Abstract
Purpose
We assessed the prognostic value of systemic immune-inflammation index (SII) to refine risk stratification of the heterogeneous spectrum of patients with non-muscle-invasive bladder cancer (NMIBC)
Methods
In this multi-institutional cohort, preoperative blood-based SII was retrospectively assessed in 1117 patients with NMIBC who underwent transurethral resection of bladder (TURB) between 1996 and 2007. The optimal cut-off value of SII was determined as 580 using the best Youden index. Cox regression analyses were performed. The concordance index (C-index) and decision curve analysis (DCA) were used to assess the discrimination of the predictive models.
Results
Overall, 309 (28%) patients had high SII. On multivariable analyses, high SII was significantly associated with worse PFS (hazard ratio [HR] 1.84; 95% confidence interval [CI] 1.23–2.77; P = 0.003) and CSS (HR 2.53; 95% CI 1.42–4.48; P = 0.001). Subgroup analyses, according to the European Association of Urology guidelines, demonstrated the main prognostic impact of high SII, with regards to PFS (HR 3.39; 95%CI 1.57–7.31; P = 0.002) and CSS (HR 4.93; 95% CI 1.70–14.3; P = 0.005), in patients with intermediate-risk group; addition of SII to the standard predictive model improved its discrimination ability both on C-index (6% and 12%, respectively) and DCA. In exploratory intergroup analyses of patients with intermediate-risk, the improved discrimination ability was retained the prediction of PFS and CSS.
Conclusion
Preoperative SII seems to identify NMIBC patients who have a worse disease and prognosis. Such easily available and cheap standard biomarkers may help refine the decision-making process regarding adjuvant treatment in patients with intermediate-risk NMIBC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The standard treatment for non-muscle-invasive bladder cancer (NMIBC) is transurethral resection of bladder (TURB) followed by intravesical instillation chemotherapy or immunotherapy, according to individual patient risk for disease recurrence and progression [1]. Despite complete resection and adjuvant intravesical instillation therapy, approximately 70% of these patients experience disease recurrence and 30%, eventually, experience progression [2, 3]. Several prognostic models and biomarkers have been investigated as predictors of oncologic outcomes to guide clinical decision-making and patient counselling [4, 5]. However, none of them have achieved sufficient accuracy to be integrated into daily routine clinical practice [1, 2, 6,7,8].
The immune system, including the inflammatory response and the tumor microenvironment, plays an important role in the clinical and biological behavior and outcomes of bladder cancer (BC) [9]. The systemic immune-inflammation index (SII), an immune and inflammatory index based on neutrophil, lymphocyte, and platelet counts, has been shown to be associated with oncological outcomes in several types of cancer [10, 11].
While SII has already been reported to be of prognostic value in MIBC and high-risk NMIBC patients, its role in NMIBC patients with intermediate-risk remains unclear [12, 13]. Given BC, which is an inflammatory disease, has efficiently been treated using bacillus Calmette–Guerin (BCG), an agent that is known to trigger a good strong inflammatory and immunologic response. We hypothesized that the simple easily available SII can help classify NMIBC patients according to their individualized risk of recurrence and progression, especially in patients with intermediate-risk [14]. Toward this aim, we explored the prognostic significance of preoperative SII in a large multi-institutional cohort of NMIBC patients.
Materials and methods
Patient selection
Our study included 1117 consecutive patients treated with TURB for primary or recurrent NMIBC with or without adjuvant intravesical instillation therapy at four academic centers in US and Europe between 1996 and 2007 [7]. All patients were histologically confirmed to have urothelial carcinoma with only minor (less than 10%) involvement of variant components, if any. None of the patients had metastatic disease, concurrent upper tract urothelial or urethral cancer invasion at the time of TURB. This study obtained institutional review board approval at each participating institution. All sites agreed to institutional data sharing prior to study initiation.
