Abstract
Though prostate cancer usually responds to androgen deprivation therapy (ADT) in the beginning, the majority of prostate cancers will develop castration resistance over time. The androgen receptor (AR) pathway is often found to be activated in castration resistant prostate cancer (CRPC). Thus, AR signalling remains a therapeutic target upon the development of CRPC. The term M0CRPC is used when ADT leads to castration resistance and there are no metastases detectable by means of conventional imaging. Until recently, there was no therapeutic standard for this group of patients. With the PROSPER-, SPARTAN- and ARAMIS-studies three large placebo-controlled phase III trials have been published lately that showed a significant benefit in metastasis-free survival in men with M0CRPC and short PSA doubling time (PSADT). The efficacy data are very similar in these studies, meaning that the drugs’ safety profiles, final analyses of overall survival and their availability will be more important to help clinicians decide which of these three drugs they use for their patients with M0CRPC.
Similar content being viewed by others
References
EAU Guidelines on Prostate Cancer (2019). EAU Guidelines Office, Arnhem, The Netherlands, presented at the EAU Annual Congress Barcelona 2019
Karantanos T, Evans CP, Tombal B, Thompson TC, Montironi R, Isaacs WB (2015) Understanding the mechanisms of androgen deprivation resistance in prostate cancer at the molecular level. Eur Urol 67(3):470–479. https://doi.org/10.1016/j.eururo.2014.09.049
Gravis G, Boher JM, Joly F, Soulie M, Albiges L, Priou F, Latorzeff I, Delva R, Krakowski I, Laguerre B, Rolland F, Theodore C, Deplanque G, Ferrero JM, Culine S, Mourey L, Beuzeboc P, Habibian M, Oudard S, Fizazi K, Getug K (2016) Androgen deprivation therapy (ADT) plus docetaxel versus ADT Alone in metastatic non castrate prostate cancer: impact of metastatic burden and long-term survival analysis of the randomized phase 3 GETUG-AFU15 trial. Eur Urol 70(2):256–262. https://doi.org/10.1016/j.eururo.2015.11.005
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA, Eisenberger MA, Higano C, Bubley GJ, Dreicer R, Petrylak D, Kantoff P, Basch E, Kelly WK, Figg WD, Small EJ, Beer TM, Wilding G, Martin A, Hussain M, Prostate Cancer Clinical Trials Working G (2008) Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol 26(7):1148–1159. https://doi.org/10.1200/JCO.2007.12.4487
Hong JH, Kim IY (2014) Nonmetastatic castration-resistant prostate cancer. Korean J Urol 55(3):153–160. https://doi.org/10.4111/kju.2014.55.3.153
Cookson MS, Roth BJ, Dahm P, Engstrom C, Freedland SJ, Hussain M, Lin DW, Lowrance WT, Murad MH, Oh WK, Penson DF, Kibel AS (2018) Castration-resistant prostate cancer: AUA Guideline. American Urological Association (AUA). Accessed 12 Oct 2019
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, Iversen P, Bhattacharya S, Carles J, Chowdhury S, Davis ID, de Bono JS, Evans CP, Fizazi K, Joshua AM, Kim CS, Kimura G, Mainwaring P, Mansbach H, Miller K, Noonberg SB, Perabo F, Phung D, Saad F, Scher HI, Taplin ME, Venner PM, Tombal B, the PI (2014) Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med 371(5):10. https://doi.org/10.1056/NEJMoa1405095
Kirby M, Hirst C, Crawford ED (2011) Characterising the castration-resistant prostate cancer population: a systematic review. Int J Clin Pract 65(11):1180–1192. https://doi.org/10.1111/j.1742-1241.2011.02799.x
