Abstract
Objectives
To evaluate the methodological quality and diagnostic accuracy of MRI-based radiomic studies predicting O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation status in gliomas.
Methods
PubMed Medline, EMBASE, and Web of Science were searched to identify MRI-based radiomic studies on MGMT methylation in gliomas published until December 31, 2022. Three raters evaluated the study methodological quality with Radiomics Quality Score (RQS, 16 components) and Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis Or Diagnosis (TRIPOD, 22 items) scales. Risk of bias and applicability concerns were assessed with QUADAS-2 tool. A meta-analysis was performed to estimate the pooled area under the curve (AUC) and to assess inter-study heterogeneity.
Results
We included 26 studies, published from 2016. The median RQS total score was 8 out of 36 (22%, range 8–44%). Thirteen studies performed external validation. All studies reported AUC or accuracy, but only 4 (15%) performed calibration and decision curve analysis. No studies performed phantom analysis, cost-effectiveness analysis, and prospective validation. The overall TRIPOD adherence score was between 50% and 70% in 16 studies and below 50% in 10 studies. The pooled AUC was 0.78 (95% CI, 0.73–0.83, I2 = 94.1%) with a high inter-study heterogeneity. Studies with external validation and including only WHO-grade IV gliomas had significantly lower AUC values (0.65; 95% CI, 0.57–0.73, p < 0.01).
Conclusions
Study RQS and adherence to TRIPOD guidelines was generally low. Radiomic prediction of MGMT methylation status showed great heterogeneity of results and lower performances in grade IV gliomas, which hinders its current implementation in clinical practice.
Clinical relevance statement
MGMT promoter methylation status appears to be variably correlated with MRI radiomic features; radiomic models are not sufficiently robust to be integrated into clinical practice to accurately predict MGMT promoter methylation status in patients with glioma before surgery.
Key Points
• Adherence to the indications of TRIPOD guidelines was generally low, as was RQS total score.
• MGMT promoter methylation status prediction with MRI radiomic features provided heterogeneous diagnostic accuracy results across studies.
• Studies that included grade IV glioma only and performed external validation had significantly lower diagnostic accuracy than others.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gliomas are the most common primary malignant brain tumors in adults, with a median age of onset of approximately 55 to 60 years [1]. In high-grade gliomas, the use of temozolomide after gross total resection represents first-line medical therapy associated to radiation therapy [2, 3]. Among all identified glioma genetic alterations, O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation is an important prognostic molecular marker in clinical settings[4].
The MGMT normally protects cells against the damage of alkylating agents [5] such as temozolomide, and therefore its inhibited expression through methylation is related to a better prognosis during standard-of-care chemotherapy for glioblastoma [2, 6, 7]. Indeed, MGMT methylation is associated with better survival, especially for patients with higher extent of MGMT methylation [8].
In a minority of patients, surgical resection is not possible (due to concomitant pathologies or old age) or tests for MGMT methylation are unsuccessful due to tissue insufficiency, especially for those undergoing stereotaxic biopsy. Therefore, the opportunity to determine MGMT methylation status through imaging without surgical intervention would be of great utility for patient management.
Several prior studies tried to correlate MRI data with MGMT methylation status, based on visual assessment of experienced radiologists. Results of these works were not always consistent, with alternate conclusions [9, 10]. The introduction of machine-learning methods based on the extraction of radiomic features has revitalized the debate [11, 12].
Radiomics is a research field that exploits the increased computing capabilities that have become available over the last few decades to extract and analyze thousands of quantitative biomarkers from radiological images [13]. Many research groups have been investigating the correlation of radiomic features with MGMT methylation status. Their findings vary greatly ranging from very promising predictive values [14] to disappointing results [15].
Radiomic studies have great variability in their methodological pipelines, which can impact the reproducibility and generalizability of results. In this context, the Image Biomarkers Standardization Initiative (IBSI) represents an international effort to provide standardized procedures for image processing and radiomic features calculation [16]. One of the methodological studies aiming to provide specific recommendations for reporting radiomic models is the Radiomics Quality Score (RQS) [17]. This tool proposes a standardized evaluation of the performance, reproducibility, and clinical utility of radiomic studies by assessing compliance not only with feature extraction but also with model development and validation. The RQS has been already applied to evaluate the methodological quality of radiomic studies for several oncological diseases such as meningiomas, gliomas, metastases, and other neoplasms [18,19,20,21].
This review aimed to evaluate the quality of prior studies on predicting MGMT methylation status in gliomas based on MRI-radiomic features, using the RQS items. We also assessed the studies using the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis Or Diagnosis (TRIPOD) guideline [22], a commonly used standard for reporting studies that develop and/or validate prediction models. Furthermore, we conducted a meta-analysis to quantitatively investigate the association between study quality and diagnostic accuracy while accounting for the heterogeneity of the included studies.
