Abstract
Objectives
Coronary artery calcifications (CACs) indicate the presence of coronary artery disease. CAC can be found on thoracic computed tomography (CT) conducted for non-cardiac reasons. This systematic review and meta-analysis of non-gated thoracic CT aims to assess the clinical impact and prevalence of CAC.
Methods
Online databases were searched for articles assessing prevalence, demographic characteristics, accuracy and prognosis of incidental CAC on non-gated thoracic CT. Meta-analysis was performed using a random effects model.
Results
A total of 108 studies (113,406 patients) were included (38% female). Prevalence of CAC ranged from 2.7 to 100% (pooled prevalence 52%, 95% confidence interval [CI] 46–58%). Patients with CAC were older (pooled standardised mean difference 0.88, 95% CI 0.65–1.11, p < 0.001), and more likely to be male (pooled odds ratio [OR] 1.95, 95% CI 1.55–2.45, p < 0.001), with diabetes (pooled OR 2.63, 95% CI 1.95–3.54, p < 0.001), hypercholesterolaemia (pooled OR 2.28, 95% CI 1.33–3.93, p < 0.01) and hypertension (pooled OR 3.89, 95% CI 2.26–6.70, p < 0.001), but not higher body mass index or smoking. Non-gated CT assessment of CAC had excellent agreement with electrocardiogram-gated CT (pooled correlation coefficient 0.96, 95% CI 0.92–0.98, p < 0.001). In 51,582 patients, followed-up for 51.6 ± 27.4 months, patients with CAC had increased all cause mortality (pooled relative risk [RR] 2.13, 95% CI 1.57–2.90, p = 0.004) and major adverse cardiovascular events (pooled RR 2.91, 95% CI 2.26–3.93, p < 0.001). When CAC was present on CT, it was reported in between 18.6% and 93% of reports.
Conclusion
CAC is a common, but underreported, finding on non-gated CT with important prognostic implications.
Clinical relevance statement
Coronary artery calcium is an important prognostic indicator of cardiovascular disease. It can be assessed on non-gated thoracic CT and is a commonly underreported finding. This represents a significant population where there is a potential missed opportunity for lifestyle modification recommendations and preventative therapies. This study aims to highlight the importance of reporting incidental coronary artery calcium on non-gated thoracic CT.
Key Points
• Coronary artery calcification is a common finding on non-gated thoracic CT and can be reliably identified compared to gated-CT.
• Coronary artery calcification on thoracic CT is associated with an increased risk of all cause mortality and major adverse cardiovascsular events.
• Coronary artery calcification is frequently not reported on non-gated thoracic CT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease is the most common cause of death around the world [1]. However, the majority of patient with coronary artery disease are asymptomatic and unaware of this diagnosis. The presence of coronary artery calcium (CAC) indicates that a patient has coronary artery disease, and this gives important information about prognosis beyond that provided by traditional cardiovascular risk factors [2]. An elevated coronary artery calcium score increases the risk of subsequent adverse cardiovascular events, even in asymptomatic patients [3]. However, CAC can also be assessed on thoracic computed tomography (CT) conducted for non-cardiac reasons.
Electrocardiogram (ECG) gating is used for dedicated CT to assess CAC in order to minimise coronary artery motion artefacts and optimise quantification [4]. However, CAC can also be identified and quantified on non-ECG gated CT performed for non-cardiac indications. Several previous studies have shown that CAC on non-gated thoracic CT is associated with subsequent cardiac events, including in populations undergoing lung cancer screening [5,6,7,8]. Recently published guidelines support the reporting of CAC on all CT of the chest [9, 10]. However, at present, incidental CAC is frequently not reported on CT scans performed for non-cardiac indications [11, 12].
This systematic review and meta-analysis aimed to assess the prevalence of incidental CAC identified on non-gated thoracic CT and its association with patient characteristics and adverse outcomes. Furthermore, we investigate the accuracy of non-gated thoracic CT compared to gated cardiac CT for the assessment of CAC and the frequency of reporting of incidental CAC on non-gated CT.
Methods
Information sources and search terms
PRISMA reporting guidelines were followed for this meta-analysis (Supplementary Table 1) and the protocol was registered (PROSPERO CRD42022342234). PubMed, Medline and Embase were searched to July 2022 using the terms computed tomography, non-gated, coronary and calcification, and synonyms. Full search terms are listed in the supplementary information (Supplementary Table 2). Reference lists from relevant review articles and all eligible studies were also reviewed for relevant articles.