Smith MR, Saad F, Oudard S, Shore N, Fizazi K, Sieber P, Tombal B, Damiao R, Marx G, Miller K, Van Veldhuizen P, Morote J, Ye Z, Dansey R, Goessl C (2013) Denosumab and bone metastasis-free survival in men with nonmetastatic castration-resistant prostate cancer: exploratory analyses by baseline prostate-specific antigen doubling time. J Clin Oncol 31(30):3800–3806. https://doi.org/10.1200/JCO.2012.44.6716
Smith MR, Kabbinavar F, Saad F, Hussain A, Gittelman MC, Bilhartz DL, Wynne C, Murray R, Zinner NR, Schulman C, Linnartz R, Zheng M, Goessl C, Hei YJ, Small EJ, Cook R, Higano CS (2005) Natural history of rising serum prostate-specific antigen in men with castrate nonmetastatic prostate cancer. J Clin Oncol 23(13):2918–2925
DePuy V, Anstrom KJ, Castel LD, Schulman KA, Weinfurt KP, Saad F (2007) Effects of skeletal morbidities on longitudinal patient-reported outcomes and survival in patients with metastatic prostate cancer. Support Care Cancer 15(7):869–876. https://doi.org/10.1007/s00520-006-0203-x
McKay R, Haider B, Duh MS, Valderrama A, Nakabayashi M, Fiorillo M, Ristovska L, Wen L, Kantoff P (2017) Impact of symptomatic skeletal events on health-care resource utilization and quality of life among patients with castration-resistant prostate cancer and bone metastases. Prostate Cancer Prostatic Dis 20(3):276–282. https://doi.org/10.1038/pcan.2017.4
Chong JT, Oh WK, Liaw BC (2018) Profile of apalutamide in the treatment of metastatic castration-resistant prostate cancer: evidence to date. Onco Targets Ther 11:2141–2147. https://doi.org/10.2147/OTT.S147168
Tran C, Ouk S, Clegg NJ, Chen Y, Watson PA, Arora V, Wongvipat J, Smith-Jones PM, Yoo D, Kwon A, Wasielewska T, Welsbie D, Chen CD, Higano CS, Beer TM, Hung DT, Scher HI, Jung ME, Sawyers CL (2009) Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science 324(5928):787–790. https://doi.org/10.1126/science.1168175
Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, de Wit R, Mulders P, Chi KN, Shore ND, Armstrong AJ, Flaig TW, Flechon A, Mainwaring P, Fleming M, Hainsworth JD, Hirmand M, Selby B, Seely L, de Bono JS (2012) Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med 367(13):1187–1197. https://doi.org/10.1056/NEJMoa1207506
Penson DF, Armstrong AJ, Concepcion R, Agarwal N, Olsson C, Karsh L, Dunshee C, Wang F, Wu K, Krivoshik A, Phung D, Higano CS (2016) Enzalutamide versus bicalutamide in castration-resistant prostate cancer: the STRIVE Trial. J Clin Oncol 34(18):2098–2106. https://doi.org/10.1200/JCO.2015.64.9285
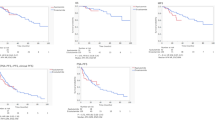
Hussain M, Fizazi K, Saad F, Rathenborg P, Shore N, Ferreira U, Ivashchenko P, Demirhan E, Modelska K, Phung KA, Sternberg CN (2018) Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. N Engl J Med 378(26):2465–2474. https://doi.org/10.1056/NEJMoa1800536
Clegg NJ, Wongvipat J, Joseph JD, Tran C, Ouk S, Dilhas A, Chen Y, Grillot K, Bischoff ED, Cai L, Aparicio A, Dorow S, Arora V, Shao G, Qian J, Zhao H, Yang G, Cao C, Sensintaffar J, Wasielewska T, Herbert MR, Bonnefous C, Darimont B, Scher HI, Smith-Jones P, Klang M, Smith ND, De Stanchina E, Wu N, Ouerfelli O, Rix PJ, Heyman RA, Jung ME, Sawyers CL, Hager JH (2012) ARN-509: a novel antiandrogen for prostate cancer treatment. Cancer Res 72(6):1494–1503. https://doi.org/10.1158/0008-5472.Can-11-3948