Materials and methods
This study presents a systematic review of the literature and a meta-analysis conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement. Ethical committee approval was waived due to the nature of the study.
Eligibility criteria
Studies were included if the following criteria were met: (1) aimed to predict MGMT methylation status using any MRI sequence; (2) used radiomic features as input for classification; (3) included patients with glioma of any WHO grade (I to IV, as defined according to the 2016 edition of the WHO central nervous system tumor classification [23]). Studies were excluded if (1) they were case reports, correlation studies, commentaries, conference abstracts, editorials, letters, and review articles, or (2) radiomic features did not encompass texture features as defined according to IBSI guidelines.
Search strategy and study selection
We performed a systematic search in PubMed Medline, EMBASE, and Web of Science databases to identify any published study until 31 December 2022, using the following query: (glioma OR glioblastoma) AND (MGMT OR ‘Methylguanine methyltransferase’) AND (radiomic OR radiogenomic OR texture).
First, duplicated studies were removed. Then, studies were independently screened by three authors (F.M.D. and M.M. with 7 years and R.P. with 8 years of experience in neuroimaging research), first reviewing the titles and abstracts to determine whether they met exclusion criteria and should be removed. Studies found to be not eligible after title and abstract screening were excluded. Next, a full text review of the identified studies was performed to determine the final list of included studies. Disagreements were resolved by consensus.
Data extraction
In a spreadsheet, we collected data on the number of patients included, WHO grade of tumors, additional molecular markers explored, number of MRI scanners, MRI sequences, number and type of tumor compartments segmented and considered for feature extraction (e.g., only contrast-enhancing areas, necrotic areas, T2/FLAIR hyperintense areas), number of extracted features, and methods for feature extraction and classification, as well as classification performances (i.e., area under the curve [AUC], accuracy).
Quality assessment
We evaluated the methodological quality of the included studies based on the RQS and TRIPOD guidelines. Our focus was only for the MGMT prediction task and not for other tasks potentially performed in the same study. In addition, risk of bias and applicability concerns were assessed using the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2), one of the most recommended tools for evaluating such risks in systematic reviews on diagnostic accuracy studies [24]. Details about QUADAS-2 are illustrated in the Supplementary Methods.
RQS
Two reviewers (F.M.D. and R.P.) achieved consensus on the evaluation criteria of RQS by discussion and independently evaluated the included studies by scoring each RQS item. Disagreements on the scores assigned to the studies were resolved by discussion and consensus or else by a third reviewer (M.M.) to avoid a potentially low inter-rater reproducibility as highlighted by recent evidence [25]. Next, we classified the 16 components of RQS into six domains, in line with previous studies [18, 19, 26, 27], and calculated the cumulative score for each domain of the RQS and overall. Table 1 reports the RQS components grouped by domain, with range of attainable points.
TRIPOD
Two reviewers (F.M. and F.P.) achieved consensus on the evaluation criteria of TRIPOD by discussion and independently evaluated the included studies by scoring each TRIPOD item. Disagreements were resolved by discussion and consensus or else by a third reviewer (M.M.). A total TRIPOD adherence score was calculated for each study by summing the adhered and applicable TRIPOD items. Overall adherence per TRIPOD item was calculated by dividing the number of studies that adhered to a specific TRIPOD item by the number of studies in which the specific TRIPOD item was applicable [22].
Statistical analysis
The measured endpoint was the AUC of each study obtained from models based only on radiomics (excluding clinical data). Of note, only studies that reported a measure of uncertainty of their AUC (either standard deviations or 95% confidence intervals [CIs]) were included in the meta-analysis. Authors of studies that did not report such information in their publications were contacted via email to ask for these missing data. Pooled results with corresponding 95% CIs were derived using the random effects model based on restricted maximum likelihood estimator [28, 29]. The heterogeneity of individual studies was estimated with Cochran’s Q test and I2 value. Sources of heterogeneity among studies were identified by performing subgroup analyses and meta-regression, considering the combination of the following two factors: (1) external validation was performed; (2) patients with only WHO-grade IV were included. Publication bias was assessed by funnel plot and Egger’s test [30]. The statistical analyses were performed using R (version 4.2.1) and, in particular, the “metafor” R package [31].
Results
We identified 101 studies, of which 26 met the inclusion criteria (Fig. 1, Table 2) [11, 12, 14, 15, 32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53]. These studies included a median of 116 patients (min 34; max 418). The majority (15/26, 58%) focused on patients with WHO grade IV gliomas, and the others included patients with heterogeneous WHO grades gliomas (from I to IV, or only II and III). Other information related to image and radiomic workflow is shown in Supplementary Table 1.
RQS assessment
Results of the RQS assessment for the 26 included studies are summarized in Table 3 and shown in Fig. 2. The median total score was 8 (22%), ranging between 3 (8%) and 16 (44%), from the maximum RQS score of 36 (100%).
