Abstract
Objective
To investigate the effect of cholinergic pathways damage caused by white matter hyperintensities (WMHs) on cognitive function in moyamoya disease (MMD).
Methods
We included 62 patients with MMD from a prospectively enrolled cohort. We evaluated the burden of cholinergic pathways damage caused by WMHs using the Cholinergic Pathways Hyperintensities Scale (CHIPS). Cognitive function was evaluated with the Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA). Cognitive impairment was determined according to the cut-off of MMSE and education. Multivariate linear and logistic regression models were used to analyze whether CHIPS was independently associated with cognition. Receiver operating characteristic curve analysis was performed to identify the ability of CHIPS in discriminating cognitive impairment and normal cognition.
Results
CHIPS was associated with both MMSE and MoCA (β = − 0.601 and β = − 0.672, both p < 0.001). After correcting age, sex, education, volumes of limbic areas, and other factors, CHIPS remained to be independently associated with both MMSE and MoCA (β = − 0.388 and β = − 0.334, both p < 0.001). In the logistic regression, only CHIPS was associated with cognitive impairment (odds ratio = 1.431, 95% confidence interval = 1.103 to 1.856, p = 0.007). The optimal cut-off of CHIPS score was 10, yielding a sensitivity of 87.5% and a specificity of 78.3% in identifying MMD patients with cognitive impairment.
Conclusions
The damage of cholinergic pathways caused by WMHs plays an independent effect on cognition and CHIPS could be a useful method in identifying MMD patients likely to be cognitive impairment.
Clinical relevance statement
This study shows that Cholinergic Pathways Hyperintensities Scale (CHIPS) could be a simple and reliable method in identifying cognitive impairment for patients with moyamoya disease. CHIPS could be helpful in clinical practice, such as guiding treatment decisions and predicting outcome.
Key Points
• Cholinergic Pathways Hyperintensities Scale was significantly associated with cognitive screening tests in patients with moyamoya disease.
• Cholinergic Pathways Hyperintensities Scale plays an independent effect on cognitive impairment in patients with moyamoya disease.
• Cholinergic Pathways Hyperintensities Scale shows higher accuracy than education, volumes of limbic areas, and sex in identifying cognitive impairment in moyamoya disease.





Similar content being viewed by others
Abbreviations
- CCH:
-
Chronic cerebral hypoperfusion
- CHIPS:
-
Cholinergic Pathways Hyperintensities Scale
- ICA:
-
Internal carotid arteries
- MMD:
-
Moyamoya disease
- MMSE:
-
Mini-Mental State Examination
- MoCA:
-
Montreal Cognitive Assessment
- mRS:
-
Modified Rankin Scale
- ROC:
-
Receiver operating characteristic
- WMHs:
-
White matter hyperintensities
References
Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360:1226–1237
Ihara M, Yamamoto Y, Hattori Y et al (2022) Moyamoya disease: diagnosis and interventions. Lancet Neurol 21:747–758
Karzmark P, Zeifert PD, Bell-Stephens TE, Steinberg GK, Dorfman LJ (2012) Neurocognitive impairment in adults with moyamoya disease without stroke. Neurosurgery 70:634–638
Shen X-X, Zhang H-D, Fu H-G et al (2023) Association of cognitive function and hypoperfusion in moyamoya disease patients without stroke. J Cereb Blood Flow Metab 43:542–551
Kazumata K, Tokairin K, Sugiyama T et al (2019) Association of cognitive function with cerebral blood flow in children with moyamoya disease. J Neurosurg Pediatr 25:62–68
Mansour A, Niizuma K, Rashad S et al (2018) A refined model of chronic cerebral hypoperfusion resulting in cognitive impairment and a low mortality rate in rats. J Neurosurg 131:892–902
Duncombe J, Kitamura A, Hase Y, Ihara M, Kalaria RN, Horsburgh K (2017) Chronic cerebral hypoperfusion: a key mechanism leading to vascular cognitive impairment and dementia. Closing the translational gap between rodent models and human vascular cognitive impairment and dementia. Clin Sci 131:2451–2468
Prins ND, Scheltens P (2015) White matter hyperintensities, cognitive impairment and dementia: an update. Nat Rev Neurol 11:157–165
Sun H, Li W, Xia C et al (2022) Magnetic resonance imaging markers of cerebral small vessel disease in adults with moyamoya disease. Transl Stroke Res 13:533–542
Yang W, Jung K-H, Kang D-W et al (2023) Characteristics and clinical implication of white matter lesions in patients with adult moyamoya disease. Neurology 100:e1912–e1921
Komatsu K, Mikami T, Noshiro S, Miyata K, Wanibuchi M, Mikuni N (2016) Reversibility of white matter hyperintensity by revascularization surgery in moyamoya disease. J Stroke Cerebrovasc Dis 25:1495–1502
Li S, Xiong J, He Y, Xiao Y, Mao D, Liu L (2020) A rare case of pediatric moyamoya disease with reversible white matter lesions in a 3-year-old Chinese girl. Childs Nerv Syst 36:197–201
Geraldo AF, Leitão C, Nunes J, Vila-Real M (2020) Partially reversible confluent white matter lesions in a Caucasian child with moyamoya disease. Childs Nerv Syst 36:2605–2608
Ballinger EC, Ananth M, Talmage DA, Role LW (2016) Basal forebrain cholinergic circuits and signaling in cognition and cognitive decline. Neuron 91:1199–1218
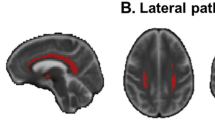
