Abstract
Purpose
To correlate ureteral lesions visualized during ureteroscopy with histopathological findings.
Materials and methods
Ureteral access sheaths (UAS) sized 13/15 Fr. were inserted bilaterally in 22 laboratory pigs. During retraction of the UAS with a semirigid ureteroscope inside, ureteral lesions were evaluated and registered using the Post-ureteroscopic lesion scale (PULS). Ureters were excised in vivo between the uretero–pelvic junction and the uretero–vesical junction. Embedded in paraffin, 4-µm thick sections were step sectioned at 250–300 µm intervals and haematoxylin and eosin (HE) stained. Histopathological scoring of ureteral wall lesions was subsequently performed according to PULS.
Results
In 72.1% of ureters, the highest histopathological score was at least 1 grade higher than the highest endoscopic PULS score. For 12 (27.9%) lesions, the difference was 2 scores higher, and for 1 (2.3%), it was 3 scores higher. The histopathological PULS grade was higher than the endoscopical PULS grade at all minimum, quartile, and maximum scores. There was a significant difference in the distribution of highest lesional scores between the endoscopic and histopathological PULS (p = 0.002). The calculated mean of the highest scores was 1.49 for endoscopic PULS and 2.51 for histopathological PULS (p < 0.0001).
Conclusion
Histopathological evaluation of ureteral wall lesions after UAS placement revealed a significantly higher degree of severity than observed endoscopically. Thus, endoscopy underestimated the histopathological extent of the lesion in the majority of cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retrograde intrarenal surgery (RIRS) is widely used for treatment of kidney stones and for diagnosis and treatment of other intrarenal pathologies. The endoscopes and ureteral access sheaths (UAS) that are used for the procedures are continuously getting smaller, but the risk of harming the ureteral wall when inserting an instrument to access the renal pelvis persists [1, 2]. Animal studies have shown that ureteral dilation with endoscopes and UAS as well as by ureteral obstruction can decrease perioperative ureteral blood flow, and subsequently cause inflammation, necrosis, and ureteral wall thickening with collagen deposition [3–5].
Recently, prospective clinical studies have focused on the risk of having a ureteral lesion from retrograde procedures done with the aid of UAS. In a series of 359 patients, UAS sized 12/14 Fr. caused ureteral injury in 46.5%, of which 13.3% involved the ureteral muscular coat [1]. A 101 patient series on UAS sizes 9.5/11.5 and 12/14 Fr. found mucosal damage in 38.6% and smooth muscle layer lesions in 2.9% [2]. In a study of 148 preoperatively JJ-stented cases using 14–16 Fr. UAS, 39.9% had superficial mucosal lesions, 17.6% had deeper mucosal lesions, and 4.7% patients had circumferential perforation [6]. These reports show that ureteral damage does occur. In order to perform uniform clinical decisions, grading systems for objective evaluation of postoperative ureteral lesions have recently been proposed [1, 7]. For this purpose the Post-ureteroscopic lesion scale (PULS) was developed [7]. PULS is a validated system with high inter-rater reliability for endoscopically assessable ureteral lesions. Although the system, if used correctly, offers a clinical tool that directs the attention of the surgeon to prevent possible postoperative complications, we hypothesized that direct observation of visible lesions may in some cases only be a sign of greater underlying damage.
The aim of this study was to correlate endoscopically evaluable ureteral lesions to the corresponding histopathological lesion in order to further validate ureteral lesion grading systems and improve the quality of clinical decisions.
Materials and methods
Experimental animals
The animal protocols were approved by The National Animal Experiments Inspectorate (Copenhagen, Denmark). Studies were performed on 22 anesthetized female pigs weighing 55 kg (Påskehøjgård, Ølsted, Denmark). The pigs were fed a standard diet during breeding. Before the study, they had access to water but were fasting 12 h prior to anesthesia.