Summary of radiomics quality scores (RQS) assessment results of the 26 included studies per domain. Each row of the plot shows the distribution of the scores achieved by the studies for a domain. Colors from red to green denote progressive increase from minimum to maximum score obtainable for each item. Abbreviations: RQS, Radiomics Quality Score
In domain 1, most studies (23/26, 88%) provided a sufficiently detailed description of the image protocol, and only four (15%) used a public protocol. Multiple segmentations by different physicians were done in twelve studies (46%). Phantom studies were never conducted.
In domain 2, all studies but two (92%) performed feature selection. Thirteen out of 26 studies (50%) performed validation without retraining the proposed model (seven based on a dataset of the same institute, and six using an external dataset), and the remaining 13 (50%) did not validate the trained model on a separate dataset.
In domain 3, the majority of studies (15/26, 58%) performed multivariable analysis with non-radiomic features. Biological correlates were discussed in 13 out of 26 (50%) studies. Comparison to gold standard was done in all included studies. Of note, we considered “gold standard” several types of MGMT methylation status analysis, as there is no consensus on the best assay to use [54] and high variability between threshold of MGMT methylation values [55]. Only four studies (15%) performed quantitative analysis (e.g., decision curve analysis) to report on the potential clinical utility.
In domain 4, all studies reported discrimination statistics (AUC or accuracy) along with their statistical significance (p values or confidence intervals) and most of them (19/26, 73%) computed those statistics using a resampling method (e.g., bootstrapping, cross-validation); some performed also cut-off analysis (12/26, 46%). In contrast, only two studies (8%) reported calibration statistics.
In domain 5, all studies had a retrospective design; no study performed a prospective validation of the radiomics signature in an appropriate trial, nor a cost-effectiveness analysis.
In domain 6, only four studies had open-source scans (15%) and three of them used also open-source segmentations of regions of interest [56].
We did not observe a remarkable difference in RQS scores when comparing more recent studies to past works (Supplementary Figure 1).
TRIPOD assessment
The adherence to all TRIPOD items is reported in Supplementary Table 2 for each study. The median total score was 15.5 (range 10–23). The 26 studies met between 31% and 68% of the TRIPOD items, considering only the applicable items. TRIPOD items from the background, study design, eligibility criteria, outcome assessment blinding, definition and handling of the predictors, model development, limitations, and interpretation were reported in more than 80% of the studies (Table 4). Lower percentages (between 60% and 80%) of adherence to items related to key study dates and setting, times and methods of outcome definition, blinding of the predictors’ assessment, and implications were obtained. Instead, other TRIPOD items from title and abstract, sample size, statistical analysis methods, participants, model specification and performance, and supplementary information were reported in less than 30% of the studies. No study performed model updating.
We did not observe a remarkable difference in TRIPOD scores when comparing more recent studies to past works (Supplementary Figure 1).
QUADAS-2 assessment
Results of the QUADAS-2 assessment are illustrated in Supplementary Figure 2 and reported in detail in the Supplementary Results. Briefly, overall risk of bias was low in 10 studies, unclear in one, and high in 15; as for the applicability concern related to the present review question, it was low in all but one of the studies.
Classification accuracy and methodology quality
In total, 13 studies provided sufficient information in the text to compute the pooled AUC. As for the other 13, only three provided such missing data following our email request [32, 35, 42]. Therefore, 16 studies were considered for meta-analysis. However, we found that two studies [40, 41] included the same cohort of patients recruited in the same center during the same period, and therefore only one of these two studies (the one with the highest number of patients) was finally incorporated in the meta-analysis [40] . The pooled AUC of the 15 studies was estimated to be equal to 0.778 (95% CI 0.728–0.830, I2 = 94.08%) (Fig. 3). Subgroup analysis indicated that studies with external validation and including only patients with WHO-grade IV tumors had AUC values significantly lower (0.647, 95% CI 0.569–0.726, I2 = 0%) than others (test for subgroup differences: χ2 = 14.04, df = 3, p = 0.0029) (Fig. 4). A meta-regression model of the AUCs based on predictors such as RQS and TRIPOD total scores was not globally significant (χ2 = 0.8506, df = 2, p = 0.6536). After excluding each study one at the time and recomputing the pooled AUC, there was no study that contributed significantly to the heterogeneity observed in this sample (Supplementary Figure 3). Publication bias was absent according to visual inspection of the funnel plot which did not suggest substantial asymmetry (Supplementary Figure 4), as confirmed also by Egger’s test (t = −0.15, df = 13, p = 0.8823).
