Abstract
Purpose
To evaluate the trends in risk-group distribution and Pentafecta outcomes in patients treated with nerve-sparing (NS), robot-assisted radical prostatectomy (RARP) in a single low-intermediate volume prostate cancer (PCa) center over a 10-year period.
Materials and methods
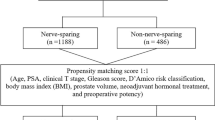
We queried a prospectively maintained database for patients who underwent NS RARP between 2009 and 2018 in a low-intermediate volume PCa center. Risk-groups were defined according to the D’Amico classification. Pentafecta outcomes referred to the postsurgical presence of potency and continence, and the absence of biochemical recurrence (BCR), positive surgical margins (PSM), and perioperative complications. The Kruskall–Wallis test, the t test and the Mann–Whitney tests were used when appropriate.
Results
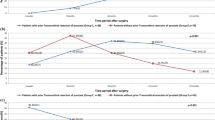
603 patients underwent NS RARP and 484 patients were evaluated for Pentafecta outcomes. Median postsurgical follow-up was 28 months. Overall, 137 (22.7%), 376 (62.3%), and 90 (15%) patients were diagnosed in the low-, intermediate-, and high-risk groups, respectively. Patients undergoing NS RARP shifted from 33 to 20% in the low-risk group, from 52 to 62% in the intermediate-risk group, and from 10 to 13% in the high-risk group. Patients reaching Pentafecta increased from 38 to 44%. No postoperative potency was the main reason for non-achieving Pentafecta (71%). BCR strongly limited Pentafecta achievement in the high-risk group (61%), but not in intermediate (24%) and low-risk (30%) groups.
Conclusions
Low-intermediate volume PCa centers show similar trends to high-volume centers regarding risk group distributions over time in PCa patients undergoing NS RARP. We reported an increase in Pentafecta outcomes achievement over time even for experienced surgeons. Pentafecta outcomes achievement is risk-group dependent.





Similar content being viewed by others
Abbreviations
- PSA:
-
Prostate specific antigen
- PCa:
-
Prostate cancer
- BCR:
-
Biochemical recurrence
- NS:
-
Nerve sparing
- RARP:
-
Robot-assisted radical prostatectomy
- LND:
-
Lymph-node dissection
- PSM:
-
Positive surgical margins
- EF:
-
Erectile function
- PDE5:
-
Phosphodiesterase type 5
References
Galper SL, Chen M-H, Catalona WJ, Roehl KA, Richie JP, D’Amico AV (2006) Evidence to support a continued stage migration and decrease in prostate cancer specific mortality. J Urol 175(3):907–912
Tosoian JJ, Carter HB, Lepor A, Loeb S (2016) Active surveillance for prostate cancer: current evidence and contemporary state of practice. Nat Rev Urol 13(4):205–215
Moyer VA, on behalf of the U.S. Preventive Services Task Force (2012) Screening for prostate cancer: U.S. preventive services task force recommendation statement. Ann Intern Med 157(2):120–134
Butler SS, Muralidhar V, Zhao SG, Sanford NN, Franco I, Fullerton ZH (2020) Prostate cancer incidence across stage, NCCN risk groups, and age before and after USPSTF Grade D recommendations against prostate-specific antigen screening in 2012. Cancer 126(4):717–724
van den Bergh R, Gandaglia G, Tilki D, Borgmann H, Ost P, Surcel C (2019) Trends in radical prostatectomy risk group distribution in a european multicenter analysis of 28,572 patients: towards tailored treatment. Eur Urol Focus. 5(2):171–178
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280(11):969–974
Fossati N, Passoni NM, Moschini M, Gandaglia G, Larcher A, Freschi M (2016) Impact of stage migration and practice changes on high-risk prostate cancer: results from patients treated with radical prostatectomy over the last two decades. BJU Int 117(5):740–747
Salomon L, Saint F, Anastasiadis AG, Sebe P, Chopin D, Abbou C-C (2003) Combined reporting of cancer control and functional results of radical prostatectomy. Eur Urol 44(6):656–660
Patel VR, Sivaraman A, Coelho RF, Chauhan S, Palmer KJ, Orvieto MA (2011) Pentafecta: a new concept for reporting outcomes of robot-assisted laparoscopic radical prostatectomy. Eur Urol 59(5):702–707
Jazayeri SB, Weissman B, Samadi DB (2018) Outcomes following robotic-assisted laparoscopic prostatectomy: Pentafecta and Trifecta achievements. Minerva Urol Nefrol 70(1):66–73
Pompe RS, Tian Z, Preisser F, Tennstedt P, Beyer B, Michl U (2017) Short- and long-term functional outcomes and quality of life after radical prostatectomy: patient-reported outcomes from a tertiary high-volume center. Eur Urol Focus 3(6):615–620
Good DW, Stewart GD, Stolzenburg JU, McNeill SA (2014) Analysis of the pentafecta learning curve for laparoscopic radical prostatectomy. World J Urol 32(5):1225–1233