Study selection
Two reviewers (M.O.G, A.A) participated in literature selection. Studies were included if they analysed one of the following topics about coronary artery calcium scoring (CACS) on non-gated thoracic CT: (1) prevalence of CAC on non-gated thoracic CT, (2) agreement between non-gated and gated CT, (3) comparison of patient characteristics with or without CAC on non-gated thoracic CT, (4) prognostic performance of CAC to predict adverse events on non-gated thoracic CT, (5) reporting practices of CAC on non-gated thoracic CT.
Conference proceedings, case reports, editorials, letters, opinion pieces and studies without English versions were excluded. Titles and abstracts were screened and full texts were obtained. Two investigators independently assessed articles for eligibility and quality, with disagreement settled by consensus. When multiple publications based on the same trial were identified, only the largest sample size was included to avoid duplicate reporting.
Data extraction
A standardised data extraction form was used to collect study and participant characteristics, methodology and study results. For all studies, information was collected concerning study design, CT technology, and participant demographic characteristics. The prevalence and severity of CAC was recorded, using continuous or categorical metrics as available. When available, the proportion of subjects with a CAC of 0 versus above 0, and below and above 400 Agatston units (AU) were extracted. A ‘high’ CACS was defined as Agatston score > 300 AU or a visual ordinal score of severe. Information on reporting practices and agreement between gated and non-gated CT were recorded. For studies assessing agreement, correlation coefficients were extracted for continuous data and weighted-Cohen K was calculated for categorical data.
To calculate the prognostic significance of CAC on thoracic CT, information on cardiovascular events during follow-up was extracted. The number of events were recorded for all-cause mortality, coronary heart disease death and major adverse cardiovascular events (MACEs) including cardiovascular death, non-fatal myocardial infarction, stroke, new-onset arrhythmia and heart failure, where possible, raw data, adjusted and unadjusted hazard ratios with 95% confidence intervals (CI) were recorded.
Study quality assessment
Two reviewers evaluated study quality. Studies assessing agreement between non-gated and gated CT were evaluated using the Quality Assessment of Diagnostic Accuracy Studies 2 [13] method with each domain scored from 1 (fulfilled) to 0 (unmet) and a total possible score of 7. For studies evaluating the presence of CAC, reporting practices and associations with demographic characteristics, study quality was assessed using the National Heart, Lung and Blood Institute (NIH) Quality Assessment Tool for Observational and Cross-sectional Studies [14]. Each domain was scored from 1 (fulfilled) to 0 (unmet) with a total possible score of 14. Seventeen studies of prognosis were evaluated with the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) 8 criteria tool [14] (12). It gives a total score of 16, with ≥ 11 considered high quality, 7–10 moderate quality and ≤ 6 low quality. Five studies of prognosis were assessed using the NIH Quality Assessment Tool for Case-Cohort studies, with domains scored as 1 (fulfilled) to 0 (unmet) and a total possible score of 12 [14].
Data synthesis and statistical analysis
Statistical analysis was performed using R version 1.3.959 (R Foundation). A 2-sided p value < 0.05 was considered significant. Where age was reported as median with interquartile range, assessment for skewness was performed using the method reported by Shi et al [15]. If the skew of the data was significant, it was excluded from the analysis and if it was not, mean and standard deviation was calculated using the method reported by Shi et al [16] and Luo et al [17]. Meta-analysis was performed using the metafor package [18]. Pooling calculations for agreement between calcium assessment methods was performed using the Hedges-Vevea random effects model. Q statistics and I2 index were used to test for heterogeneity with a 2-sided p value < 0.1 or > 50% indicating heterogeneity, respectively. For categorical variables, proportion and 95% CI are presented. The relative risk (RR) and 95% CI was calculated for the risk of events in patients with and without CAC. Odds ratios (ORs) and 95% CI were calculated for the presence of cardiovascular risk factors in patients with and without CAC. Standardised mean difference was calculated for continuous variables. Publication bias was assessed using the Begg and Mazumdar rank correlation and Egger regression test if the effect size was 3 or more in the included studies.
Results
Study selection
After removal of duplicates, 7708 papers were identified (Fig. 1). Of these, 108 studies were included in the systematic review [11, 19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125] and meta-analysis was performed on 96 studies assessing CAC prevalence, 23 studies comparing non-gated to gated CT, 33 studies providing information on participant characteristics, 41 studies assessing the prognostic implication of CAC and 12 studies assessing reporting practices (Supplementary Table 4).
Study characteristics
The systematic review included 114,036 participants (range of mean age 46.4 to 74 years), comprising 63,115 men (55%), 43,138 females (38%) and 7743 (7%) individuals without indicated sex (Table 1). Nineteen studies were prospective and 92 studies were retrospective. A variety of CT modalities were used ranging from single slice to 256-row multidetector CT, and including attenuation correction CT for positron emission tomography. Six studies used electron beam CT. Low-dose CT acquisition was used in 44 studies and normal dose CT in 68 studies. CAC was assessed with the Agatston method [126] in 54 studies, with a visual ordinal or Weston scale in 30 studies, or with binary assessment of its presence or absence in 26 studies.