Forest plots with the results of the subgroup analysis. Studies were grouped based on the combination of two factors: (1) whether an external validation was performed; (2) whether WHO-grade IV glioma were only included in their analysis. Abbreviations: AUC, area under the curve; SE, standard error; CI, confidence interval
Of note, the above results were obtained with models based on radiomic features only. There were 13 out of 26 studies investigating multivariable models integrating radiomic with non-radiomic features and comparing AUCs with models based only on radiomics: in seven of them [11, 12, 37, 40, 46, 47, 50], non-radiomic features were not selected by the algorithm and therefore they did not improve model accuracy; in other four studies, AUC values increased when the model included non-radiomic features, such as other radiological features of the images [39], Visually AcceSAble Rembrandt Images (VASARI) features [45, 49], fractal features [48], or prediction results obtained by a multi-label classification model [15]; in the remaining two studies, AUC values were lower when age [42] or apparent diffusion coefficient values of tumor/edema areas [51] were included in a multivariate model.
Discussion
We reviewed 26 studies aiming to predict MGMT promoter methylation in patients with glioma based on MRI-radiomic features. We analyzed the adherence of these studies to the RQS and TRIPOD guidelines, finding generally unsatisfactory results for the two scales and heterogeneous classification performances. We performed a meta-analysis on the classification performances obtaining a pooled AUC of 0.78 and finding significantly lower AUC value (0.65) for studies performing external validation only on grade IV gliomas.
RQS assessment
In our review, the median total RQS score of the analyzed studies was globally low (8/36 points, 22%), in agreement with other methodological reviews of radiomic studies [18,19,20, 26, 27, 57].
Regarding the specific RQS domains, most studies complied with domain 3 (biologic/clinical validation and utility), where 19 out of 26 studies obtained at least a score of 3 out of 6. However, a perfect score in this domain was rarely achieved due to the lack of a decision curve analysis. Such analysis enables estimation of the clinical net benefit achievable by the prediction/diagnostic model, although it is rarely performed in medical literature [58]. It should also be noted that this tool is often misused in literature, even though it can still provide useful insights [59].
Referring to domain 1 (protocol quality and stability in image and segmentation), less than half of the analyzed studies (12/26) did multiple segmentations: this item is very time-consuming, but it increases the reproducibility of the results [17, 60].
In domain 4 (model performance index), all studies performed discrimination analysis reporting an appropriate accuracy metric and most of them also used resampling techniques (bootstrap or cross-validation) to reduce the overfitting issue. However, calibration (which measures the agreement between the probability of being classified as positive and the true underlying risk of being positive) was rarely conducted, probably because this analysis is not commonly performed outside the machine learning community. Future radiomic studies should also consider this analysis when individual predictions are made and used to support clinical decision-making.
As reported by previous works [18, 26], the RQS is inherently inferior in retrospective and radio-genomic correlation studies, such as those included in this review. They inevitably performed poorly in domain 5 (high level of evidence), in which 7 out of 36 total points are attributed if the study is prospective. Moreover, apart from studies that used large public databases [12, 14, 48], no work shared their images, obtaining low scores in domain 6 (open science and data). Therefore, 11 RQS points out of 36 coming from domains 5 and 6 were difficult to attribute, suggesting that some RQS items may be too strict for most studies as recently highlighted [61].
In domain 2 (feature selection and validation), almost all studies performed a feature reduction step. However, half of them did not perform the validation step (−5 points), because they did not test the final model on a separate dataset. This has serious implications on the classification performance of the models.
Classification performance
Unsurprisingly, studies without external validation performed better than those with a separate test set, according to our meta-analysis. Indeed, machine learning methods are prone to overfitting to the trained dataset, especially when a feature selection step is performed before training the model [62]. This is the reason why most recommended guidelines such as TRIPOD [22] and RQS require a step of external validation after developing the prediction model [60]. Without this step, it is impossible to reach generalizable results. Therefore, results of studies suffering from this issue should be interpreted carefully.
Our meta-analysis proved that MGMT promoter methylation prediction was less accurate when considering a homogeneous cohort of patients with grade IV gliomas only, whose radiological characteristics are similar. In other words, radiomic models considering heterogeneous glioma grades perform better because they may be influenced by the different levels of MGMT promoter methylation between lower- and higher-grade gliomas [63].
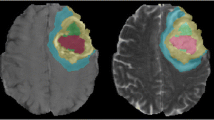
Other sources of variability may be found in the different choices of tumor segmentation. Although specific tumor compartments were identified in 19 studies (as shown in Supplementary Table 1), they were not standardized across studies and therefore subgroup analysis was not possible. Moreover, the indication of contouring the “whole tumor” made by some studies was not always sufficiently specific to understand the precise extension of the tumor considered (i.e., if edema or necrosis was included). Future studies should provide more details of the tumor compartments considered (possibly illustrating representative examples) and are encouraged to develop separate radiomic models on each compartment as well as on their union to increase comparability and reproducibility across studies.