Data collection and pathologic evaluation
Pretreatment blood-based SII values were assessed within the 30 days prior to TURB. SII was calculated as platelet count × neutrophil/lymphocyte count. SII and demographic, pathologic, and survival outcomes data were collected and entered into a computerized database. The optimal SII cut-off value was defined by creating a time-dependent receiver operating characteristic (ROC) curve to yield the highest Youden index value. Using this score the overall population was divided into two separate SII groups (> 580 vs. ≤ 580). The specimens were reviewed at the beginning of the study at each center by expert genitourinary pathologists. They were blinded to the previous history of the patient and to the clinical development after specimen acquisition. The pathologic stage was reassigned using the 2010 American Joint Committee on Cancer TNM staging system and tumor grade according to the 1973 World Health Organization (WHO) grading system. Patients were categorized into low, intermediate, and high (added highest only for progression risk classification) risk groups for the prediction of disease progression and recurrence according to the European Association of Urology (EAU) guidelines and European Organization for Research and Treatment of Cancer risk tables (EORTC) [1, 15, 16].
Management and follow-up
All patients underwent complete TURB. A second-look resection was performed 2–6 weeks after initial treatment based on the pathologic and intraoperative findings according to the guidelines at the time. In general, a second look was indicated in cases of incomplete initial TURB or doubt about the completeness of a TURB; if there was no muscle in the specimen after initial resection, with the exception of Ta LG/G1 tumors and primary CIS; in T1 tumors. Immediate single-dose postoperative instillation chemotherapy, adjuvant intravesical chemotherapy, or adjuvant BCG immunotherapy were administered according to risk categories of disease recurrence and progression based on current guidelines.
All patients were generally followed up according to the EAU guidelines. This included urinary cytology and a cystoscopy every 3 months for the first 2 years after surgery; after that, every 6 months for 3 years, and then, annually. Disease recurrence was defined as the first tumor relapse in the bladder regardless of tumor stage. Disease progression was defined as tumor relapse in the bladder with tumor stage T2 or higher. Disease occurrence in the upper urinary tract was considered as a second primary.
Statistical analysis
Associations of SII with categorical variables were assessed using chi-squared tests and differences in continuous variables were analyzed using Mann–Whitney U tests. Recurrence-free (RFS), progression-free (PFS), cancer-specific (CSS), and overall (OS) survival were graphically visualized using the Kaplan–Meier method. Differences between groups were assessed with the log-rank test. Multivariable Cox regression models were used to investigate the associations of SII with each survival outcome. The discrimination of the model was evaluated using the Harrel’s concordance index (C-index). The additional clinical net-benefit of SII was evaluated using decision curve analysis (DCA). In addition to subgroup analyses based on patients with intermediate-risk, we performed exploratory analyses of patients with intermediate-risk based on the risk stratification proposed by the International Bladder Consultation Group (IBCG) [17, 18]. In these analyses, we excluded patients who received intravesical BCG therapy due to the changes of treatment strategies depending on the previous BCG therapy. All P values were two-sided, and statistical significance was defined as P < 0.05. Statistical analyses were performed using R version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria) and Stata/MP 14.2 statistical software (Stata Corp., College Station, TX, USA).
Results
Of the 1117 patients included in this study, 309 (28%) were categorized into the high SII (SII > 580) group and 808 (72%) into the low (SII ≤ 580). Patients with low-, intermediate-, high-, and very high-risk disease were 18%, 37%, 41%, and 4%, respectively. The associations of SII with standard clinicopathologic characteristics are shown in Table 1. There was no significant difference between groups, apart from sex (P = 0.048).
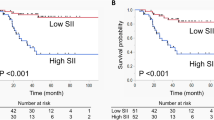
Association with survival outcomes in the entire cohort
During the median follow-up of 64 months (IQR 26–110 months), 470 (42.1%) patients experienced disease recurrence, 103 (9.2%) experienced disease progression, and 299 (27%) died from any causes, and 50 (4.5%) died from BC. In Kaplan–Meier analyses, patients with high SII were at significantly increased risk of worse PFS and CSS (hazard ratio [HR] 1.75; 95% confidence interval [CI] 1.17–2.60; P = 0.005, and HR 2.32; 95% CI 1.33–4.05; P = 0.002, respectively), but not RFS and OS (HR 1.21; 95% CI 0.99–1.47; P = 0.06, and HR 0.95; 95% CI 0.73–1.23; P = 0.70, respectively) (Supplementary Fig. 1). On multivariable Cox regression analyses that adjusted for the effects of established confounders, pre-TURB SII remained associated with both PFS and CSS (HR 1.84; 95% CI 1.23–2.77; P = 0.003, and HR 2.53; 95% CI 1.42–4.48; P = 0.001, respectively) (Table 2).