After premedication with azaperone (4 mg/kg) and midazolam (4 mg/kg), anesthesia was induced by propofol (4–20 mg/kg) and maintained with sevoflurane (1.2 MAC) and fentanil (0.03 mg/kg/h). The pigs were orotracheally intubated and mechanically ventilated (GE Healthcare S5 Avance). Hydration was maintained by administration of saline (9 g/l sodium chloride; 10 ml/kg/h) at a temperature of 37 °C through an ear vein.
A cystoscope was inserted through the urethra into the bladder. A ureteral catheter (Selectip®, Bard Medical, Covington, Georgia, USA) was placed in the distal part of the ureter on one side, and a retrograde pyelography was performed to visualize the anatomy of the upper urinary tract. A guidewire (0.035 inches/150 cm, Sensor®, Boston Scientific, Marlborough, MA, USA) was inserted via the ureteral catheter to the renal pelvis, and the cystoscope was removed. The ureter size of the type of pigs evaluated in the present study was found to be slightly larger than the normal human ureter. In a pilot series, the clinical feeling of placing a 13/15 Fr. UAS in the pig ureters was equivalent to placing 12/14 Fr. UASs in human ureters, and therefore this UAS size was chosen as the appropriate size for the experiment. Over the guidewire, under fluoroscopic guidance, a hydrophilic UAS (13/15 Fr × 36 cm, Navigator™ Ureteral Access Sheath, Boston Scientific, Marlborough, MA, USA) was inserted. During retraction of the UAS with a semirigid ureteroscope (Karl Storz Endoskope, Tuttlingen, Germany, 7 Fr.) inside, ureteral lesions were evaluated and graded according to the PULS classification system (endoscopic PULS) [7] (Table 1; Fig. 1). The insertion and extraction procedure was performed bilaterally. All procedures were performed by two experienced endourologists (KHA, PJSO).
Examples of Endoscopic PULS grade 1, 2, and 3 lesions as visualized during endoscopic video recordings (see Table 1)
Through a midline abdominal incision, both ureters were exposed and carefully excised in vivo including surrounding connective tissue between the uretero–pelvic junction and the uretero–vesical junction.
Each ureter was immersed and stored in neutral, buffered formalin 10% (Hounisen, DK) for preservation until histopathological processing in the laboratory.
Finally, the pigs were euthanized under anesthesia with 20 ml of pentobarbital, 200 mg/ml.
Tissue processing
After fixation, the ureters were cut at right angle to the tubular organ into pieces of equal length. 37 of the ureters were cut into 8 pieces, but 6 of the harvested ureters were shorter in length, thus yielding only 7, 6, and 4 pieces of equal length. Each of these pieces were then further cut into 3 pieces, and each triplet was placed in one tissue container, routinely processed, and embedded in the same paraffin (Tissue-Tek Paraform™, Sakura, DK) block. Four µm thick sections were step sectioned at 250–300 µm intervals, using a rotation microtome, producing step sections from ≥10 levels, which were mounted on Superfrost Plus™ slides (Menzel-Gläser, Thermo Scientific, DK). After rehydration, the histological sections underwent staining with Mayer’s haematoxylin and eosin (HE), followed by dehydration and were cover slipped, using Pertex™ (Sakura, DK). Thus 240 histologic sections (120–210 for the 6 shorter ureters) were available from each ureter, covering the whole length of the organ (Fig. 2).
After fixation, the ureters were cut at right angle to the tubular organ into pieces of equal length. Each of these pieces were then further cut into 3 pieces, and each triplet was placed in one tissue container, routinely processed, and embedded in paraffin. Four-µm thick sections were step sectioned at 250–300 µm intervals, producing step sections from ≥10 levels. Thus 240 histologic sections (120–210 for the 6 shorter ureters) were available from each ureter, covering the whole length of the organ
Histopathological scoring of ureteral lesions
The pathologist was blinded to the endoscopic PULS grade. Scoring of histopathological ureteral lesions was based on PULS (histopathological PULS) [7] (Table 1; Fig. 3), with a few modifications, as summarized in Table 1. In the case of tangential sections with no possibility to evaluate the whole ureteral circumference, a score of “not determined” (ND) was given, unless a significant lesion (histopathological PULS ≥1) was seen in the remaining part of the evaluable ureteral wall.