Prevalence of coronary artery calcification on non-gated CT
Prevalence of incidental CAC on non-cardiac CT was reported in 94 studies, including 89,006 patients. The prevalence ranged from 2.7 to 100% (Fig. 2) with a pooled prevalence of 52% (95% CI 46 to 58%).
There was moderate heterogeneity between the included studies (I2 > 50%, p = 0) with higher CAC prevalence in studies of older patients and those with a higher prevalence of men. No publication bias was found in the pooling (Eggers: p = 0.23, Begg’s: p = 0.31). All 66 studies that evaluated the incidence of CAC, reporting practices for CAC or cardiovascular risk factors, were of high or moderate quality with sub-optimal scores present for 9 domains (Supplementary Table 3).
Impact of demographic characteristics on coronary artery calcification
Information on cardiovascular risk factors was available in 33 studies (sex in 32 studies, age in 14 studies, body mass index (BMI) in 5 studies, diabetes mellitus in 24 studies, hypercholesterolaemia in 21 studies, hypertension in 22 studies and smoking history in 22 studies). All of these studies showed heterogeneity in the pooling calculation (Q test p < 0.001 and I2 > 50%). No publication bias was found in the pooling (Eggers: p = 0.50, p = 0.25, p = 0.12, p = 0.15, p = 0.11, p = 0.67, p = 0.83).
Mean age was 60.3 ± 10.3 years and patients with CACS > 0 were older than those without CAC (pooled standardised mean difference 0.88, 95% CI 0.65 to 1.11, p < 0.001, Supplementary Fig. 1). Of the 106,293 patients where sex was reported, 59.4% were male and 40.6% were female. Men were more likely to have CAC than women (pooled odds ratio 1.95, 95% CI 1.55 to 2.45, p < 0.001, Supplementary Fig. 2). The presence of diabetes mellitus (pooled odds ratio 2.63, 95% CI 1.95 to 3.54, p < 0.001, Supplementary Fig. 3), hypercholesterolaemia (pooled odds ratio 2.28, 95% CI 1.33 to 3.93, p < 0.01, Supplementary Fig. 4), and hypertension (pooled odds ratio 3.89, 95% CI 2.26 to 6.70, p < 0.001, Supplementary Fig. 5) was all associated with an increased likelihood of having CAC. However, there was no difference in smoking history (pooled odds ratio 1.35, 95% CI 0.98 to 1.85, p = 0.06, Supplementary Fig. 6) or BMI between those with and without CAC (pooled standardised mean difference 0.05, 95% CI − 0.34 to 0.44, p = 0.74, Supplementary Fig. 7).
Prognostic implications of CAC on non-gated CT
Forty studies (51,582 patients) reported cardiovascular events or all-cause mortality in patients with and with out CAC. Patients were followed up for a mean of 51.6 ± 27.4 months.
Compared the patients without CAC, patients with CAC had an increase risk of all-cause mortality (pooled relative risk 2.13, 95% CI 1.57 to 2.90, p = 0.004), MACE (pooled relative risk 2.91, 95% CI 2.26 to 3.93, p < 0.001) and combined all-cause mortality and MACE (pooled relative risk 2.61, 95% CI 2.17 to 3.74, p < 0.001, Fig. 3). There was heterogeneity amongst studies reporting all cause mortality or MACE (I2 > 50%, Q test p < 0.001). Publication bias could not be assessed for all-cause mortality due to insufficient sample size. No publication bias was found in the pooling calculations for MACE or combined all-cause mortality and MACE (Eggers test p = 0.08 and p = 0.17, respectively).
There were 10 studies which reported cardiovascular events or all-cause mortality in patients with different categories of CAC severity. There was an increased risk of all cause mortality and MACE in patients with a ‘high’ CACS compared to those with a ‘low’ CACS (RR 3.92, 95% CI 2.50 to 6.14, p < 0.001, Supplementary Fig. 8). There was heterogeneity in the pooling calculation (I2 > 50%, Q test p < 0.001) but in the pooling calculation no publication bias was found (p = 0.92).
The clinical implications of CAC in patients undergoing lung cancer screening were reported in 5 studies. Compared to patients without CAC, patients with CAC who were undergoing lung cancer screening had an increased risk of combined MACE and all cause mortality (pooled relative risk 3.27, 95% CI 1.88 to 5.68, p = 0.004). There was no heterogeneity amongst these studies (I2 < 50%, Q test p = 0.23 and) but publication bias could not be assessed due to insufficient sample size.
