Abstract
Purpose
To investigate whether the position of the tape under the urethra may influence ‘outside-in’ transobturator sling (TOT) outcome.
Methods
The study comprised 141 women who underwent TOT for clinically and urodynamically proved stress urinary incontinence. The postoperative ultrasound examination with an endovaginal biplane probe was performed before discharging the patients from hospital. The measurements obtained described the position of the tape relative to the urethra and pubic symphysis, as well as anatomical relationships in the anterior compartment.
Results
Ninety-six (68.1 %) patients were cured, 27 (19.1 %) significantly improved, and in 18 cases (12.7 %), the surgery failed. The tape position under the midurethra (40–70th percentile of the urethral length) or distal urethra (>70th percentile) coincided with better results (cure rate 67.1 and 82.4 %, respectively) than the location in the proximity of the bladder neck (<40th percentile) (21.4 % cured, p = 0.0015 and p < 0.001, respectively). However, the risk of failure was the lowest when the tape was located under the distal urethra. Other ultrasonographic findings were not related to treatment results.
Conclusions
The highest failure rate for ‘outside-in’ TOT is associated with the location of the tape under the proximal third of the urethra. Both the middle and distal sections of the urethra may be regarded as targets for transobturator tape placement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Suburethral synthetic slings are nowadays a first-choice method for surgical treatment of female stress urinary incontinence (SUI) [1]. Since the role of the tape is to reinforce weakened pubouretheral ligaments, its insertion under the middle section of the urethra has been recommended [2–4]. Indeed, several studies confirm the advantages of midurethral tape position [5–8]. The part of the urethra termed ‘the high pressure zone,’ which is estimated to lie between 53 and 72 % of the functional urethral length, has been proposed as the optimal target for suburethral tape placement [9, 10]. Conversely, other reports question any relationship between the tape position relative to the urethra and the sling outcome, emphasizing that the gap between the tape and the pubic symphysis plays a more important role [11–15]. Favorable sling results have also been linked to ultrasonographic parameters reflecting tape tension, such as the compression of the urethra by the tape, described as ‘encroachment,’ or a shorter distance between the urethra and the tape [5–7, 13]. However, due to variable ultrasound techniques used and parameters measured in these studies, their findings are not directly comparable, and the impact of the tape position on the sling outcome is still a matter of discussion.
Previous reports demonstrated that a biplane endovaginal high-frequency ultrasound probe can be successfully used for a detailed evaluation of the urethral structures and surrounding tissues, as well as for a precise identification of the tape’s position under the urethra [16–18]. The aim of the present study was to investigate whether the position of the tape under the urethra can influence the results of an ‘outside-in’ transobturator sling (TOT). In addition, our objective was to determine whether the position and outcome of the sling are related to the ultrasonographic parameters representing anatomical relationships in the urethra.
Materials and method
Between April 2009 and June 2010, 179 women, who had undergone ‘outside-in’ TOT for clinically and urodynamically proved SUI, were prospectively enrolled in the study. Exclusion criteria comprised a previous pelvic reconstructive or anti-incontinence surgery, symptoms of urgency, detrusor overactivity, and anterior vaginal wall prolapse stage III or higher, assessed according to the Pelvic Organ Prolapse Quantification (POP-Q) system [19].
A TOT procedure with a monofilament tape was performed by means of an IVS-04 M device (Covidien®) according to the technique described by Delorme [20]. Fifty-eight patients concomitantly underwent posterior vaginal wall colporrhaphy or posterior mesh reinforcement due to prolapse stage II or III.