Examples of histopathological PULS grade 0–4 lesions (see Table 1)
The highest endoscopic PULS and the highest histopatholocial PULS for each ureter were deducted as the primary outcome measures in order to compare the results of the two scoring modalities.
Statistical analysis
Statistical analysis was performed with Stata (StataCorp, Texas) comparing mean and quartile scores, and using Wilcoxon signed-rank test for significance. Fisher’s exact test was used for analysis of difference in the distribution of highest lesional scores; p < 0.05 was considered significant.
Results
A total of 44 ureters were harvested from the experimental animals. Due to a technical error, no intraoperative evaluation was obtained from one of the ureters and this specimen was excluded, yielding 43 samples for final analysis. A total of 3310 histological sections were morphologically evaluated. 65 (2%) of the sections were cut tangentially, making them incomplete in ureteral circumference, and therefore not determinable (ND) regarding lesional score (Table 2).
All endoscopically visible lesions were scored using the PULS grading system and were assigned an endoscopic PULS score [2], and it was registered using endoscopy and fluoroscopy whether the lesion was found in proximal, middle, or distal ureter. Histopathological PULS scoring for the whole ureter in each individual ureteral unit is presented in Table 2, creating a numerical visual image of the lesions.
Endoscopic PULS ranged between 0 and 3 compared to histopathological PULS ranging between 0 and 4. In 8 of 43 ureteral units, no lesions were observed endoscopically (18%). Histopathologically, no ureteral units were without lesions.
Comparing the highest endoscopic PULS score with the highest histopathological PULS score, only in 1 (2.3%) of the ureters, the endoscopic PULS score was 1 point higher than the histopathological score, and in 11 ureters (25.6%), they were equal (Table 2). In the remaining 31 ureters (72.1%), the histopathological PULS was at least 1 grade higher than the endoscopic PULS score. For 12 (27.9%) of these, the difference was 2 score points, and for 1 (2.3%), it was 3 points.
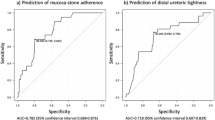
Statistical analysis using only the highest lesional scores showed that there was a highly significant difference between endoscopic and histopathological PULS grading (p = 0.002) (Table 3). The histopathological PULS score was at least 1 grade higher than the endoscopic PULS grade for minimum, quartile, and maximum scores (Table 3). The calculated mean of the highest scores was 1.49 for endoscopic PULS and 2.51 for histopathological PULS score (p < 0.0001).
In order not to restrict analysis to the highest registered lesional score for each ureter, we also calculated the mean lesional score for each ureter, thereby comparing the longitudinal extent of lesions registered by the two evaluation systems. For the histopathological PULS scoring, mean scores were calculated as simple means of all evaluation scores. For the endoscopic PULS scores, we used video recordings during extraction of the UAS and ureteroscope to estimate the length of all registered lesions. The length was recorded as being <10%, <20%, <30%, or <40% of the total length of the ureter. If estimation of the length was difficult or uncertain between two intervals, the higher of the two intervals was chosen as the registered length in order not to underestimate the lesion length. The registered length of all lesions was used to calculate a weighted average lesional score for each ureter regarding endoscopic PULS. Finally, a total material, mean lesional score was calculated (Table 4). In all 43 ureteral units, the mean lesional score was higher by histopathological evaluation. The whole material mean endoscopic PULS score was 0.5, and the whole material mean histopathological PULS score was 1.4 (p < 0.001).
The PULS grading system by default only applies to endoscopically assessable injuries. To take this into account, we performed a downgrading of the highest histopathological PULS score from 1 to 0 in 5 cases where the highest endoscopic PULS score was 0. In all cases where the highest histopathological lesional score was >2, no changes were made as lesions of this severity by definition should be endoscopically assessable. By performing this adjustment, the number of ureters, in which the highest endoscopic PULS and histopathological PULS scores were equal, changed from 11 (25.6%) to 16 (37.2%), and the number of ureters, in which the histopathological score was at least 1 grade higher than the endoscopic PULS score, changed from 31 (72.1%) to 26 (60.5%). With this modification, the difference between the highest score between endoscopic and histopathological PULS was still highly significant (p < 0.001).
