https://doi.org/10.1016/j.eururo.2014.10.002
Welch HG, Kramer BSBW (2020) Epidemiologic signatures in cancer. N Engl J Med 382(1):95–98. https://doi.org/10.1056/nejmc1914747
Selby PJ, Banks RE, Gregory W et al (2018) Methods for the evaluation of biomarkers in patients with kidney and liver diseases: multicentre research programme including ELUCIDATE RCT. Program Grants Appl Res 6(3):1–528. https://doi.org/10.3310/pgfar06030
Office for National Statistics (2019) Office for National Statistics, Cancer survival by stage at diagnosis for England (2013–2017). https://www.ons.gov.uk/
Capitanio U, Bensalah K, Bex A et al (2019) Epidemiology of renal cell carcinoma. Eur Urol 75(1):74–84. https://doi.org/10.1016/j.eururo.2018.08.036
Foreman KJ, Marquez N, Dolgert A et al (2018) Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet 392(10159):2052–2090. https://doi.org/10.1016/S0140-6736(18)31694-5
Reitblat C, Bain PA, Porter ME et al (2021) Value-based healthcare in urology: a collaborative review. Eur Urol 79(5):571–585. https://doi.org/10.1016/j.eururo.2020.12.008
Rossi SH, Klatte T, Usher-Smith JA et al (2021) A decision analysis evaluating screening for kidney cancer using focused renal ultrasound. Eur Urol Focus 7(2):407–419. https://doi.org/10.1016/j.euf.2019.09.002
Diaz-de-Leon A, Pedrosa I (2017) Imaging and screening of kidney cancer. Radiol Clin North Am 55(6):1235–1250. https://doi.org/10.1016/j.rcl.2017.06.007
Campi R, Stewart GD, Staehler M et al (2021) Novel liquid biomarkers and innovative imaging for kidney cancer diagnosis: what can be implemented in our practice today? A systematic review of the literature. Eur Urol Oncol 4(1):22–41. https://doi.org/10.1016/j.euo.2020.12.011
Usher-Smith J, Simmons RK, Rossi SH, Stewart GD (2020) Current evidence on screening for renal cancer. Nat Rev Urol 17(11):637–642. https://doi.org/10.1038/s41585-020-0363-3
Knoll T, Omar MI, Maclennan S et al (2018) Key Steps in conducting systematic reviews for underpinning clinical practice guidelines: methodology of the European Association of Urology. Eur Urol 73(2):290–300. https://doi.org/10.1016/j.eururo.2017.08.016
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021:372. https://doi.org/10.1136/bmj.n71
Moher D, Shamseer L, Clarke M et al (2016) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Rev Esp Nutr Humana y Diet 20(2):148–160. https://doi.org/10.1186/2046-4053-4-1
Shamseer L, Moher D, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: elaboration and explanation. BMJ 349:g7647. http://www.bmj.com/content/bmj/349/bmj.g7647.full.pdf%0Ahttp://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emex&NEWS=N&AN=601176689
Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C (2013) Assessing bias in studies of prognostic factors. Ann Intern Med 158(4):280–286. https://doi.org/10.7326/0003-4819-158-4-201302190-00009
Ono K, Ochiat R, Yoshida T, Kitagawa M (2007) The detection rates and tumor clinical/pathological stages of whole-body FDG-PET cancer screening. Ann Nucl Med 21(1):65–72
Malaeb BS, Martin DJ, Littooy FN et al (2005) The utility of screening renal ultrasonography: identifying renal cell carcinoma in an elderly asymptomatic population. BJU 2005:977–981. https://doi.org/10.1111/j.1464-410X.2005.05451.x
Mizuma Y, Watanabe Y, Ozasa K (2002) Validity of sonographic screening for the detection of abdominal cancers. J Clin Ultrasound 30(7):408–415
Hakan A, Omer H (2011) Urinary ultrasonography in screening incidental renal cell carcinoma: is it obligatory ? Int Urol Nephrol 2011:687–690. https://doi.org/10.1007/s11255-010-9843-3
Tsuboi N, Horiuchi K, Kimura GO et al (2000) Renal masses detected by general health checkup. Int J Urol 7(11):404–408
Filipas D, Spix C, Hohenfellner R (2003) Screening for renal cell carcinoma using ultrasonography : a feasibility. BJU Int 91:595–599. https://doi.org/10.1046/j.1464-410X.2003.04175.x
Mitchell TL, Pippin JJ, Devers SM et al (2000) Incidental detection of preclinical renal tumors with electron beam computed tomography : report of 26 consecutive operated patients. J Comput Assist Tomogr 24(6):843–845
Feldstein MS, Rhodes DJ, Parker AS, Orford RR, Castle EP (2009) The haphazard approach to the early detection contemporary executive health programme. BJT Int. https://doi.org/10.1111/j.1464-410X.2008.08315.x
Ljungberg B, Bensalah K, Canfield S et al (2019) Renal Cell carcinoma EAU guidelines on renal cell carcinoma: 2019. Eur Urol. https://doi.org/10.1016/j.eururo.2015.01.005
Rossi SH, Fielding A, Blick C, Handforth C, Brown JE, Stewart GD (2019) Setting research priorities in partnership with patients to provide patient-centred urological cancer care. Eur Urol 75(6):891–893. https://doi.org/10.1016/j.eururo.2019.03.008
Rossi SH, Blick C, Handforth C, Brown JE, Stewart GD (2020) Essential research priorities in renal cancer: a modified delphi consensus statement. Eur Urol Focus 6(5):991–998. https://doi.org/10.1016/j.euf.2019.01.014
Wilson JM, Jungner YG (1968) Principles and practice of mass screening for disease. Bol Oficina Sanit Panam 65(4):281–393. http://www.ncbi.nlm.nih.gov/pubmed/4234760.