All prognostic studies were of high or moderate quality, with suboptimal scores present due to limited sample sizes (Supplementary Fig. 3).
Reporting of incidental CAC on non-gated CT
Eleven studies (5350 patients) assessed whether incidental CAC on non-gated CT was reported. When CAC was present, it was reported in between 18.6% and 93% of CT reports. The pooled proportion of reports that included mention of CAC when present was 57% (95% CI 0.39 to 0.74, p < 0.01, Fig. 4). These studies had significant heterogeneity (I2 = 98%, p < 0.001) but no publication bias was found in the pooling (Eggers: p = 0.17; Begg: p = 0.70).
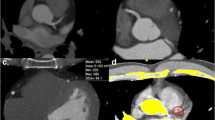
Agreement between gated and non-gated CT
Twenty-three studies (6537 patients) provided information on the diagnostic accuracy of non-gated CT compared to gated CT, of which 47.8% had no CAC, 25.5% had CACS 1 to 99 AU, 12.1% had CACS 100 to 399 AU and 11.0% had CACS > 400 AU on gated CT (Fig. 5). The tube voltage used for non-gated CT was 100 kV for 4 studies, 120 kV for 15 studies and 80 kV/140 kV for 1 study. Two studies varied tube voltage based on body mass index and 1 study did not report the tube voltage.
Of the 3021 patient with CACS on gated CT, 129 (4.3%) showed no CAC on non-gated CT. Non-gated CT downgraded the CACS severity from > 400 to 100–399 AU for 6.4% (n = 44/685) and upgraded CACS severity from < 400 to > 400 AU for 1.2% (n = 66/5416), compared to ECG-gated CT.
Fifteen studies (5181 patients) provided information on the correlation between CACS calculated on non-gated and gated CT. The correlation ranged from 81 to 100% and the pooled correlation coefficient showed excellent agreement (R 0.96, 95% CI 0.92 to 0.98, p < 0.001, Fig. 6). There was significant heterogeneity between these studies (I2 > 50%, Q test p < 0.001) but no publication bias was identified (Eggers: p = 0.16; Begg: p = 0.30).
Seventeen studies (4598 participants) reported the comparison between gated CT and non-gated CT with CACS provided with 4 categories of severity (CAC score 0, 1–99, 100–399 and > 400 AU). The pooled Cohen κ showed very good agreement between gated and non-gated CT (0.84, 95% CI 0.75 to 0.90, p < 0.001, Supplementary Fig. 9). There was significant heterogeneity between studies (I2 > 50%, Q test p < 0.001) but no publication bias was identified (Eggers: p = 0.06; Begg: p = 0.93).
All studies on agreement between non-gated and gated CT were of high quality according to the QUADAS-2 scoring tool. Suboptimal scores were present in 3 domains of the QUADAS-2 tool, with 4 studies not mention whether CT interpretation was blinded and 3 studies not mention the timing of measurements (Supplementary Fig. 3).
Discussion
In this meta-analysis, we have demonstrated that as an incidental finding on thoracic CT, coronary artery calcium is a frequent finding and has important prognostic implications. On non-gated thoracic CT scans, CAC was present on 52% of scans performed for non-cardiac indications. The occurrence of CAC on non-gated thoracic CT was related to the presence of traditional cardiovascular risk factors, except for smoking status and body mass index. Patients with incidental CAC on thoracic CT were more likely to develop subsequent cardiovascular events or all-cause mortality. Quantification of CAC on non-gated CT correlates well with the gold standard of ECG-gated CT. However, CAC on non-gated CT is only reported in approximately half of the CT scans where it is present. This highlights an important unmet need which should be addressed.
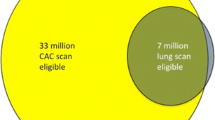
The number of thoracic CT performed around the world every year is rapidly increasing, particularly with the instigation of lung cancer screening CT. CAC will be a common finding on these CT scans, occurring in up to 91.7% of patients in some studies [52]. At present, CAC is frequently not reported on thoracic CT. In this meta-analysis, it was only reported in just over half of scans where it was present. This is a potential missed opportunity for lifestyle modification recommendations and preventative therapies. We have shown a wide range for the prevalence of CAC on non-gated thoracic CT, from 3 to 100% in studies included in this meta-analysis. Underlying differences in age, sex and prevalence of cardiovascular risk factors were key drivers of this. Patients with incidental CAC on thoracic CT were more likely to be older males, with a history of diabetes, hypercholesterolaemia and hypertension. Overall, CAC was present in just under half of patients undergoing non-gated CT. This is therefore a common incidental finding which may be a significant indicator of poor prognosis.