Subgroup analyses in patients with intermediate-risk NMIBC
In patients with intermediate-risk NMIBC, high SII was significantly associated with an increased probability of worse PFS, and CSS (HR 3.39; 95% CI 1.57–7.31; P = 0.002, and HR 4.93; 95% CI 1.70–14.3; P = 0.005, respectively), but not with RFS and OS (HR 1.40; 95% CI 1.00–1.96; P = 0.05, and HR 1.21; 95% CI 0.79–1.84; P = 0.38) (Table 3). Addition of pre-TURB SII levels to a basic model based on age, sex, tumor size, multifocality, tumor grade, and tumor stage increased the discriminatory ability for the prediction of both PFS (change of C-index 6%) and CSS (change of C-index 12%). DCA showed that adding SII to a standard model increased the net benefit for the prediction of PFS and CSS (Supplementary Fig. 2).
In exploratory analyses for intermediate-risk patients with 1–2 factor determined according to the algorithm proposed by IBCG, high SII was significantly associated with worse PFS and CSS (HR 3.71; 95% CI 1.62–8.51; P = 0.002, HR 5.15; 95% CI 1.72–16.9; P = 0.005, respectively) (Supplementary Table 1).
Discussion
In this large multi-institutional study, we investigated the clinical value of the preoperative blood-based SII for patients with primary or recurrent NMIBC treated with TURB. We found that high SII was an independent predictive factor for PFS and CSS, but not for OS in NMIBC. Subgroup analyses demonstrated that in intermediate-risk patients, high SII was a significant predictor of PFS, and CSS; furthermore, for patients with 1–2 factors substantified by the IBCG algorithm, high SII remained also an independent predictor of PFS and CSS. These findings suggest that SII would help refine our clinical practice by helping identify individualized treatment strategies in the large cohort of heterogeneous patients with intermediate-risk BC.
Inflammatory conditions induced by mediators such as chemokines or cytokines extrinsically aid proliferation and survival of malignant cells, angiogenesis, and metastasis; while the activation of oncogene drives intrinsic inflammatory pathways. Thus, inflammation and cancer are strongly linked, and inflammation can create the nurturing environment for cancer formation and promotion [14, 19]. To date, the wide spectrum of biological behavior in NMIBC, especially in intermediate-risk disease, has encouraged researchers to explore several tissue- and blood-based biomarkers [20]. Of these, the prognostic values of blood-based biomarkers measuring systemic inflammatory responses have been investigated in various malignancies, driven by advantages in availability and cost. Recently, SII, determined by multiplying NLR by platelet count demonstrated promising discriminatory power for cancer progression with several functional mechanisms having been proposed. Neutrophils, a hallmark of inflammation, interact with circulating tumor cells (CTCs) facilitating binding to the endothelium. This interaction can promote tumor progression and metastasis by inducing tumor cell proliferation, stimulating angiogenesis, and suppressing the function of the adaptive immune response in the tumor microenvironment [21, 22]. Impairment of immune cells triggered by the evolving tumor microenvironment can be detected in cancer patients [23]. Aggregated active platelets envelop around CTCs (present in 18–20% of patients with NMIBC and associated with inferior oncologic outcomes), shielding CTCs from immunological attacks in high-risk NMIBC (especially pT1 G3 disease) [24, 25]. Taken together, SII objectively reflects a combination of the inflammatory and host immune system status.
In our study, we confirmed the significant prognostic value of SII in NMIBC, regardless of the risk category. These findings suggest that low SII level may help identify patients who could benefit from meticulous surveillance instead of additional treatments which are often associated with adverse effects (e.g., maintenance therapy following induction intravesical BCG or chemotherapy).