Rossi SH, Klatte T, Usher J, Grant S (2018) Epidemiology and screening for renal cancer. World J Urol 36(9):1341–1353. https://doi.org/10.1007/s00345-018-2286-7
Fenton JJ, Weiss NS (2004) Screening computed tomography: will it result in overdiagnosis of renal carcinoma? Cancer 100(5):986–990. https://doi.org/10.1002/cncr.20055
Rossi SH, Hsu R, Blick C et al (2017) Meta-analysis of the prevalence of renal cancer detected by abdominal ultrasonography. Br J Surg 104(6):648–659. https://doi.org/10.1002/bjs.10523
Warshauer DM, McCarthy SM, Street L et al (1988) Detection of renal masses: Sensitivities and specificities of excretory urography/linear tomography, US, and CT. Radiology 169(2):363–365. https://doi.org/10.1148/radiology.169.2.3051112
Jamis-dow CA, Jennings B (1996) Radiology CT versus masses: and detection. Genitourin Radiol 198:785–788
Kim JH, Li S, Khandwala Y, Chung KJ, Park HK, Chung BI (2019) Association of prevalence of benign pathologic findings after partial nephrectomy with preoperative imaging patterns in the United States from 2007 to 2014. JAMA Surg 154(3):225–231. https://doi.org/10.1001/jamasurg.2018.4602
Swensen SJ, Jett JR, Sloan JA et al (2002) Screening for lung cancer with low-dose spiral computed tomography. Am J Respir Crit Care Med 165:508–513. https://doi.org/10.1164/rccm.2107006
Harrison H, Thompson RE, Lin Z et al (2021) Risk prediction models for kidney cancer: a systematic review. Eur Urol Focus 7(6):1380–1390. https://doi.org/10.1016/j.euf.2020.06.024
Lotan Y, Karam JA, Shariat SF, Gupta A, Roupret M, Bensalah K, Margulis V (2016) Renal-cell carcinoma risk estimates based on participants in the prostate, lung, colorectal, and ovarian cancer screening trial and national lung screening trial. Urol Oncol Semin Orig Investig 34(4):167. http://www.elsevier.com/locate/issn/10781439%5Cn, http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed18a&NEWS=N&AN=606964836
Chandrasekar T, Boorjian SA, Capitanio U, Gershman B, Mir MC, Kutikov A (2021) Collaborative review: factors influencing treatment decisions for patients with a localized solid renal mass[formula presented]. Eur Urol 80(5):575–588. https://doi.org/10.1016/j.eururo.2021.01.021
Harvey-Kelly LLW, Harrison H, Rossi SH, Griffin SJ, Stewart GD, Usher-Smith JA (2020) Public attitudes towards screening for kidney cancer: an online survey. BMC Urol 20:1. https://doi.org/10.1186/s12894-020-00724-0
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Consortia
Contributions
PD: data extraction; risk of bias assessment; manuscript writing. TK: writing of the systematic review protocol; manuscript editing. DA: title/abstract screening; manuscript editing. RB: title/abstract screening; manuscript editing. UC: manuscript editing. SE: manuscript editing. AI: full text screening; manuscript editing. OK: manuscript editing. LM: full text screening; manuscript editing. MM: manuscript editing. SM: manuscript editing. NP: manuscript editing. AP: manuscript editing. AP: risk of bias assessment; manuscript editing. ER: full text screening; manuscript editing. RC: project concept and design; data extraction; manuscript writing; manuscript editing.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Research involving human participants
The study did not involve human participants.
Informed consent
No individual participants were included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Diana, P., Klatte, T., Amparore, D. et al. Screening programs for renal cell carcinoma: a systematic review by the EAU young academic urologists renal cancer working group. World J Urol 41, 929–940 (2023). https://doi.org/10.1007/s00345-022-03993-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-03993-6