Abstract
Objectives
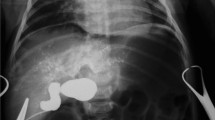
To analyze the ability of magnetic resonance (MR) to identify cystic biliary atresia (CBA) and choledochal cyst (CC).
Methods
Infants (≤ 1 year old) who were diagnosed with CBA or CC type I/IV from January 2010 to July 2023 were retrospectively reviewed. Imaging characteristics on MR were compared between the CBA and CC groups. Binary logistic regression and the area under the receiver operating characteristic curve (AUC) were analyzed for the identification of CBA.
Results
Sixty-three patients with CBA (median age, 30 days) and 172 patients with CC (median age, 60 days) were included. Gallbladder (GB) wall thickness (cutoff, 1.2 mm) showed 98.4% sensitivity and 100% specificity (AUC, 0.998). MR-triangular cord thickness (MR-TCT) (cutoff, 4.1 mm) showed 100% sensitivity and 95.9% specificity (AUC, 0.986). The bile duct loop visualization showed 96.8% sensitivity and 100% specificity (AUC, 0.984). Proximal bile duct (PBD) diameter (cutoff, 1.3 mm) showed 92.1% sensitivity and 95.3% specificity (AUC, 0.977). Cyst wall thickness (cutoff, 1 mm) showed 77.8% sensitivity and 95.3% specificity (AUC, 0.942). The combination of GB wall thickness > 1.2 mm and MR-TCT > 4.1 mm, GB wall thickness > 1.2 mm and loop visualization, GB wall thickness > 1.2 mm, and cyst wall thickness > 1 mm showed 100% sensitivity and 100% specificity (AUC, 1.000).
Conclusions
Imaging characteristics on MR might be used to identify CBA and CC, and the combination of GB wall thickness and MR-TCT, or loop visualization, or cyst wall thickness, has a perfect diagnostic value.
Clinical relevance statement
Early and accurate differentiation of CBA and CC is essential, but current methods rely on inherently subjective ultrasound. Biliary features on MRI allow for an objective, accurate diagnosis.
Key Points
-
Cystic biliary atresia and choledochal cysts have similar clinical presentations, but require different treatments at different ages.
-
Examined MR features eliminate ultrasound related subjectivity and diagnose cystic biliary atresia with nearly perfect accuracy.
-
Early and accurate differentiation between these entities allows for timely life-saving intervention.






Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the ROC curve
- BA:
-
Biliary atresia
- CBA:
-
Cystic biliary atresia
- CC:
-
Choledochal cyst
- GB:
-
Gallbladder
- MPR:
-
Multiplanar reconstruction
- MR:
-
Magnetic resonance
- MRCP:
-
Magnetic resonance cholangiopancreatography
- ROC:
-
Receiver operating characteristic
- TC:
-
Triangular cord
- TCT:
-
Triangular cord thickness
References
Verkade HJ, Bezerra J, Davenport M et al (2016) Biliary atresia and other cholestatic childhood diseases: advances and future challenges. J Hepatol 65:631–642
Nio M, Sasaki H, Wada M, Kazama T, Nishi K, Tanaka H (2010) Impact of age at Kasai operation on short- and long-term outcomes of type III biliary atresia at a single institution. J Pediatr Surg 45:2361–2363
Pakarinen MP, Johansen LS, Svensson JF et al (2018) Outcomes of biliary atresia in the nordic countries- a mulitcenter study of 158 patients during 2005–2016. J Pediatr Surg 53:1509–1515
Fanna M, Masson G, Capito C et al (2019) Management of biliary atresia in France 1986–2015: long-term results. J Pediatr Gastroenterol Nutr 69:416–424
Lobeck IN, Sheridan R, Lovell M, Dupree P, Tiao GM, Bove KE (2017) Cystic biliary atresia and choledochal cysts are distinct histopathologic entities. Am J Surg Pathol 41:354–364
Arora A, Patidar Y, Khanna R, Alam S, Rastogi A, Negi SS (2012) Cystic biliary atresia: confounding and intriguing. J Pediatr 161:562
Caponcelli E, Knisely AS, Davenport M (2008) Cystic biliary atresia: an etiologic and prognostic subgroup. J Pediatr Surg 43:1619–1624
Ten Hove A, de Meijer VE, Hulscher JBF, de Kleine RHJ (2018) Meta-analysis of risk of developing malignancy in congenital choledochal malformation. Br J Surg 105:482–490
Farooq MA, Khan SA, Malik MI (2023) Choledochal Cyst in Children, presentation and outcome - 10 years’ experience from a tertiary care center in Pakistan. Pak J Med Sci 39:456–459
Tannuri ACA, Hara LAA, Paganoti GF, Andrade WC, Tannuri U (2020) Choledochal cysts in children: How to diagnose and operate on. Clinics 75:e1539
Zhou LY, Wang W, Shan QY et al (2015) Optimizing the US diagnosis of biliary atresia with a modified triangular cord thickness and gallbladder classification. Radiology 277:181–191
Chen YT, Gao MJ, Zheng ZB et al (2022) Comparative analysis of cystic biliary atresia and choledochal cysts. Front Pediatr 10:947876
Chen L, He F, Zeng K et al (2022) Differentiation of cystic biliary atresia and choledochal cysts using prenatal ultrasonography. Ultrasonography 41:140–149
Koob M, Pariente D, Habes D, Ducot B, Adamsbaum C, Franchi-Abella S (2017) The porta hepatis microcyst: an additional sonographic sign for the diagnosis of biliary atresia. Eur Radiol 27:1812–1821