Further sources of variability were identified in the sequences used to extract radiomic features. Only a small number (5 out of 26) of studies used public databases, while the majority relied on retrospective data collected in single centers, which demonstrated a substantial heterogeneity. For instance, only 6 studies employed 3D-T1-weighted imaging sequences post-contrast, while 13 and 18 studies made use of 2D-T1-weighted imaging sequences without and with contrast, respectively; there were 14 studies considering 2D-T2-weighted imaging sequences and only 2 employing 3D-T2-weighted imaging sequences. This substantial heterogeneity of the conventional sequences markedly diminishes the generalizability of the findings. Standardizing the sequences across various centers (including prospective studies) and enlarging the number of cases in public databases can alleviate this variability.
Our review relied on conventional radiomic studies involving hand-crafted features, which offer a potentially high level of interpretability and may be appropriate for relatively small datasets, such as those commonly gathered in neuro-oncological research. On the other hand, deep-learning techniques are increasingly being employed to automatically extract radiomic features that have the potential to capture complex, high-dimensional patterns within the data. However, more recent studies using deep-learning radiomics to predict MGMT promoter methylation status reported heterogeneous results, obtaining high [33, 64] and low [65] classification performances. Thus, it appears that deep-learning studies may also be affected by comparable concerns as those identified in this review. However, further evidence is required to conduct a more thorough investigation of this matter.
Risk of bias
Most of the included studies had high or unclear risk of bias (16/26), as estimated through QUADAS-2 tool: this was partially in agreement with the results of the RQS and TRIPOD, which indicated even lower methodological quality overall. This is because RQS and TRIPOD examine the issues related to several methodological choices in greater depth and specificity than QUADAS-2 for studies that develop radiomic and prediction models.
Limitations
One limitation of this study was that only papers written in English were included. Moreover, gray literature was not incorporated; nevertheless, we believe the included studies provided a comprehensive representation of the literature, as we found no evidence of publication bias (Supplementary Figure 4). Another limitation was that certain studies included in the systematic review did not report AUC values with uncertainty measures, and consequently could not be included in the meta-analysis.
Conclusions
Adherence of the published articles to RQS items or the indications of TRIPOD was generally low. Radiomic models do not provide accurate predictions of the MGMT promoter methylation status in grade IV gliomas. Therefore, to date, they are not ready to be integrated into clinical practice. Future studies aiming to predict MGMT promoter methylation status with radiomics should include homogeneous cohorts of glioblastoma patients and have a sufficiently large number of cases to permit a proper external validation; adherence to current reporting guidelines and radiomic pipelines (such as RQS, TRIPOD, and CLEAR [17, 22, 61]) should also be increased to improve quality, reliability, and, therefore, inter-study comparability.
Abbreviations
- AUC:
-
Area Under the Curve
- IBSI:
-
Image Biomarker Standardization Initiative
- MGMT:
-
O6-Methylguanine-DNA methyltransferase
- QUADAS-2:
-
Quality Assessment of Diagnostic Accuracy Studies 2
- RQS:
-
Radiomics Quality Score
- TRIPOD:
-
Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis Or Diagnosis
References
Ostrom QT, Cioffi G, Gittleman H et al (2019) CBTRUS Statistical Report: primary brain and other central nervous system tumors diagnosed in the United States in 2012–2016. Neuro Oncol 21:v1–v100. https://doi.org/10.1093/neuonc/noz150
Stupp R, Taillibert S, Kanner A et al (2017) Effect of tumor-treating fields plus maintenance temozolomide vs maintenance temozolomide alone on survival in patients with glioblastoma a randomized clinical trial. JAMA 318:2306–2316. https://doi.org/10.1001/jama.2017.18718
Stupp R, Mason WP, Van Den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. https://doi.org/10.1056/NEJMoa043330
Weller M, Stupp R, Reifenberger G et al (2010) MGMT promoter methylation in malignant gliomas: ready for personalized medicine? Nat Rev Neurol 6:39–51. https://doi.org/10.1038/nrneurol.2009.197