Before discharging the patients from hospital, two investigators (M.B. and A.P.W.) conducted endovaginal ultrasound with an ultrasound scanner ProFocus 2202 (B–K Medical, Herlev, Denmark) and a biplane transducer (type 8848; B–K Medical, Herlev, Denmark), frequency range 5–12 MHz, by a standardized technique, as described previously [17, 18]. The 3D volumes obtained were analyzed offline with software provided by the producer. The analysis was conducted independently by two investigators (M.B. and A.P.W.) who were blinded to clinical data and to each other’s measurements. The mean value of the two measurements of each parameter was used for analysis. According to the classification proposed by Shoukri and Pause [21], good to excellent inter- and intraobserver agreement was noted. Interclass correlation coefficients ranged from 0.713 to 0.932. Interobserver reliability was assessed for one investigator (M.B.).
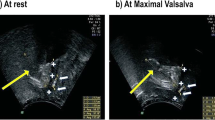
The following measurements were taken at the sagittal plane (Fig. 1a, b):
a, b Measurements taken at the sagittal plane: UL urethral length, BTD the bladder neck–tape distance, TED tape–external urethral meatus distance, BSD bladder neck–pubic symphysis distance, ESD external urethral meatus–pubic symphysis distance, TSD tape–pubic symphysis distance, TLD tape–urethral lumen distance, BN bladder neck, PS pubic symphysis, EUM external urethral meatus. c Measurements taken at the axial plane: APD anterior–posterior diameter, UA urethral area. d Presence of urethral ‘encroachment’
-
1.
Urethral length (UL) was measured from the bladder neck to the external meatus, along the urethral longitudinal axis. Setting the reference point at the midpoint of the tape, the bladder neck tape (BTD) and tape external urethral meatus (TED) distances were determined during the measurement of the UL. The position of the tape relative to the percentile of the UL was calculated, assuming the bladder neck as the proximal end of the urethra.
-
2.
Bladder neck–symphysis pubis distance (BSD)—measured from the bladder neck to the lowest margin of the symphysis pubis.
-
3.
External urethral meatus–symphysis pubis distance (ESD)—measured from the external urethral meatus to the lowest margin of the symphysis pubis.
-
4.
Tape–symphysis pubic distance (TSD)—measured from the midpoint on the tape to the lowest margin of the symphysis pubis.
-
5.
Tape–urethral lumen distance (TLD)—measured as the shortest distance between the tape and the urethral lumen.
At the axial plane, the anterior–posterior diameter (APD) and urethral area (UA) were measured at midurethra, and the whole urethra was inspected for the presence of ‘encroachment’ by the tape (Fig. 1c, d).
One hundred and thirty-six women were able to attend, and 5 were readmitted to hospital because of recurrent stress urinary incontinence before the scheduled period of 24 months. Overall, 141 women were included in further analysis.
Assessments of the sling outcome were performed after 24 months, consisting of a cough test with the patient supine and standing with a comfortably full bladder, and a standard 1-h pad test, as described previously [22]. Patients were considered completely cured if they were free of all subjective SUI symptoms, and if the cough tests and the pad test were negative. The operation was considered as a failure if the patient still reported urine leakage during increases in intra-abdominal pressure, or if the cough test or pad test was positive. In the improved group, the cough test was negative, but patients still reported occasional urinary leakage, or the pad test was negative, but the increase in pad weight was greater than zero and smaller than 1 g.
Ethical approval for the study was obtained from the Ethical Committee of Medical University in Lublin (KE-0245/29/2008). All the patients gave their informed consent prior to inclusion in the study.
Statistical analysis was performed with Statistica Statsoft, version 8 package, using the unpaired t test, the Mann–Whitney U test, χ 2, Pearson’s correlation coefficient, or ANCOVA, as appropriate. A p < 0.05 was considered statistically significant.
Results
Demographic and clinical variables
The analysis of data from 141 patients with known sling outcomes showed that 96 (68.1 %) patients were cured, 27 (19.1 %) significantly improved, and 18 (12.7 %) experienced no significant improvement after the surgery. The patients for whom the surgery was ineffective were older and more frequently postmenopausal than those in the other groups. In addition, women with treatment failure had a higher BMI in comparison with those who were completely dry. Other demographic and clinical factors did not significantly influence sling results (Table 1).