Yu P, Dong N, Pan YK, Li L (2021) Ultrasonography is useful in differentiating between cystic biliary atresia and choledochal cyst. Pediatr Surg Int 37:731–736
Zhou LY, Guan BY, Li L et al (2012) Objective differential characteristics of cystic biliary atresia and choledochal cysts in neonates and young infants: sonographic findings. J Ultras Med 31:833–841
Kim YH, Kim MJ, Shin HJ et al (2018) MRI-based decision tree model for diagnosis of biliary atresia. Eur Radiol 28:3422–3431
Shin HJ, Yoon H, Han SJ et al (2021) Key imaging features for differentiating cystic biliary atresia from choledochal cyst: prenatal ultrasonography and postnatal ultrasonography and MRI. Ultrasonography 40:301–311
Han SJ, Kim MJ, Han A et al (2002) Magnetic resonance cholangiography for the diagnosis of biliary atresia. J Pediatr Surg 37:599–604
Liu B, Cai J, Xu Y et al (2014) Three-dimensional magnetic resonance cholangiopancreatography for the diagnosis of biliary atresia in infants and neonates. PLoS One 9:e88268
Sung S, Jeon TY, Yoo SY et al (2016) Incremental value of MR cholangiopancreatography in diagnosis of biliary atresia. PLoS One 11:e0158132
Siles P, Aschero A, Gorincour G et al (2014) A prospective pilot study: can the biliary tree be visualized in children younger than 3 months on magnetic resonance cholangiopancreatography? Pediatr Radiol 44:1077–1084
Ni Y, Lukito G, Marchal G et al (1994) Potential role of bile duct collaterals in the recovery of the biliary obstruction: experimental study in rats using microcholangiography, histology, serology and magnetic resonance imaging. Hepatology 20:1557–1566
Vartak N, Damle-Vartak A, Richter B et al (2016) Cholestasis-induced adaptive remodeling of interlobular bile ducts. Hepatology 63:951–964
Russo P, Magee JC, Anders RA et al (2016) Key histopathologic features of liver biopsies that distinguish biliary atresia from other causes of infantile cholestasis and their correlation with outcome: a multicenter study. Am J Surg Pathol 40:1601–1615
Lv WJ, Zhao XY, Hu DD, Xin XH, Qin LL, Hu CH (2021) Insight into bile duct reaction to obstruction from a three-dimensional perspective using ex vivo phase-contrast CT. Radiology 299:597–610
Qi BN, Lv WJ, Jian JB et al (2023) Insight into microvascular adaptive alterations in the Glisson system of biliary atresia after Kasai portoenterostomy using X-ray phase-contrast CT. Eur Radiol 33:4082–4093
Slott PA, Liu MH, Tavoloni N (1990) Origin, pattern, and mechanism of bile duct proliferation following biliary obstruction in the rat. Gastroenterology 99:466–477
Kotb MA, Kotb A, Sheba MF et al (2001) Evaluation of the triangular cord sign in the diagnosis of biliary atresia. Pediatrics 108:416–420
Lee HJ, Lee SM, Park WH, Choi SO (2003) Objective criteria of triangular cord sign in biliary atresia on US scans. Radiology 229:395–400
Suzuki T, Hashimoto T, Hussein MH, Hara F, Hibi M, Kato T (2013) Biliary atresia type I cyst and choledochal cyst [corrected]: can we differentiate or not? J Hepatobiliary Pancreat Sci 20:465–470
Tang J, Zhang D, Liu W, Zeng JX, Yu JK, Gao Y (2018) Differentiation between cystic biliary atresia and choledochal cyst: a retrospective analysis. J Paediatr Child Health 54:383–389
Huang FC, Hwang KP (2006) Differential diagnosis of infantile choledochal cyst with or without biliary atresia. Acta Paediatr Taiwan 47:175–180
Hasegawa T, Sasaki T, Kimura T et al (2002) Prenatal ultrasonographic appearance of type IIId (uncorrectable type with cystic dilatation) biliary atresia. Pediatr Surg Int 18:425–428
Koukoura O, Kelesidou V, Delianidou M, Athanasiadis A, Dagklis T (2019) Prenatal sonographic diagnosis of biliary tract malformations. J Clin Ultrasound 47:292–297
Kim WS, Kim IO, Yeon KM, Park KW, Seo JK, Kim CJ (1998) Choledochal cyst with or without biliary atresia in neonates and young infants: US differentiation. Radiology 209:465–469
Hartley JL, Davenport M, Kelly DA (2009) Biliary atresia. Lancet 374:1704–1713
Choochuen P, Kritsaneepaiboon S, Charoonratana V, Sangkhathat S (2019) Is “gallbladder length-to-width ratio” useful in diagnosing biliary atresia? J Pediatr Surg 54:1946–1952
Narkewicz MR (2001) Biliary atresia: an update on our understanding of the disorder. Curr Opin Pediatr 13:435–440
Funding
This study has received funding from the project of Guangzhou Municipal Science and Technology Bureau (Grant No. 2024A03J1008).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr Hongsheng Liu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
The study subjects or cohorts have not been reported.
Methodology
-
Retrospective
-
Diagnostic study
-
Performed at one institution
Additional information
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
He, F., Guan, X., Yang, B. et al. Key postnatal magnetic resonance characteristics for differentiating cystic biliary atresia from choledochal cyst. Eur Radiol (2024). https://doi.org/10.1007/s00330-024-10753-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-024-10753-0