Although CAC is traditionally evaluated on cardiac-specific gated CT, we have confirmed that there is excellent agreement between non-gated and gated CT for the assessment of CAC. Indeed, the correlation between Agatston scores calculated using non-gated and gated CT was was excellent (Pooled R = 0.96) and stratification across four risk groups (CAC score 0, 1–99, 100–399 and > 400 AU) showed very good agreement (Pooled Cohen κ = 0.84). Agatston scoring is time -onsuming to perform manually on routine thoracic CT, but in the future automation with machine learning will mean that this can be done rapidly in advance of scan reporting. In the mean time, ordinal visual assessment is recommended by contemporary guidelines [10]. It should also be remembered that CAC only identifies one type of atherosclerotic plaque, and ignores non-calcified plaque.
It is interesting that we did not find an association between CAC and body mass index or smoking status. This is likely because of the complex relationship between these risk factors and the presence of cardiovascular disease and adverse cardiovascular outcomes. Large studies of unselected patients undergoing CAC scoring have shown an association between CAC and body mass index [127]. However, other studies have shown that body mass index is not an independent predictor of CAC when corrected for other cardiovascular risk factors [128], and that there is an inverse relationship between lesion-specific CAC and body mass index [129]. The lack of association between smoking status and CAC has been shown in previous studies of patients undergoing thoracic CT [130]. The reasons for this are multi-factorial, and likely include the prevalence of smoking in those undergoing imaging, the indication for imaging and challenges with recording accurate smoking status.
Absence of coronary artery calcium is associated with a low risk of cardiac events, extending to 15 years in asymptomatic patients [131]. We found that over a mean follow-up of 51.6 months, 11.9% of subjects with CAC score above 0 experienced a cardiovascular event compared to 3.4% of subjects with CAC score of 0. A previous meta-analysis demonstrated a lower risk of cardiovascular events in patients with calcium score of 0, of 0.47% over a mean follow-up of 50 months [132]. This difference is likely due to the inclusion of a wider range of patients in our meta-analysis, who had a higher frequency of underlying cardiovascular risk factors. There is also a higher risk of cardiovascular events in patietns with CAC who are undergoing lung cancer screening. These patients are more likely to be older and have a history of smoking. However, the low radiation dose nature of many lung cancer screening CT scans also means that the presence of CAC may be underestimated in these patients.
The presence of calcification on thoracic CT has important implications for patients. National and international guidelines now recommend that patients with CAC identified as an incidental finding on thoracic CT should have an assessment of their cardiovascular risk factors, such as the presence of hypertension, and be considered for preventative therapies [9, 10]. Research into the clinical implications of such management changes is currently limited. A recent single-centre retrospective analysis of 1400 chest CT found that the number needed to report to impact management was low, at only 2 scans [133]. However, to date, there are no randomised studies which assess the impact on outcomes of changing management based on the presence of incidental CAC on thoracic CT.
This study has a number of limitations. A range of different CT scanner types, radiation doses and slice thicknesses were present between studies resulting in significant heterogeneity. The number of patients who underwent both gated and non-gated CT was relatively low. A number of different calcium scoring methods were used in studies reporting prognosis and the number of cardiovascular events reported during follow-up was relatively low. The studies of prognosis reported a variety of cardiovascular events, leading to heterogeneity between these studies. All included studies were heterogenous for the participant population characteristics, imaging equipment and acquisition protocol. The random-effects model was used to compensate for some of the heterogeneity in the pooling calculation, and sensitivity analyses were used to identify influential outliers to minimise the heterogeneity.
To conclude, this meta-analysis has established that non-gated thoracic CT is a useful technique to identify incidental coronary artery calcification. CAC is frequently identified on non-gated thoracic CT and this has a significant impact on prognosis. Despite the relationship between CAC and subsequent cardiovascular events and all-cause mortality, CAC is often not mentioned in clinical reports.