Smith MR, Antonarakis ES, Ryan CJ, Berry WR, Shore ND, Liu G, Alumkal JJ, Higano CS, Chow Maneval E, Bandekar R, de Boer CJ, Yu MK, Rathkopf DE (2016) Phase 2 study of the safety and antitumor activity of apalutamide (ARN-509), a potent androgen receptor antagonist, in the high-risk nonmetastatic castration-resistant prostate cancer cohort. Eur Urol 70(6):963–970. https://doi.org/10.1016/j.eururo.2016.04.023
Smith MR, Saad F, Chowdhury S, Oudard S, Hadaschik BA, Graff JN, Olmos D, Mainwaring PN, Lee JY, Uemura H, Lopez-Gitlitz A, Trudel GC, Espina BM, Shu Y, Park YC, Rackoff WR, Yu MK, Small EJ, Investigators S (2018) Apalutamide treatment and metastasis-free survival in prostate cancer. N Engl J Med 378(15):1408–1418. https://doi.org/10.1056/NEJMoa1715546
Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, Nykanen PS, Tormakangas OP, Palvimo JJ, Kallio PJ (2015) Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies. Sci Rep 5:12007. https://doi.org/10.1038/srep12007
Fizazi K, Massard C, Bono P, Kataja V, James N, Tammela TL, Joensuu H, Aspegren J, Mustonen M (2017) Safety and antitumour activity of ODM-201 (BAY-1841788) in castration-resistant, CYP17 inhibitor-naive prostate cancer: results from extended follow-up of the ARADES Trial. Eur Urol Focus 3(6):606–614. https://doi.org/10.1016/j.euf.2017.01.010
Fizazi K, Smith MR, Tombal B (2018) Clinical development of darolutamide: a novel androgen receptor antagonist for the treatment of prostate cancer. Clin Genitourin Cancer 16(5):332–340. https://doi.org/10.1016/j.clgc.2018.07.017
Zurth C, Sandmann S, Trummel D, Seidel D, Gieschen H (2018) Blood-brain barrier penetration of [14C]darolutamide compared with [14C]enzalutamide in rats using whole body autoradiography. J Clin Oncol 36(6_suppl):345–345. https://doi.org/10.1200/JCO.2018.36.6_suppl.345
Fizazi K, Massard C, Bono P, Jones R, Kataja V, James N, Garcia JA, Protheroe A, Tammela TL, Elliott T, Mattila L, Aspegren J, Vuorela A, Langmuir P, Mustonen M, Group As (2014) Activity and safety of ODM-201 in patients with progressive metastatic castration-resistant prostate cancer (ARADES): an open-label phase 1 dose-escalation and randomised phase 2 dose expansion trial. Lancet Oncol 15(9):975–985. https://doi.org/10.1016/S1470-2045(14)70240-2
Fizazi K, Shore N, Tammela TL, Ulys A, Vjaters E, Polyakov S, Jievaltas M, Luz M, Alekseev B, Kuss I, Kappeler C, Snapir A, Sarapohja T, Smith MR, Investigators A (2019) Darolutamide in nonmetastatic, castration-resistant prostate cancer. N Engl J Med 380(13):1235–1246. https://doi.org/10.1056/NEJMoa1815671
Potter GA, Barrie SE, Jarman M, Rowlands MG (1995) Novel steroidal inhibitors of human cytochrome P45017 alpha (17 alpha-hydroxylase-C17,20-lyase): potential agents for the treatment of prostatic cancer. J Med Chem 38(13):2463–2471. https://doi.org/10.1021/jm00013a022
Attard G, Belldegrun AS, de Bono JS (2005) Selective blockade of androgenic steroid synthesis by novel lyase inhibitors as a therapeutic strategy for treating metastatic prostate cancer. BJU Int 96(9):1241–1246. https://doi.org/10.1111/j.1464-410X.2005.05821.x
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, Chi KN, Jones RJ, Goodman OB Jr, Saad F, Staffurth JN, Mainwaring P, Harland S, Flaig TW, Hutson TE, Cheng T, Patterson H, Hainsworth JD, Ryan CJ, Sternberg CN, Ellard SL, Flechon A, Saleh M, Scholz M, Efstathiou E, Zivi A, Bianchini D, Loriot Y, Chieffo N, Kheoh T, Haqq CM, Scher HI (2011) Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 364(21):1995–2005. https://doi.org/10.1056/NEJMoa1014618