Moreover, subgroup analyses revealed that in intermediate-risk NMIBC patients who did not receive BCG therapy, addition of SII to a basic model improved the discrimination power for the prediction of PFS (6%) and CSS (12%), along with the improved net benefit within the clinical reasonable range of thresholds in the DCA. Additionally, the impact of SII in this group was greater than that in the overall analyses (nearly five-times higher risk for CSS and more than three-times higher risk for PFS). Although the definition of intermediate-risk was different from this study, we and others have previously highlighted the heterogeneity of the intermediate-risk NMIBC group [17, 18]. Previous studies suggested that BCG therapy with maintenance was superior to BCG induction only or chemotherapy induction with maintenance for preventing recurrence or progression in patients with intermediate-risk NMIBC [26, 27]. However, given the heterogeneity of this population, variety of available options, and adverse effects of BCG, urologists have often been unsure about the type, schedule, and length of adjuvant therapy, resulting in low compliance with NMIBC guidelines [28]. Our findings suggest that pre-therapy SII would help guide individual treatment strategies of patients with intermediate-risk NMIBC, leading to improved outcomes and compliance with guidelines.
Moreover, due to concerns regarding the large heterogeneity in the risk of recurrence and progression in NMIBC patients with intermediate-risk, the IBCG proposed an intergroup subclassification in patients with intermediate-risk disease. However, for patients with 1–2 factors according to the IBCG algorithm, urologists still have a choice of regimen in adjuvant therapy. We confirmed that for patients with 1–2 factors, SII remained an independent factor for the prediction of both PFS and CSS with considerable increases in C-index (7% and 12%, respectively). Thus, pre-TURB SII can help guide decision of treatment regimen in intermediate-risk NMIBC patients with 1–2 factors (for example, chemotherapy for patients with low SII, and BCG for those with high SII).
Several limitations of our study should be acknowledged. First, due to the retrospective and multi-institutional aspect, therapeutic strategies and pathologic indications varied among the institutions, which may have affected survival outcomes. Second, we did not capture comorbidities at the time of SII measurement, which are major confounding factors due to their strong effects on the value of each variable. Third, we lack data on prior intravesical therapy, radical cystectomy, and variant histology, which could have influenced the oncologic outcomes. Finally, SII was measured preoperatively and the lack of standardized cut-off points. As such, measuring the postoperative SII might have some additive prognostic value.
Conclusion
We found that high pre-therapy SII was an independent predictive factor for both PFS and CSS in patients with NMIBC; this impact was enhanced in patients with intermediate-risk. Due to the improvement to the discriminatory accuracy of the standard prognostic model, SII may help discern patients who are likely to benefit from adjuvant intravesical treatments from those who are unlikely to have an oncologic benefit while suffering from unnecessary adverse events. Since BC is an inflammatory disease, SII has tangible potential to improve NMIBC patient care, together with other biomarkers that capture host and tumor factors.
Availability of data and material
Yes.
References
Babjuk M et al (2019) European Association of Urology guidelines on non-muscle-invasive bladder cancer (TaT1 and Carcinoma In Situ)-2019 update. Eur Urol 76(5):639–657
Xylinas E et al (2013) Accuracy of the EORTC risk tables and of the CUETO scoring model to predict outcomes in non-muscle-invasive urothelial carcinoma of the bladder. Br J Cancer 109(6):1460–1466
Sylvester RJ et al (2006) Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 49(3):466–477
D’Andrea D et al (2018) Progressive tissue biomarker profiling in non-muscle-invasive bladder cancer. Expert Rev Anticancer Ther 18(7):695–703
Soria F et al (2018) Diagnostic, prognostic and surveillance urinary markers in nonmuscle invasive bladder cancer: any role in clinical practice? Curr Opin Urol 28(6):577–583
Shariat SF et al (2010) Combination of multiple molecular markers can improve prognostication in patients with locally advanced and lymph node positive bladder cancer. J Urol 183(1):68–75
Laukhtina E et al (2020) Association of De Ritis ratio with oncological outcomes in patients with non-muscle invasive bladder cancer (NMIBC). World J Urol. https://doi.org/10.1007/s00345-020-03384-9. Online ahead of print