Tape position
The mean tape position was significantly more distal in the cured and improved patients than in those who did not benefit from the surgery (Table 1). The bar charts showing the distribution of the tape’s position relative to the urethral length, presented in Fig. 2, indicate that most of the cured and improved patients had tapes located distally to the 40th percentile. To explore the impact of the location of the tape under the urethra on sling results, the urethra was divided into the proximal (<40th percentile), middle (40th–70th percentile) and distal sections (>70th percentile).
The rate of success, defined as a complete cure, was the highest when the tape was positioned under the distal urethra, but the advantage of this location, compared with the midurethral one, did not reach statistical significance (χ 2 = 3.62, p = 0.057). Both distal and middle positions were superior to the proximal placement. The incidence of treatment failure was the lowest when the tape was implanted under the distal urethra, but the position of the tape under the middle section of the urethra also coincided with a lower failure rate than the position under the proximal section (Table 2). The position of the tape under the urethra was not related to anatomical parameters, such as the urethral length, bladder neck–symphysis pubis distance or external urethral meatus–symphysis pubis distance. The analysis of covariance (ANCOVA) showed that although age (p = 0.046) and BMI (p = 0.002) influenced treatment results, they had no compounding influence on the effect of the tape position (p < 0.001).
The position of the tape in relation to the urethral lumen (tape–urethral lumen distance) or pubis symphysis (tape–symphysis pubic distance), as well as urethral ‘encroachment’, did not influence sling efficacy. Urethral encroachment coincided with a shorter tape–urethral lumen distance (3.8 ± 0.9 vs. 5.3 ± 1.4 mm, p < 0.001) and a shorter tape–symphysis pubic distance (17.7 ± 1.2 vs. 20.8 ± 3.3 mm p < 0.001), which indicate that all these parameters reflect the tension applied during tape placement. Among other parameters determined by ultrasound, a longer bladder neck–symphysis pubis distance and a shorter external urethral meatus–symphysis pubis distance were associated with better results. These differences, however, were no longer statistically significant after ANCOVA was performed, using tape position, age, and BMI as compounding factors.
Complications
In 11 (7.8 %) women, de novo urgency developed after the surgery. None of the ultrasonographic parameters was significantly related to this condition. Only one woman with de novo urgency had a visible tape ‘encroachment’. One patient with the tape located close to the bladder neck was subjected to sling incision. The patients with de novo urgency were older than those free of this complaint (65.6 ± 6.9 vs. 57.0 ± 10.1; p = 0.006).
Five patients had acute postoperative urinary retention requiring a prolonged stay in hospital, and one of them underwent tape incision because of voiding difficulties, but remained continent.
Discussion
The results of our study show a strong relationship between the position of the tape and the outcome of ‘outside-in’ TOT. In line with other reports, we observed that the location of the tape under the proximal urethra, close to the bladder neck, is related to a greater risk of treatment failure [5–8, 23]. In our population, the position of the tape proximally to the 40th percentile of the urethral length was associated with failure in almost 60 % of the patients, whereas the position of the tape distally to the 40th percentile resulted in a substantially higher cure rate. Surprisingly, unlike other investigators, we did not find any association of poorer outcomes with the distal tape position. In fact, the location of the tape at >70th percentile of the urethral length resulted in the lowest failure rate.
It has been observed that the location of the tape close to the bladder neck may predispose to de novo urgency [18, 24]. Statistical analysis of the results of the present study does not support this association. Although patients with the tape under the proximal urethra who develop de novo urgency are encountered in clinical practice, a study comprising a larger population of such patients is needed to prove that the tape position plays a causative role in this complication.