Ryan CJ, Crawford ED, Shore ND, Underwood W 3rd, Taplin ME, Londhe A, Francis PSJ, Phillips J, McGowan T, Kantoff PW (2018) The IMAAGEN Study: effect of abiraterone acetate and prednisone on prostate specific antigen and radiographic disease progression in patients with nonmetastatic castration resistant prostate cancer. J Urol 200(2):344–352. https://doi.org/10.1016/j.juro.2018.03.125
Xie W, Regan MM, Buyse M, Halabi S, Kantoff PW, Sartor O, Soule H, Clarke NW, Collette L, Dignam JJ, Fizazi K, Paruleker WR, Sandler HM, Sydes MR, Tombal B, Williams SG, Sweeney CJ, Group ICW (2017) Metastasis-free survival is a strong surrogate of overall survival in localized prostate cancer. J Clin Oncol 35(27):3097–3104. https://doi.org/10.1200/JCO.2017.73.9987
Smith MR (2018) Association of metastasis-free survival (MFS) and overall survival (OS) in nonmetastatic castration-resistant prostate cancer (nmCRPC). In: Paper presented at the ASCO Annual Meeting, Chicago, IL, USA, 1–5 June 2018
Small EJ, Saad F, Chowdhury S, Oudard S, Hadaschik BA, Graff JN, Olmos D, Mainwaring PN, Lee JY, Uemura H, De Porre P, Smith AA, Zhang K, Lopez-Gitlitz A, Smith MR (2019) Apalutamide and overall survival in non-metastatic castration-resistant prostate cancer. Ann Oncol. https://doi.org/10.1093/annonc/mdz397
Tombal B, Saad F, Penson D, Hussain M, Sternberg CN, Morlock R, Ramaswamy K, Ivanescu C, Attard G (2019) Patient-reported outcomes following enzalutamide or placebo in men with non-metastatic, castration-resistant prostate cancer (PROSPER): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol 20(4):556–569. https://doi.org/10.1016/S1470-2045(18)30898-2
Saad F, Cella D, Basch E, Hadaschik BA, Mainwaring PN, Oudard S, Graff JN, McQuarrie K, Li S, Hudgens S, Lawson J, Lopez-Gitlitz A, Yu MK, Smith MR, Small EJ (2018) Effect of apalutamide on health-related quality of life in patients with non-metastatic castration-resistant prostate cancer: an analysis of the SPARTAN randomised, placebo-controlled, phase 3 trial. Lancet Oncol 19(10):1404–1416. https://doi.org/10.1016/S1470-2045(18)30456-X
Bouchelouche K, Choyke PL (2018) Advances in prostate-specific membrane antigen PET of prostate cancer. Curr Opin Oncol 30(3):189–196. https://doi.org/10.1097/CCO.0000000000000439
Author information
Authors and Affiliations
Contributions
YH-B project development, data management, manuscript writing. BH project development, manuscript writing/editing. JH project development, data management, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflicts of interest
Y. Hess-Busch reports non-financial support from Roche and BMS. J. Hess reports grants and personal fees and non-financial support from Boston Scientific and personal fees and non-financial support from Bayer, Janssen and MSD. B. Hadaschik reports grants, personal fees and non-financial support from Janssen, personal fees and non-financial support from Astellas, AstraZeneca, Bayer, BMS, Lightpoint Medical, and Uromed.
Ethical approval
Research did not involve human participants and/or animals. No informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hess-Busch, Y., Hadaschik, B. & Hess, J. M0CRPC overview of management options. World J Urol 39, 349–356 (2021). https://doi.org/10.1007/s00345-019-02997-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02997-z