Discussion
This porcine model attempted to simulate the conditions that exist during clinical RIRS with UAS usage. The study was performed in vivo on upper urinary tracts of pigs because of the anatomical and physiological similarities to conditions in humans, and the animal size was chosen to approximate the size of the ureter of an adult human. All procedures were performed meticulously with respect for ureteral integrity as if they were done in a clinical setting.
To our knowledge, this is the first study reporting on histopathological correlations to endoscopically visualized ureteral lesions. The main finding of our study was that endoscopic grading of ureteral lesions using PULS following UAS usage underestimated the actual histopathological lesions. The exact clinical implication of this finding is uncertain. It may explain the clinical observation that some patients surprisingly develop a rigid, fibrotic ureter after previous retrograde endoscopic procedures, although no obvious lesions were encountered during the initial procedures. Long-term data of patients, primarily endoscopic PULS graded, are warranted for further evaluation of the clinical importance of the present data.
The endoscopic PULS scoring revealed severe lesions (grade 3) in 7 of the ureteral units (16.2%), which is comparable to results reported in clinical studies using UAS sized 12/14 Fr. [7, 1], confirming that our animal model with usage of 13/15 Fr. UASs was comparable to the human clinical setting.
In the histopathological evaluation process, the differentiation between PULS scores 3 and 4 sometimes proved to be challenging, as the degree of circumferential involvement was difficult to estimate. The same applied to the differentiation between scores 2 and 3, where a distinction should be made based upon the depth of the lesion, which was especially difficult in cases where the ureter was very dilated. In all cases where the exact histopathological lesional grade was questionable, we chose to downgrade the severity. In Table 2, which simulates an “image” of the ureter in terms of histopathological lesions, it is noticeable that the longitudinal distribution of lesions was quite coherent and not interrupted by observations of markedly different severity, which corresponds with the clinical feeling of a smooth passage of the UAS without sensation of resistance. We did however at times notice abrupt transitions between grade 1 and 3, where a gradual transition would have been expected (Table 2: ureteral units 9, 32, and 43). This may have occurred due to forced introduction of the UAS during a ureteral contraction (peristalsis), which was not noticed by the surgeon. It is well known that rising pressure in the renal pelvis may promote peristalsis due to activation of pacemaker cells [8]. Overfilling of the collecting system thus may be involved in access-related ureteral injuries [8].
During histopathological scoring of lesions, other observations were made, such as profound ureteral dilatation sometimes accompanied by total epithelial denudation but without lesion of the muscular coat; de-epithelialization with luminal fibrin casts; sub-mucosal edema and hematoma; acute neutrophil inflammation often with angiocentric location; and focal necrosis. These findings correspond with previous findings demonstrating a marked up-regulation of proinflammatory mediators in the ureteral wall following UAS usage [5]. Interestingly, we also saw varying degrees of focal eosinophilia, at times very profound and located under the mucosal or deep in the muscular layers. We do not know of any reason why the laboratory animal should present with eosinophilia in the ureter, but we did sometimes observe luminal foreign bodies of gel-like appearance, which may be remnants of the hydrophilic coating the UAS. Whether this may have any implications for postoperative outcome needs to be further evaluated.
Post-ureteroscopic ureteral lesional scores have in part been developed as an instrument to decide whether the patient should be stented or not [1, 2, 7]. In 19 (44.2%) of cases in our study, the PULS grade was upgraded from superficial to severe (from grade 1 or 2 to grade 3 or 4) by histopathological evaluation. This suggests that some of the observed superficial lesions could possibly represent penetrating lesions and as such accordingly should be followed by JJ-stenting. Whether our observations also may have clinical implications for immediate as well as long-term outcome with regard to ureteral function needs to be evaluated in a clinical setting using ureteral lesional scoring.
Conclusions
Endoscopical evaluation of ureteral lesions using the PULS grading system following UAS placement in a porcine model underestimated the actual histopathological lesion. The findings may explain why ureteral malfunction occurs in some individuals following ureteral instrumentation.