Esteller M, Hamilton SR, Burger PC et al (1999) Inactivation of the DNA repair gene O6-methylguanine-DNA methyltransferase by promoter hypermethylation is a common event in primary human neoplasia. Cancer Res 59:793–7
Johnson DR, O’Neill BP (2012) Glioblastoma survival in the United States before and during the temozolomide era. J Neurooncol 107:359–364. https://doi.org/10.1007/s11060-011-0749-4
Hegi ME, Diserens A-C, Gorlia T et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003. https://doi.org/10.1056/nejmoa043331
Poon MTC, Keni S, Vimalan V et al (2021) Extent of MGMT promoter methylation modifies the effect of temozolomide on overall survival in patients with glioblastoma: a regional cohort study. Neurooncol Adv 3:1–10. https://doi.org/10.1093/noajnl/vdab171
Eoli M, Menghi F, Bruzzone MG et al (2007) Methylation of O6-methylguanine DNA methytransferase and loss of heterozygosity on 19q and/or 17p are overlapping features of secondary glioblastomas with prolonged survival. Clin Cancer Res 13:2606–2613. https://doi.org/10.1158/1078-0432.CCR-06-2184
Bruzzone MG, Eoli M, Cuccarini V et al (2009) Genetic signature of adult gliomas and correlation with MRI features. Expert Rev Mol Diagn 9:709–720. https://doi.org/10.1586/erm.09.44
Korfiatis P, Kline TL, Coufalova L et al (2016) MRI texture features as biomarkers to predict MGMT methylation status in glioblastomas. Med Phys 43:2835–2844. https://doi.org/10.1118/1.4948668
Li ZC, Bai H, Sun Q et al (2018) Multiregional radiomics features from multiparametric MRI for prediction of MGMT methylation status in glioblastoma multiforme: a multicentre study. Eur Radiol 28:3640–3650. https://doi.org/10.1007/s00330-017-5302-1
Lotan E, Jain R, Razavian N et al (2019) State of the art: machine learning applications in glioma imaging. AJR Am J Roentgenol 212:26–37. https://doi.org/10.2214/AJR.18.20218
Le NQK, Do DT, Chiu FY et al (2020) XGBoost improves classification of MGMT promoter methylation status in IDH1 wildtype glioblastoma. J Pers Med 10:1–13. https://doi.org/10.3390/jpm10030128
Sohn B, An C, Kim D et al (2021) Radiomics-based prediction of multiple gene alteration incorporating mutual genetic information in glioblastoma and grade 4 astrocytoma, IDH-mutant. J Neurooncol 155:267–276. https://doi.org/10.1007/s11060-021-03870-z
Zwanenburg A, Vallières M, Abdalah MA et al (2020) The image biomarker standardization initiative: standardized quantitative radiomics for high-throughput image-based phenotyping. Radiology 295:328–338. https://doi.org/10.1148/radiol.2020191145
Lambin P, Leijenaar RTH, Deist TM et al (2017) Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol 14:749–762. https://doi.org/10.1038/nrclinonc.2017.141
Won SY, Park YW, Ahn SS et al (2021) Quality assessment of meningioma radiomics studies: bridging the gap between exploratory research and clinical applications. Eur J Radiol 138:109673. https://doi.org/10.1016/j.ejrad.2021.109673
Park JE, Kim D, Kim HS et al (2020) Quality of science and reporting of radiomics in oncologic studies: room for improvement according to radiomics quality score and TRIPOD statement. Eur Radiol 30:523–536. https://doi.org/10.1007/S00330-019-06360-Z
Sanduleanu S, Woodruff HC, de Jong EEC et al (2018) Tracking tumor biology with radiomics: a systematic review utilizing a radiomics quality score. Radiother Oncol 127:349–360. https://doi.org/10.1016/J.RADONC.2018.03.033
Spadarella G, Stanzione A, AkinciD’Antonoli T et al (2023) Systematic review of the radiomics quality score applications: an EuSoMII Radiomics Auditing Group Initiative. Eur Radiol 33:1884–1894. https://doi.org/10.1007/s00330-022-09187-3
Collins GS, Reitsma JB, Altman DG, Moons KGM (2015) Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis Or Diagnosis (TRIPOD): the TRIPOD statement. J Clin Epidemiol 68:112–121. https://doi.org/10.1016/j.jclinepi.2014.11.010
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Whiting PF (2011) QUADAS-2: a revised tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann Intern Med 155:529. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Akinci D’Antonoli T, Cavallo AU, Vernuccio F et al (2023) Reproducibility of radiomics quality score: an intra- and inter-rater reliability study. Eur Radiol. https://doi.org/10.1007/s00330-023-10217-x
Park JE, Kim HS, Kim D et al (2020) A systematic review reporting quality of radiomics research in neuro-oncology: toward clinical utility and quality improvement using high-dimensional imaging features. BMC Cancer 20:29. https://doi.org/10.1186/s12885-019-6504-5
Won SY, Park YW, Park M et al (2020) Quality reporting of radiomics analysis in mild cognitive impairment and Alzheimer’s disease: a roadmap for moving forward. Korean J Radiol 21:1345–1354. https://doi.org/10.3348/kjr.2020.0715