Data availability
Available
Abbreviations
- ACCF/AHA:
-
American College of Cardiology Foundation/American Heart Association
- AU:
-
Agatston units
- CAC:
-
Coronary artery calcification
- CACS:
-
Coronary artery calcium scoring
- CI:
-
Confidence intervals
- CT:
-
Computed tomography
- ECG:
-
Electrocardiogram
- NIH:
-
National Heart, Lung and Blood Institute
- OR:
-
Odds ratio
- RR:
-
Relative risk
References
World Health Organisation (2021) Cardiovascular diseases (CVDs). In: Fact Sheet . https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 10 Jan 2022
Williams MC, Moss AJ, Dweck M et al (2019) Coronary artery plaque characteristics associated with adverse outcomes in the SCOT-HEART study. J Am Coll Cardiol 73:291–301. https://doi.org/10.1016/j.jacc.2018.10.066
Detrano R, Guerci AD, Carr JJ et al (2008) Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 358:1336–1345. https://doi.org/10.1056/nejmoa072100
Oudkerk M, Stillman AE, Halliburton SS et al (2008) Coronary artery calcium screening: current status and recommendations from the European Society of Cardiac Radiology and North American Society for Cardiovascular Imaging. Eur Radiol 18:2785–2807. https://doi.org/10.1007/s00330-008-1095-6
Jacobs PC, Gondrie MJA, van der Graaf Y et al (2012) Coronary artery calcium can predict all-cause mortality and cardiovascular events on low-dose ct screening for lung cancer. AJR Am J Roentgenol 198:505–511. https://doi.org/10.2214/AJR.10.5577
van de Wiel JCM, Wang Y, Xu DM et al (2007) Neglectable benefit of searching for incidental findings in the Dutch-Belgian lung cancer screening trial (NELSON) using low-dose multidetector CT. Eur Radiol 17:1474–1482. https://doi.org/10.1007/s00330-006-0532-7
Sverzellati N, Cademartiri F, Bravi F et al (2012) Relationship and prognostic value of modified coronary artery calcium score, FEV 1, and emphysema in lung cancer screening population: the MILD trial. Radiology 262:460–467. https://doi.org/10.1148/radiol.11110364
Takx RAP, Išgum I, Willemink MJ et al (2015) Quantification of coronary artery calcium in nongated CT to predict cardiovascular events in male lung cancer screening participants: Results of the NELSON study. J Cardiovasc Comput Tomogr 9:50–57. https://doi.org/10.1016/j.jcct.2014.11.006
Hecht HS, Cronin P, Blaha MJ et al (2017) 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: A report of the society of cardiovascular computed tomography and society of thoracic radiology. J Cardiovasc Comput Tomogr 11:74–84. https://doi.org/10.1016/j.jcct.2016.11.003
Williams MC, Abbas A, Tirr E et al (2020) Reporting incidental coronary, aortic valve and cardiac calcification on non-gated thoracic computed tomography, a consensus statement from the BSCI/BSCCT and BSTI. Br J Radiol 20200894. https://doi.org/10.1259/bjr.20200894
Sverzellati N, Arcadi T, Salvolini L et al (2016) Under-reporting of cardiovascular findings on chest CT. Radiol Med 121:190–199. https://doi.org/10.1007/s11547-015-0595-0
Williams M, Weir-McCall J, Moss A et al (2020) Radiologist opinions regarding reporting incidental coronary and cardiac calcification on thoracic CT. J Cardiovasc Comput Tomogr 14:S57. https://doi.org/10.1016/j.jcct.2020.06.103
Whiting PF, Rutjes AWS, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Study Quality Assessment Tools | NHLBI, NIH. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 25 Oct 2020
Shi J, Luo D, Wan X et al (2020) Detecting the skewness of data from the five-number summary and its application in meta-analysis. https://doi.org/10.48550/ARXIV.2010.05749
Shi J, Luo D, Weng H et al (2020) Optimally estimating the sample standard deviation from the five‐number summary. Res Synth Methods 11:641–654. https://doi.org/10.1002/jrsm.1429
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range and/or mid-quartile range. Stat Methods Med Res 27:1785–1805
Viechtbauer W (2010) Conducting meta-analyses inRwith themetaforPackage. J Stat Softw 36. https://doi.org/10.18637/jss.v036.i03
An S, Fan R, Zhao B et al (2022) Evaluating coronary artery calcification with low-dose chest CT reconstructed by different kernels. Clin Imaging 83:166–171. https://doi.org/10.1016/j.clinimag.2021.12.024
Arcadi T (2014) Coronary artery calcium score on low-dose computed tomography for lung cancer screening. World J Radiol 6:381. https://doi.org/10.4329/wjr.v6.i6.381
Atkins KM, Weiss J, Zeleznik R et al (2022) Elevated coronary artery calcium quantified by a validated deep learning model from lung cancer radiotherapy planning scans predicts mortality. JCO Clin Cancer Inform. https://doi.org/10.1200/cci.21.00095