References
Traxer O, Thomas A (2013) Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J Urol Elsevier Inc 189(2):580–584
Guzelburc V, Guven S, Boz MY, Erkurt B, Soytas M, Altay B et al (2016) Intraoperative evaluation of ureteral access sheath-related injuries using post-ureteroscopic lesion scale. J Laparoendosc Adv Surg Tech A 26(1):23–26
Dinlenc CZ, Liatsikos EN, Smith AD (2002) Ureteral ischemia model: an explanation of ureteral dysfunction after chronic obstruction. J Endourol 16(1):47–50
Lallas CD, Auge BK, Raj GV, Santa-Cruz R, Madden JF, Preminger GM (2002) Laser doppler flowmetric determination of ureteral blood flow after ureteral access sheath placement. J Endourol 16(8):583–590
Lildal SK, Nørregaard R, Andreassen KH, Christiansen FE, Jung H, Pedersen MR et al (2017) Ureteral access sheath influence on the ureteral wall evaluated by cyclooxygenase-2 and tumour necrosis factor-α in a porcine model. J Endourol 31(3):307–313
Miernik A, Wilhelm K, Ardelt PU, Adams F, Kuehhas FE, Schoenthaler M (2012) Standardized flexible ureteroscopic technique to improve stone-free rates. Urology 80(6):1198–1202
Schoenthaler M, Buchholz N, Farin E, Ather H, Bach C, Bach T et al (2014) The post-ureteroscopic lesion scale (PULS): a multicenter video-based evaluation of inter-rater reliability. World J Urol 32(4):1033–1040
Osther PJS, Pedersen KV, Lildal SK, Pless MS, Andreassen KH, Osther SS et al (2015) Pathophysiological aspects of ureterorenoscopic management of upper urinary tract calculi. Curr Opin Urol 26(1):63–69
Acknowledgements
The authors thank Hanne Rasmussen, Department of Clinical Pathology, Lillebaelt Hospital, Vejle, Denmark (tissue processing) and Henrik Sørensen, Institute of Clinical Research, Aarhus University, Aarhus, Denmark (laboratory animals) for expert technical assistance.
Author information
Authors and Affiliations
Contributions
Protocol/project development: S.K. Lildal, F.B. Sørensen, K.H. Andreassen, P.J.S. Osther. Data collection: S.K. Lildal, F.B. Sørensen, K.H. Andreassen, F.S. Christiansen, H. Jung, M.R. Christiansen, P.J.S. Osther. Data management: S. K. Lildal. Data analysis: S.K. Lildal, F.B. Sørensen, K.H. Andreassen, P.J.S. Osther. Manuscript writing: S.K. Lildal. Manuscript editing: S.K. Lildal, F.B. Sørensen, K.H. Andreassen, F.S. Christiansen, H. Jung, M.R. Christiansen, P.J.S. Osther.
Corresponding author
Ethics declarations
Funding
The Japanese-Swedish Research Foundation and the Research Foundation of Lillebaelt Hospital supported the study, but had no influence on study design, performance, analysis of data and publication.
Conflict of interest
K.H. Andreassen has received speaker honoraria from Boston Scientific. P.J.S. Osther is member of advisory boards of Olympus, Boston Scientific, and Coloplast. P.J.S. Osther has received speaker honoraria from Olympus, Cook Medical, Boston Scientific, Karl Storz Endoskope, and Coloplast.
Human and animal rights statement
The research did not involve human participants. The animal studies complied with national ethical standards, and the protocols were approved by The National Animal Experiments Inspectorate (Copenhagen, Denmark) (Animal approved project number 2014-15-2934-01015).
Informed consent
N.A. (the study did not involve human participants).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lildal, S.K., Sørensen, F.B., Andreassen, K.H. et al. Histopathological correlations to ureteral lesions visualized during ureteroscopy. World J Urol 35, 1489–1496 (2017). https://doi.org/10.1007/s00345-017-2035-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-017-2035-3