Raudenbush SW (2009) Analyzing effect sizes: random effects models. The handbook of research synthesis and meta-analysis, 2nd edn. Russell Sage Foundation, New York, pp 295–315
Viechtbauer W (2005) Bias and efficiency of meta-analytic variance estimators in the random-effects model on JSTOR. In: J Educ Behav Stat. https://www.jstor.org/stable/3701379. Accessed 13 Jul 2023
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor Package. J Stat Softw 36:1–48. https://doi.org/10.18637/jss.v036.i03
Calabrese E, Rudie JD, Rauschecker AM et al (2022) Combining radiomics and deep convolutional neural network features from preoperative MRI for predicting clinically relevant genetic biomarkers in glioblastoma. Neurooncol Adv 4:1–11. https://doi.org/10.1093/noajnl/vdac060
Chen S, Xu Y, Ye M et al (2022) Predicting MGMT promoter methylation in diffuse gliomas using deep learning with radiomics. J Clin Med 11:3445. https://doi.org/10.3390/jcm11123445
Crisi G, Filice S (2020) Predicting MGMT promoter methylation of glioblastoma from dynamic susceptibility contrast perfusion: a radiomic approach. J Neuroimaging 30:458–462. https://doi.org/10.1111/jon.12724
Do DT, Yang MR, Lam LHT et al (2022) Improving MGMT methylation status prediction of glioblastoma through optimizing radiomics features using genetic algorithm-based machine learning approach. Sci Rep 12:1–12. https://doi.org/10.1038/s41598-022-17707-w
Hajianfar G, Shiri I, Maleki H et al (2019) Noninvasive O6 methylguanine-DNA methyltransferase status prediction in glioblastoma multiforme cancer using magnetic resonance imaging radiomics features: univariate and multivariate radiogenomics analysis. World Neurosurg 132:e140–e161. https://doi.org/10.1016/j.wneu.2019.08.232
Haubold J, Hosch R, Parmar V et al (2021) Fully automated MR based virtual biopsy of cerebral gliomas. Cancers 13:6186. https://doi.org/10.3390/cancers13246186
Haubold J, Demircioglu A, Gratz M et al (2020) Non-invasive tumor decoding and phenotyping of cerebral gliomas utilizing multiparametric 18F-FET PET-MRI and MR Fingerprinting. Eur J Nucl Med Mol Imaging 47:1435–1445. https://doi.org/10.1007/s00259-019-04602-2
He J, Ren J, Niu G et al (2022) Multiparametric MR radiomics in brain glioma: models comparation to predict biomarker status. BMC Med Imaging 22:1–13. https://doi.org/10.1186/s12880-022-00865-8
Huang WY, Wen LH, Wu G et al (2021) Comparison of radiomics analyses based on different magnetic resonance imaging sequences in grading and molecular genomic typing of glioma. J Comput Assist Tomogr 45:110–120. https://doi.org/10.1097/RCT.0000000000001114
Huang W, Wen L, Wu G et al (2021) Radiological model based on the standard magnetic resonance sequences for detecting methylguanine methyltransferase methylation in glioma using texture analysis. Cancer Sci 112:2835–2844. https://doi.org/10.1111/cas.14918
Jiang C, Kong Z, Liu S et al (2019) Fusion radiomics features from conventional MRI predict MGMT promoter methylation status in lower grade gliomas. Eur J Radiol 121:108714. https://doi.org/10.1016/j.ejrad.2019.108714
Kihira S, Tsankova NM, Bauer A et al (2021) Multiparametric MRI texture analysis in prediction of glioma biomarker status: added value of MR diffusion. Neurooncol Adv 3:1–9. https://doi.org/10.1093/noajnl/vdab051
Kihira S, Mei X, Mahmoudi K et al (2022) U-net based segmentation and characterization of gliomas. Cancers (Basel) 14:1–10. https://doi.org/10.3390/cancers14184457
Lu Y, Patel M, Natarajan K et al (2020) Machine learning-based radiomic, clinical and semantic feature analysis for predicting overall survival and MGMT promoter methylation status in patients with glioblastoma. Magn Reson Imaging 74:161–170. https://doi.org/10.1016/j.mri.2020.09.017
Pasquini L, Napolitano A, Lucignani M et al (2021) AI and high-grade glioma for diagnosis and outcome prediction: do all machine learning models perform equally well? Front Oncol 11:1–14. https://doi.org/10.3389/fonc.2021.601425
Sasaki T, Kinoshita M, Fujita K et al (2019) Radiomics and MGMT promoter methylation for prognostication of newly diagnosed glioblastoma. Sci Rep 9:1–9. https://doi.org/10.1038/s41598-019-50849-y
Shboul ZA, Chen J, Iftekharuddin KM (2020) Prediction of molecular mutations in diffuse low-grade gliomas using MR imaging features. Sci Rep 10:1–13. https://doi.org/10.1038/s41598-020-60550-0
Verduin M, Primakov S, Compter I et al (2021) Prognostic and predictive value of integrated qualitative and quantitative magnetic resonance imaging analysis in glioblastoma. Cancers (Basel) 13:1–20. https://doi.org/10.3390/cancers13040722
Vils A, Bogowicz M, Tanadini-Lang S et al (2021) Radiomic analysis to predict outcome in recurrent glioblastoma based on multi-center MR imaging from the prospective DIRECTOR trial. Front Oncol 11:1–9. https://doi.org/10.3389/fonc.2021.636672