Aybay MN, Peker A, Keskin M et al (2021) Ordinal scoring of coronary artery calcification by computed tomography pulmonary angiography in acute pulmonary embolism. J Comput Assist Tomogr 45:863–869. https://doi.org/10.1097/RCT.0000000000001199
Azour L, Kadoch MA, Ward TJ et al (2017) Estimation of cardiovascular risk on routine chest CT: Ordinal coronary artery calcium scoring as an accurate predictor of Agatston score ranges. J Cardiovasc Comput Tomogr 11:8–15. https://doi.org/10.1016/j.jcct.2016.10.001
Bailey G, Healy A, Young BD et al (2017) Relative predictive value of lung cancer screening CT versus myocardial perfusion attenuation correction CT in the evaluation of coronary calcium. PLoS One 12:e0175678. https://doi.org/10.1371/journal.pone.0175678
Barda N, Dagan N, Stemmer A et al (2022) Improving cardiovascular disease prediction using automated coronary artery calcium scoring from existing chest CTs. J Digit Imaging 35:962–969. https://doi.org/10.1007/s10278-021-00575-7
Blair KJ, Allison MA, Morgan C et al (2014) Comparison of ordinal versus Agatston coronary calcification scoring for cardiovascular disease mortality in community-living individuals. Int J Cardiovasc Imaging 30:813–818. https://doi.org/10.1007/s10554-014-0392-1
Balakrishnan R, Nguyen B, Raad R et al (2017) Coronary artery calcification is common on nongated chest computed tomography imaging. Clin Cardiol 40:498–502. https://doi.org/10.1002/clc.22685
Budoff MJ, Nasir K, Kinney GL et al (2011) Coronary artery and thoracic calcium on noncontrast thoracic CT scans: Comparison of ungated and gated examinations in patients from the COPD Gene cohort. J Cardiovasc Comput Tomogr 5:113–118. https://doi.org/10.1016/j.jcct.2010.11.002
Callaway MP, Richards P, Goddard P, Rees M (1997) The incidence of coronary artery calcification on standard thoracic CT scans. Br J Radiol 70:572–574. https://doi.org/10.1259/bjr.70.834.9227248
Castagna F, Miles J, Arce J et al (2022) Visual coronary and aortic calcium scoring on chest computed tomography predict mortality in patients with low-density lipoprotein-cholesterol ≥190 mg/dL. Circ Cardiovasc Imaging 15:e014135. https://doi.org/10.1161/CIRCIMAGING.122.014135
Chamberlin J, Kocher MR, Waltz J et al (2021) Automated detection of lung nodules and coronary artery calcium using artificial intelligence on low-dose CT scans for lung cancer screening: accuracy and prognostic value. BMC Med 19:55. https://doi.org/10.1186/s12916-021-01928-3
Chandra D, Gupta A, Leader JK et al (2017) Assessment of coronary artery calcium by chest CT compared with EKG-gated cardiac CT in the multicenter AIDS cohort study. PLoS One 12:e0176557. https://doi.org/10.1371/journal.pone.0176557
Chandra D, Gupta A, Kinney GL et al (2021) The association between lung hyperinflation and coronary artery disease in smokers. Chest 160:858–871. https://doi.org/10.1016/j.chest.2021.04.066
Chen L, Vavrenyuk A, Ren JH et al (2021) Prognostic value of coronary artery calcification identified by the semi-quantitative weston method in the emergency room or other hospitalized patients. Front Cardiovasc Med 8. https://doi.org/10.3389/fcvm.2021.684292
Chen Y, Hu Z, Li M et al (2019) Comparison of nongated chest CT and dedicated calcium scoring CT for coronary calcium quantification using a 256-dector row CT scanner. Acad Radiol 26:e267–e274. https://doi.org/10.1016/j.acra.2018.12.005
Chi JM, Makaryus JN, Rahmani N et al (2021) Coronary CT calcium score in patients with prior nongated CT, is it necessary? Curr Probl Diagn Radiol 50:54–58. https://doi.org/10.1067/j.cpradiol.2019.07.011
Choy G, Kröpil P, Scherer A et al (2013) Pertinent reportable incidental cardiac findings on chest CT without electrocardiography gating: review of 268 consecutive cases. Acta Radiol 54:396–400. https://doi.org/10.1177/0284185113475918
de Mattos JN, Santiago Escovar CE, Zereu M et al (2022) Computed tomography on lung cancer screening is useful for adjuvant comorbidity diagnosis in developing countries. ERJ Open Res 8:00061–02022. https://doi.org/10.1183/23120541.00061-2022
Dirrichs T, Penzkofer T, Reinartz SD et al (2015) Extracoronary thoracic and coronary artery calcifications on chest CT for lung cancer screening. Acad Radiol 22:880–889. https://doi.org/10.1016/j.acra.2015.03.005
Douthit NT, Wyatt N, Schwartz B (2021) Clinical impact of reporting coronary artery calcium scores of non-gated chest computed tomography on statin management. Cureus. https://doi.org/10.7759/cureus.14856