Observations relating sling results to the location of the tape under the urethra imply that greater control over the place where the tape is positioned should produce a higher rate of success. For the retropubic procedure, Kociszewski et al. [10] recommend the preoperative measurement of the urethral length by introital ultrasound and suggest that the site for the beginning of the suburethral incision be calculated according to the one-third rule. These steps are to maximize the probability that TVT is placed under the distal end of the midurethra. The results of the present study indicate that for TOT, it is more important to avoid placing the tape too proximally than to aim at the middle section of the urethra. In most patients, this can be achieved by following the standard rules. However, because of a considerable anatomical variability, including the bony pelvis [25], proximal tape positioning may occur in some patients despite the application of an appropriate surgical technique. To prevent tape displacement during final adjustment, we introduced a modification of the transobturator sling procedure, consisting in the application of 2 additional sutures to the periurethral tissue, 0.5 cm laterally on each side of the midurethra, and between 1.0 and 1.5 cm from the external urethral meatus, which fixate the tape. This step significantly increased the clinical efficacy of the procedure [22].
Reports published previously link the tension of the tape to sling results. The compression of the urethra by the tape at rest and during straining, also termed ‘encroachment,’ associates with better results, but also with a higher incidence of de novo urgency and voiding dysfunctions [5–7, 15, 26]. We did not observe any association of urethral ‘encroachment’ at rest either with surgical results or with voiding difficulties. As in other studies, urethral compression among our patients coincided with a shorter distance between the tape and the urethra, and with a shorter distance between the tape and the pubic symphysis.
Although according to the integral theory, a correction of the vaginal axis may play a major role in the continence status [2]; patients after a posterior vaginal wall repair for prolapse stage II or III were not excluded from the study. This approach was based on the lack of evidence that an isolated repair of the rectocele may affect sling efficacy, as well as on the observation of Yang et al. [26] that anterior colporrhaphy with mesh reinforcement is the only concomitant pelvic surgical procedure that affects the position and motion of the bladder neck or the TOT position. We believe that the study population including such patients is more representative of women encountered in everyday clinical practice.
Conclusions
The highest failure rate of ‘outside-in’ TOT coincides with the location of the tape under the proximal third of the urethra, whereas both the middle and distal sections of the urethra may be regarded as targets for tape placement during this procedure. The distance of the tape from the pubic symphysis and urethral ‘encroachment’ do not seem to affect TOT results.
References
Fong ED, Nitti VW (2010) Review article: mid-urethral synthetic slings for female stress urinary incontinence. BJU Int 106:596–608
Petros PE, Ulmsten UI (1993) An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol Suppl 153:1–93
Ulmsten U, Henricksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J 7:81–86
Cruikshank SH, Kovac SR (1997) The functional anatomy of the urethra: role of the pubourethral ligaments. Am J Obstet Gynecol 176:1200–1203
Kociszewski J, Rautenberg O, Perucchini D, Eberhard J, Geissbühler V, Hilgers R, Viereck V (2008) Tape functionality: sonographic tape characteristics and outcome after TVT incontinence surgery. Neurourol Urodyn 27:485–490
Yang JM, Yang SH, Huang WC (2009) Correlation of morphological alterations and functional impairment of the tension-free vaginal tape obturator procedure. J Urol 181:211–218
Yang JM, Yang SH, Huang WC, Tzeng CR (2012) Correlation of tape location and tension with surgical outcome after transobturator suburethral tape procedures. Ultrasound Obstet Gynecol 39:458–465
Jiang YH, Wang CC, Chuang FC, Ke QS, Kuo HC (2013) Positioning of a suburethral sling at the bladder neck is associated with a higher recurrence rate of stress urinary incontinence. J Ultrasound Med 32:239–245