Wei J, Yang G, Hao X et al (2019) A multi-sequence and habitat-based MRI radiomics signature for preoperative prediction of MGMT promoter methylation in astrocytomas with prognostic implication. Eur Radiol 29:877–888. https://doi.org/10.1007/s00330-018-5575-z
Xi BY, Guo F, Xu ZL et al (2018) Radiomics signature: a potential biomarker for the prediction of MGMT promoter methylation in glioblastoma. J Magn Reson Imaging 47:1380–1387. https://doi.org/10.1002/jmri.25860
Pease M, Gersey ZC, Ak M et al (2022) Pre-operative MRI radiomics model non-invasively predicts key genomic markers and survival in glioblastoma patients. J Neurooncol 160:253–263. https://doi.org/10.1007/s11060-022-04150-0
Mansouri A, Hachem LD, Mansouri S et al (2019) MGMT promoter methylation status testing to guide therapy for glioblastoma: refining the approach based on emerging evidence and current challenges. Neuro Oncol 21:167–178. https://doi.org/10.1093/neuonc/noy132
Malmström A, Łysiak M, Kristensen BW et al (2020) Do we really know who has an MGMT methylated glioma? Results of an international survey regarding use of MGMT analyses for glioma. Neurooncol Pract 7:68–76. https://doi.org/10.1093/nop/npz039
Bakas S, Akbari H, Sotiras A et al (2017) Advancing The Cancer Genome Atlas glioma MRI collections with expert segmentation labels and radiomic features. Sci Data 4:1–13. https://doi.org/10.1038/sdata.2017.117
Brancato V, Cerrone M, Lavitrano M et al (2022) A systematic review of the current status and quality of radiomics for glioma differential diagnosis. Cancers (Basel) 14:2731. https://doi.org/10.3390/cancers14112731
Vickers AJ, van Calster B, Steyerberg EW (2019) A simple, step-by-step guide to interpreting decision curve analysis. Diagnostic Progn Res 3:18. https://doi.org/10.1186/s41512-019-0064-7
Capogrosso P, Vickers AJ (2019) A systematic review of the literature demonstrates some errors in the use of decision curve analysis but generally correct interpretation of findings. Med Decis Mak 39:493–498. https://doi.org/10.1177/0272989X19832881
Park JE, Park SY, Kim HJ, Kim HS (2019) Reproducibility and generalizability in radiomics modeling: possible strategies in radiologic and statistical perspectives. Korean J Radiol 20:1124–1137. https://doi.org/10.3348/kjr.2018.0070
Kocak B, Baessler B, Bakas S et al (2023) CheckList for EvaluAtion of Radiomics research (CLEAR): a step-by-step reporting guideline for authors and reviewers endorsed by ESR and EuSoMII. Insights Imaging 14:75. https://doi.org/10.1186/s13244-023-01415-8
Vabalas A, Gowen E, Poliakoff E, Casson AJ (2019) Machine learning algorithm validation with a limited sample size. PLoS One 14:e0224365. https://doi.org/10.1371/journal.pone.0224365
Aoki K, Natsume A (2019) Overview of DNA methylation in adult diffuse gliomas. Brain Tumor Pathol 36:84–91. https://doi.org/10.1007/s10014-019-00339-w
Chen X, Zeng M, Tong Y et al (2020) Automatic prediction of MGMT status in glioblastoma via deep learning-based MR image analysis. Biomed Res Int 2020:9258649. https://doi.org/10.1155/2020/9258649
Saeed N, Ridzuan M, Alasmawi H et al (2023) MGMT promoter methylation status prediction using MRI scans? An extensive experimental evaluation of deep learning models. Med Image Anal 90:102989. https://doi.org/10.1016/j.media.2023.102989
Funding
This work was supported by the Italian Ministry of Health (RRC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is prof. Luca Maria Sconfienza.
Conflict of interest
Riccardo Pascuzzo, Tugba Akinci D’Antonoli, and Renato Cuocolo are members of the European Radiology Scientific Editorial Board. Luca Maria Sconfienza is a member of the European Radiology Advisory Editorial Board. They have not taken part in the review or selection process of this article. All remaining authors declare no competing interests related to the subject matter of this article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was not required for this study because this is a systematic review.
Ethical approval
Institutional Review Board approval was not required because this is a systematic review.
Study subjects or cohorts overlap
Since this study is a systematic review and meta-analysis, all data were collected from previously published studies.
Methodology
• Systematic review and meta-analysis
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Doniselli, F.M., Pascuzzo, R., Mazzi, F. et al. Quality assessment of the MRI-radiomics studies for MGMT promoter methylation prediction in glioma: a systematic review and meta-analysis. Eur Radiol 34, 5802–5815 (2024). https://doi.org/10.1007/s00330-024-10594-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-024-10594-x