Gershman B, Meier SK, Jeffery MM, Moreira DM, Tollefson MK, Kim SP (2017) Redefining and contextualizing the hospital volume-outcome relationship for robot-assisted radical prostatectomy: implications for centralization of care. J Urol 198(1):92–99
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71(4):618–629
Kessler TM, Burkhard FC, Studer UE (2007) Nerve-sparing open radical retropubic prostatectomy. Eur Urol 51(1):90–97
Briganti A, Chun FKH, Salonia A, Zanni G, Scattoni V, Valiquette L (2006) Validation of a nomogram predicting the probability of lymph node invasion among patients undergoing radical prostatectomy and an extended pelvic lymphadenectomy. Eur Urol 49(6):1019–1026 (discussion 1026–1027)
Briganti A, Larcher A, Abdollah F, Capitanio U, Gallina A, Suardi N (2012) Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol 61(3):480–487
Gandaglia G, Fossati N, Zaffuto E, Bandini M, Dell’Oglio P, Bravi CA (2017) Development and internal validation of a novel model to identify the candidates for extended pelvic lymph node dissection in prostate cancer. Eur Urol 72(4):632–640
Gandaglia G, Zaffuto E, Fossati N, Bandini M, Suardi N, Mazzone E (2018) Identifying candidates for super-extended staging pelvic lymph node dissection among patients with high-risk prostate cancer. BJU Int 121(3):421–427
Donovan JL, Peters TJ, Abrams P, Brookes ST, de Rosette JJ, Schäfer W (2000) Scoring the short form ICSmaleSF questionnaire. International Continence Society. J Urol 164(6):1948–1955
Lepor H, Kaci L, Xue X (2004) Continence following radical retropubic prostatectomy using self-reporting instruments. J Urol 171(3):1212–1215
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD (August 2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Huland H, Graefen M (2015) Changing trends in surgical management of prostate cancer: the end of overtreatment? Eur Urol 68(2):175–178
Pierorazio PM, Ross AE, Han M, Epstein JI, Partin AW, Schaeffer EM (2012) Evolution of the clinical presentation of men undergoing radical prostatectomy for high-risk prostate cancer. BJU Int 109(7):988–993
Zorn KC, Gautam G, Shalhav AL, Clayman RV, Ahlering TE, Albala DM (2009) Training, credentialing, proctoring and medicolegal risks of robotic urological surgery: recommendations of the society of urologic robotic surgeons. J Urol 182(3):1126–1132
Vickers AJ, Bianco FJ, Serio AM, Eastham JA, Schrag D, Klein EA (2007) The surgical learning curve for prostate cancer control after radical prostatectomy. J Natl Cancer Inst 99(15):1171–1177
Asimakopoulos AD, Miano R, Di Lorenzo N, Spera E, Vespasiani G, Mugnier C (2013) Laparoscopic versus robot-assisted bilateral nerve-sparing radical prostatectomy: comparison of pentafecta rates for a single surgeon. Surg Endosc 27(11):4297–4304
Patel VR, Coelho RF, Chauhan S, Orvieto MA, Palmer KJ, Rocco B (2010) Continence, potency and oncological outcomes after robotic-assisted radical prostatectomy: early trifecta results of a high-volume surgeon. BJU Int 106(5):696–702
Greco F, Hoda MR, Wagner S, Reichelt O, Inferrera A, Magno C (2011) Bilateral vs unilateral laparoscopic intrafascial nerve-sparing radical prostatectomy: evaluation of surgical and functional outcomes in 457 patients. BJU Int 108(4):583–587
Author information
Authors and Affiliations
Contributions
LA: project development, data management, data analysis, manuscript writing/editing. MM: project development, data collection, manuscript editing. PB: project development, data collection, manuscript editing. SZ: project development, data collection, manuscript editing. JC: data collection, manuscript editing. GI: data collection, manuscript editing. AM: project development, manuscript writing/editing: LM: project development, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement on the welfare of animals and human rights
This article does not contain any studies/experiments with human participants or animals performed by any of the authors. All persons gave their informed consent to use their data (deidentified) for this retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Afferi, L., Moschini, M., Baumeister, P. et al. Trends in risk-group distribution and Pentafecta outcomes in patients treated with nerve-sparing, robot-assisted radical prostatectomy: a 10-year low-intermediate volume single-center experience. World J Urol 39, 389–397 (2021). https://doi.org/10.1007/s00345-020-03206-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03206-y