Abstract
Objective
To evaluate the efficacy and safety of skeletonized mesh implants for advanced pelvic organ prolapse (POP).
Methods
Women with advances POP underwent repair of stage III or greater anterior or posterior and apical compartment prolapse using skeletonized mesh implants (Seratom PA MR MN® system—SERAG-WIESSNER, Naila, Germany). Anatomical outcomes were assessed using pelvic organ prolapse quantification staging and functional outcomes were self-reported by the patients at 6 weeks, 6 and 12 months. Anatomical and functional cure rates, post-operative pain and dyspareunia as well as intra and post-operative complications were reported. Success was defined as a composite of no bulge symptoms and no prolapse beyond the hymenal ring.
Results
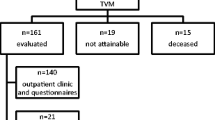
At 12 months, data were available for 103 of the 105 patients originally recruited. Intra-operative complications included 2 (2 %) cases of cystotomy that were corrected vaginally. The immediate post-operative complications included 1 patient (1 %) with UTI, 4 (3.9 %) cases of self-resolved hematomas, and 6 (5.8 %) cases of bladder outlet obstruction. At 12 months, a high success rate and low complication rate was noted. Recurrence of prolapse was reported by 7 (6.6 %) patients. However, only 4 (3.8 %) underwent a repeat procedure. Two patient developed de novo SUI, and 6 (5.7 %) developed dyspareunia. No cases of mesh erosion/extrusion were noted.
Conclusion
The present study showed excellent anatomical and quality of life results in patients with advanced POP treated with a skeletonized and reduced mesh system. No mesh exposure was recorded within the first year after surgery.



Similar content being viewed by others
References
Haylen BT, Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN, International Urogynecological Association, International Continence Society (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29:4–20
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M (2014) Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol 123:1201–1206
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, Markland AD (2014) Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol 123:141–148
Tzur T, Yohai D, Weintraub AY (2016) The role of local estrogen therapy in the management of pelvic floor disorders. Climacteric. 2016 Feb 2:1–10. [Epub ahead of print]
Nguyen JN, Burchette RJ (2008) Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol 111:891–898
Weber AM, Walters MD, Piedmonte MR, Ballard LA (2001) Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol 185:1299–1304
Petros PE, Ulmsten UI (1993) An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol 153(Suppl):1–93
Skoczylas LC, Turner LC, Wang L, Winger DG, Shepherd JP (2014) Changes in prolapse surgery trends relative to FDA notifications regarding vaginal mesh. Int Urogynecol J 25:471–477
Abed H, Rahn DD, Lowenstein L, Balk EM, Clemons JL, Rogers RG (2011) Systematic Review Group of the Society of Gynecologic Surgeons Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. Int Urogynecol J 22:789–798
Vu MK, Letko J, Jirschele K, Gafni-Kane A, Nguyen A, Du H, Goldberg RP (2012) Minimal mesh repair for apical and anterior prolapse: initial anatomical and subjective outcomes. Int Urogynecol J 23:1753–1761
http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm061976.htm. Accessed 17 October, 2015
http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm. Accessed 17 October 2015
Committee on Gynecologic Practice (2012) Vaginal placement of synthetic mesh for pelvic organ prolapse. Female Pelvic Med Reconstr Surg 18:5–9
Davila GW, Baessler K, Cosson M, Cardozo L (2012) Selection of patients in whom vaginal graft use may be appropriate. Consensus of the 2nd IUGA Grafts Roundtable: optimizing safety and appropriateness of graft use in transvaginal pelvic reconstructive surgery. Int Urogynecol J 23:S7–S14
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Friedman T, Neuman M, Peled Y, Krissi H (2015) A new reusable suturing device for vaginal sacrospinous fixation: feasibility and safety study. Eur J Obstet Gynecol Reprod Biol 193:23–26
Lo TS, Tan YL, Cortes EF, Pue LB, Wu PY, Al-Kharabsheh A (2015) Anterior-apical single-incision mesh surgery (SIMS): surgical and functional outcomes at 1 year. J Minim Invasive Gynecol. 22:50–56
Rapp DE, King AB, Rowe B, Wolters JP (2014) Comprehensive evaluation of anterior elevate system for the treatment of anterior and apical pelvic floor descent: 2-year followup. J Urol 191:389–394
Fialkow MF, Newton KM, Weiss NS (2008) Incidence of recurrent pelvic organ prolapse 10 years following primary surgical management: a retrospective cohort study. Int Urogynecol J Pelvic Floor Dysfunct. 19:1483–1487
Lo TS, Pue LB, Tan YL, Wu PY (2014) Long-term outcomes of synthetic transobturator nonabsorbable anterior mesh versus anterior colporrhaphy in symptomatic, advanced pelvic organ prolapse surgery. Int Urogynecol J 25:257–264
Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, Heinonen PK (2010) Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol 203:235.e1–8
Menefee SA, Dyer KY, Lukacz ES, Simsiman AJ, Luber KM, Nguyen JN (2011) Colporrhaphy compared with mesh or graft-reinforced vaginal paravaginal repair for anterior vaginal wall prolapse: a randomized controlled trial. Obstet Gynecol 118:1337–1344
Önol FF, Tosun F, Güzel R, Boylu U, Küçük EV, Gümüş E (2012) Minimum 1.5-year results of “surgeon-tailored” transvaginal mesh repair for female stress urinary incontinence and pelvic organ prolapse. Urology 80:273–279
Moore RD, Mitchell GK, Miklos JR (2012) Single-incision vaginal approach to treat cystocele and vault prolapse with an anterior wall mesh anchored apically to the sacrospinous ligaments. Int Urogynecol J 23:85–91
Turgal M, Sivaslioglu A, Yildiz A, Dolen I (2013) Anatomical and functional assessment of anterior colporrhaphy versus polypropylene mesh surgery in cystocele treatment. Eur J Obstet Gynecol Reprod Biol 170:555–558
Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M (2006) Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct 17:315–320
Yalcin I, Bump RC (2003) Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol 189:98–101
Author contributions
Adi Y. Weintraub was involved in data analysis and manuscript writing/editing; Menahem Neuman was involved in protocol/project development, data collection and manuscript writing/editing; Yonatan Reuven was involved in data analysis and manuscript writing/editing; Joerg Neymeyer was involved in manuscript editing; and Naama Marcus-Braun was involved in protocol/project development, data analysis and manuscript writing/editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors AYW, YR and NMB have nothing to declare, MN receives royalties from SERAG-WIESSNER, and JN serves as a consultant for SERAG-WIESSNER.
Ethical approval
The study was approved by the local institutional ethics committee in accordance with the principles of the Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Weintraub, A.Y., Neuman, M., Reuven, Y. et al. Efficacy and safety of skeletonized mesh implants for advanced pelvic organ prolapse: 12-month follow-up. World J Urol 34, 1491–1498 (2016). https://doi.org/10.1007/s00345-016-1792-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1792-8