Bocti C, Swartz RH, Gao F-Q, Sahlas DJ, Behl P, Black SE (2005) A new visual rating scale to assess strategic white matter hyperintensities within cholinergic pathways in dementia. Stroke 36:2126–2131
Shin J, Choi S, Lee JE, Lee HS, Sohn YH, Lee PH (2012) Subcortical white matter hyperintensities within the cholinergic pathways of Parkinson’s disease patients according to cognitive status. J Neurol Neurosurg Psychiatry 83:315–321
Hu J, Wang Y, Zhu Y et al (2023) Preoperative brain functional connectivity improve predictive accuracy of outcomes after revascularization in moyamoya disease. Neurosurgery 92:344–352
Lim J-S, Kim N, Jang MU et al (2014) Cortical hubs and subcortical cholinergic pathways as neural substrates of poststroke dementia. Stroke 45:1069–1076
Fazekas F, Chawluk JB, Alavi A, Hurtig H, Zimmerman R (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJNR Am J Neuroradiol 149:351–356
Catani M, Dell’Acqua F, De Schotten MT (2013) A revised limbic system model for memory, emotion and behaviour. Neurosci Biobehav Rev 37:1724–1737
Schoemaker D, Buss C, Head K et al (2016) Hippocampus and amygdala volumes from magnetic resonance images in children: assessing accuracy of FreeSurfer and FSL against manual segmentation. Neuroimage 129:1–14
Liu C-F, Hsu J, Xu X et al (2023) Digital 3D brain MRI arterial territories atlas. Sci Data 10:74
Houkin K, Nakayama N, Kuroda S, Nonaka T, Shonai T, Yoshimoto T (2005) Novel magnetic resonance angiography stage grading for moyamoya disease. Cerebrovasc Dis 20:347–354
Li H, Jia J, Yang Z (2016) Mini-Mental State Examination in elderly Chinese: a population-based normative study. J Alzheimers Dis 53:487–496
Román GC, Kalaria RN (2006) Vascular determinants of cholinergic deficits in Alzheimer disease and vascular dementia. Neurobiol Aging 27:1769–1785
Selden NR, Gitelman DR, Salamon-Murayama N, Parrish TB, Mesulam M-M (1998) Trajectories of cholinergic pathways within the cerebral hemispheres of the human brain. Brain 121:2249–2257
Qu J, Chen Y, Luo G, Zhao J, Zhong H, Yin H (2018) Severe lesions involving cortical cholinergic pathways predict poorer functional outcome in acute ischemic stroke. Stroke 49:2983–2989
Lim JS, Kwon HM, Lee YS (2020) Effect of cholinergic pathway disruption on cortical and subcortical volumes in subcortical vascular cognitive impairment. Eur J Neurol 27:210–212
Kazumata K, Tha KK, Narita H et al (2015) Chronic ischemia alters brain microstructural integrity and cognitive performance in adult moyamoya disease. Stroke 46:354–360
Kazumata K, Tokairin K, Ito M et al (2020) Combined structural and diffusion tensor imaging detection of ischemic injury in moyamoya disease: relation to disease advancement and cerebral hypoperfusion. J Neurosurg 134:1155–1164
Edden RA, Jones DK (2011) Spatial and orientational heterogeneity in the statistical sensitivity of skeleton-based analyses of diffusion tensor MR imaging data. J Neurosci Methods 201:213–219
Kronenburg A, Van Den Berg E, Van Schooneveld MM et al (2018) Cognitive functions in children and adults with moyamoya vasculopathy: a systematic review and meta-analysis. J Stroke 20:332–341
Miyamoto S, Kikuchi H, Karasawa J, Nagata I, Ikota T, Takeuchi S (1984) Study of the posterior circulation in moyamoya disease: clinical and neuroradiological evaluation. J Neurosurg 61:1032–1037
Jochems ACC, Arteaga C, Chappell F et al (2022) Longitudinal changes of white matter hyperintensities in sporadic small vessel disease: a systematic review and meta-analysis. Neurology 99:e2454–e2463
Duering M, Finsterwalder S, Baykara E et al (2018) Free water determines diffusion alterations and clinical status in cerebral small vessel disease. Alzheimers Dement 14:764–774
Yu X, Yin X, Hong H et al (2021) Increased extracellular fluid is associated with white matter fiber degeneration in CADASIL: in vivo evidence from diffusion magnetic resonance imaging. Fluids Barriers CNS 18:29
Wardlaw JM, Valdés Hernández MC, Muñoz-Maniega S (2015) What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. J Am Heart Assoc 4:e001140
Kolb B, Fadel H, Rajah G, Saber H, Luqman A, Rangel-Castilla L (2019) Effect of revascularization on cognitive outcomes in intracranial steno-occlusive disease: a systematic review. Neurosurg Focus 46:E14
Levine DA, Gross AL, Briceño EM et al (2021) Sex differences in cognitive decline among US adults. JAMA Netw Open 4:e210169
Miller DI, Halpern DF (2014) The new science of cognitive sex differences. Trends Cogn Sci 18:37–45
Funding
This study has received funding by the National Natural Science Foundation of China (No. 81901706, No. 82171271).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Minming Zhang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained. The study was approved by the Medical Ethics Committee of the Second Affiliated Hospital, Zhejiang University School of Medicine.
Study subjects or cohorts overlap
None.
Methodology
• prospective
• cross-sectional study
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, D., Yu, X., Hu, J. et al. White matter hyperintensities in cholinergic pathways correlates of cognitive impairment in moyamoya disease. Eur Radiol (2023). https://doi.org/10.1007/s00330-023-10489-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-023-10489-3