Quhal F et al (2021) Prognostic value of albumin to globulin ratio in non-muscle-invasive bladder cancer. World J Urol. https://doi.org/10.1007/s00345-020-03586-1. Online ahead of print
Mbeutcha A et al (2016) Prognostic significance of markers of systemic inflammatory response in patients with non-muscle-invasive bladder cancer. Urol Oncol 34(11):483.e17-483.e24
Yang R et al (2018) Prognostic value of systemic immune-inflammation index in cancer: a meta-analysis. J Cancer 9(18):3295–3302
Zhong JH, Huang DH, Chen ZY (2017) Prognostic role of systemic immune-inflammation index in solid tumors: a systematic review and meta-analysis. Oncotarget 8(43):75381–75388
Akan S et al (2020) Can the systemic immune inflammation index be a predictor of BCG response in patients with high-risk non-muscle invasive bladder cancer? Int J Clin Pract 75(4):e13813
Bi H et al (2020) Predictive values of preoperative prognostic nutritional index and systemic immune-inflammation index for long-term survival in high-risk non-muscle-invasive bladder cancer patients: a single-centre retrospective study. Cancer Manag Res 12:9471–9483
Mantovani A et al (2008) Cancer-related inflammation. Nature 454(7203):436–444
Soukup V et al (2020) Risk stratification tools and prognostic models in non-muscle-invasive bladder cancer: a critical assessment from the European association of urology non-muscle-invasive bladder cancer guidelines panel. Eur Urol Focus 6(3):479–489
Sylvester RJ et al (2021) European Association of Urology (EAU) prognostic factor risk groups for non-muscle-invasive bladder cancer (NMIBC) incorporating the WHO 2004/2016 and WHO 1973 classification systems for grade: an update from the EAU NMIBC guidelines panel. Eur Urol 79(4):480–488
Kamat AM et al (2014) Defining and treating the spectrum of intermediate risk nonmuscle invasive bladder cancer. J Urol 192(2):305–315
Soria F et al (2020) Stratification of intermediate-risk non-muscle-invasive bladder cancer patients: implications for adjuvant therapies. Eur Urol Focus. https://doi.org/10.1016/j.euf.2020.05.004
Candido J, Hagemann T (2013) Cancer-related inflammation. J Clin Immunol 33(Suppl 1):S79-84
Soria F et al (2019) Molecular markers in bladder cancer. World J Urol 37(1):31–40
Mollinedo F (2019) Neutrophil degranulation, plasticity, and cancer metastasis. Trends Immunol 40(3):228–242
Giese MA, Hind LE, Huttenlocher A (2019) Neutrophil plasticity in the tumor microenvironment. Blood 133(20):2159–2167
Ménétrier-Caux C et al (2019) Lymphopenia in cancer patients and its effects on response to immunotherapy: an opportunity for combination with cytokines? J Immunother Cancer 7(1):85
Rink M et al (2019) The current role of circulating biomarkers in non-muscle invasive bladder cancer. Transl Androl Urol 8(1):61–75
van Es N et al (2014) Effects of cancer on platelets. Semin Oncol 41(3):311–318
Oddens J et al (2013) Final results of an EORTC-GU cancers group randomized study of maintenance bacillus Calmette-Guérin in intermediate- and high-risk Ta, T1 papillary carcinoma of the urinary bladder: one-third dose versus full dose and 1 year versus 3 years of maintenance. Eur Urol 63(3):462–472
Hinotsu S et al (2011) Maintenance therapy with bacillus Calmette-Guérin Connaught strain clearly prolongs recurrence-free survival following transurethral resection of bladder tumour for non-muscle-invasive bladder cancer. BJU Int 108(2):187–195
Mori K et al (2020) Low compliance to guidelines in nonmuscle-invasive bladder carcinoma: a systematic review. Urol Oncol 38(10):774–782
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Consortia
Contributions
SK: data analysis and manuscript writing; KM: manuscript editing; EL: manuscript editing; VMS: data analysis; BP: manuscript editing; FQ: manuscript editing; RSM: data analysis; HM: data analysis; NCG: manuscript editing; PR: manuscript editing; MM: manuscript editing; RM: manuscript editing; MA: manuscript editing; DD’A: data analysis; EC: manuscript editing; MH: manuscript editing; SE: project development; YN: project development; SFS: project development and manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
All authors state that they have no conflict of interest that might bias this work.
Ethical approval.
This study has been approved by the appropriate ethics committee.
Consent to participants
Yes.
Consent for publication
Yes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Katayama, S., Mori, K., Pradere, B. et al. Prognostic value of the systemic immune-inflammation index in non-muscle invasive bladder cancer. World J Urol 39, 4355–4361 (2021). https://doi.org/10.1007/s00345-021-03740-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-021-03740-3