Westby M, Asmussen M, Ulmsten U (2009) Location of maximum intraurethral pressure related to urogenital diaphragm in the female subject as studied by simultaneous urethrocystometry and voiding urethrocystography. Am J Obstet Gynecol 144:408–412
Kociszewski J, Rautenberg O, Kuszka A, Eberhard J, Hilgers R, Viereck V (2012) Can we place tension-free vaginal tape where it should be? The one-third rule. Ultrasound Obstet Gynecol 39:210–214
Dietz HP, Mouritsen L, Ellis G, Wilson PD (2004) How important is TVT location? Acta Obstet Gynecol Scand 83:904–908
Dietz HP, Wilson PD (2004) The ‘iris effect’: how two-dimensional and three-dimensional ultrasound can help us understand anti-incontinence procedure. Ultrasound Obstet Gynecol 23:267–271
Chantarasorn V, Shek KL, Dietz HP (2011) Sonographic appearance of transobturator slings: implications for function and dysfunction. Int Urogynecol J Pelvic Floor Dysfunct 22:493–498
Chen HY, Yeh LS, Chang WC, Ho M (2007) Analysis of risk factors associated with surgical failure of inside–out transobturator vaginal tape for treating urodynamic stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18:443–447
Lin KL, Juan YS, Lo TS, Liu CM, Tsai EM, Long CY (2012) Three-dimensional ultrasonographic assessment of compression effect on urethra following tension-free vaginal tape and transobturator tape procedures. Ultrasound Obstet Gynecol 39:452–457
Rostaminia G, White DE, Quiroz LH, Shobeiri SA (2013) Visualization of periurethral structures by 3D endovaginal ultrasonography in midsagittal plane is not associated with stress urinary incontinence status. Int Urogynecol J 24:1145–1150
Santoro GA, Wieczorek AP, Stankiewicz A, Woźniak MM, Bogusiewicz M, Rechberger T (2009) High-resolution three-dimensional endovaginal ultrasonography in the assessment of pelvic floor anatomy: a preliminary study. Int Urogynecol J Pelvic Floor Dysfunct 20:1213–1222
Bogusiewicz M, Monist M, Stankiewicz A, Woźniak M, Wieczorek AP, Rechberger T (2013) Most of the patients with suburethral sling failure have tapes located outside the high-pressure zone of the urethra. Ginekol Pol 84:334–3388
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) International urogynecological association; international continence society. An international urogynecological association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct 21:5–26
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 2001(11):1306–1313
Shoukri MM, Pause CA (1999) Statistical methods for health sciences, 2nd edn. CRC Press, Boca Raton. ISBN 0849310954, 9780849310959
Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Bogusiewicz M, Bartuzi A, Miotła P, Skorupski P, Tomaszewski J (2011) Tape fixation: an important surgical step to improve success rate of anti-incontinence surgery. J Urol 18:180–184
Long CY, Hsu CS, Lo TS, Liu CM, Chen YH, Tsai EM (2008) Ultrasonographic assessment of tape location following tension-free vaginal tape and transobturator tape procedure. Acta Obstet Gynecol Scand 87:116–121
Wang F, Song Y, Huang H (2009) Which placement of the tension-free vaginal tape is more important for urinary continence: midurethral position or bladder neck? Consideration from a case report. Int Urogynecol J Pelvic Floor Dysfunct 20:1277–1279
Bogusiewicz M, Rosińska-Bogusiewicz K, Drop A, Rechberger T (2011) Anatomical variation of bony pelvis from the viewpoint of transobturator sling placement for stress urinary incontinence. Int Urogynecol J 22:1005–1009
Yang JM, Yang SH, Huang WC (2008) Dynamic interaction involved in the tension-free vaginal tape obturator procedure. J Urol 180:2081–2087
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
Ethical approval for the study was obtained from the Ethical Committee of Medical University in Lublin (KE-0245/29/2008). All the patients gave their informed consent prior to inclusion in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Bogusiewicz, M., Monist, M., Gałczyński, K. et al. Both the middle and distal sections of the urethra may be regarded as optimal targets for ‘outside-in’ transobturator tape placement. World J Urol 32, 1605–1611 (2014). https://doi.org/10.1007/s00345-014-1261-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-014-1261-1