Einstein AJ, Johnson LL, Bokhari S et al (2010) Agreement of visual estimation of coronary artery calcium from low-dose CT attenuation correction scans in hybrid PET/CT and SPECT/CT with standard agatston score. J Am Coll Cardiol 56:1914–1921. https://doi.org/10.1016/j.jacc.2010.05.057
Ezponda A, Casanova C, Divo M et al (2022) Chest CT‐assessed comorbidities and all‐cause mortality risk in COPD patients in the BODE cohort. Respirology 27:286–293. https://doi.org/10.1111/resp.14223
Fan R, Shi X, Qian Y et al (2018) Optimized categorization algorithm of coronary artery calcification score on non-gated chest low-dose CT screening using iterative model reconstruction technique. Clin Imaging 52:287–291. https://doi.org/10.1016/j.clinimag.2018.08.015
Foley PWX, Hamaad A, El-Gendi H, Leyva F (2010) Incidental cardiac findings on computed tomography imaging of the thorax. BMC Res Notes 3:326 https://doi.org/10.1186/1756-0500-3-326
Fresno CU, Tijmes FS, Thavendiranathan P et al (2022) Visual ordinal scoring of coronary artery calcium on contrast-enhanced and noncontrast chest CT: a retrospective study of diagnostic performance and prognostic utility. AJR Am J Roentgenol 219:569–578. https://doi.org/10.2214/AJR.22.27664
Gazourian L, Regis SM, Pagura EJ et al (2021) Qualitative coronary artery calcification scores and risk of all cause, COPD and pneumonia hospital admission in a large CT lung cancer screening cohort. Respir Med 186:106540. https://doi.org/10.1016/j.rmed.2021.106540
Gernaat SAM, van Velzen SGM, Koh V et al (2018) Automatic quantification of calcifications in the coronary arteries and thoracic aorta on radiotherapy planning CT scans of Western and Asian breast cancer patients. Radiother Oncol 127:487–492. https://doi.org/10.1016/j.radonc.2018.04.011
Gernaat SAM, Išgum I, de Vos BD et al (2016) Automatic coronary artery calcium scoring on radiotherapy planning CT scans of breast cancer patients: Reproducibility and association with traditional cardiovascular risk factors. PLoS One 11:e0167925. https://doi.org/10.1371/journal.pone.0167925
Gupta VA, Sousa M, Kraitman N et al (2018) Coronary artery calcification predicts cardiovascular complications after sepsis. J Crit Care 44:261–266. https://doi.org/10.1016/j.jcrc.2017.11.038
Hashimoto H, Nakanishi R, Mizumura S et al (2021) Prognostic values of coronary artery calcium score and 123I-BMIPP SPECT in patients with non-ischemic heart failure with preserved ejection fraction. Int J Cardiovasc Imaging 37:3573–3581. https://doi.org/10.1007/s10554-021-02332-x
Heidinger BH, DaBreo D, Kirkbride R et al (2020) Risk assessment of acute pulmonary embolism utilizing coronary artery calcifications in patients that have undergone CT pulmonary angiography and transthoracic echocardiography. Eur Radiol. https://doi.org/10.1007/s00330-020-07385-5
Hiltunen A, Kivisaari L, Leino-Arjas P, Vehmas T (2008) Visual scoring of atherosclerosis in chest computed tomography: findings among male construction workers. Acta Radiol 49:328–336. https://doi.org/10.1080/02841850701870914
Htwe Y, Cham MD, Henschke CI et al (2015) Coronary artery calcification on low-dose computed tomography: comparison of Agatston and Ordinal Scores. Clin Imaging 39:799–802. https://doi.org/10.1016/j.clinimag.2015.04.006
Huang Y-L, Wu F-Z, Wang Y-C et al (2013) Reliable categorisation of visual scoring of coronary artery calcification on low-dose CT for lung cancer screening: validation with the standard Agatston score. Eur Radiol 23:1226–1233. https://doi.org/10.1007/s00330-012-2726-5
Hughes-Austin JM, Dominguez A III, Allison MA et al (2016) Relationship of coronary calcium on standard chest CT scans with mortality. JACC Cardiovasc Imaging 9:152–159. https://doi.org/10.1016/j.jcmg.2015.06.030
Hutt A, Duhamel A, Deken V et al (2016) Coronary calcium screening with dual-source CT: reliability of ungated, high-pitch chest CT in comparison with dedicated calcium-scoring CT. Eur Radiol 26:1521–1528. https://doi.org/10.1007/s00330-015-3978-7
Itani Y, Sone S, Nakayama T et al (2004) Coronary artery calcification detected by a mobile helical computed tomography unit and future cardiovascular death: 4-year follow-up of 6120 asymptomatic Japanese. Heart Vessels 19:161–163. https://doi.org/10.1007/s00380-003-0759-z
Jacobs PC, Gondrie MJ, Mali WP et al (2011) Unrequested information from routine diagnostic chest CT predicts future cardiovascular events. Eur Radiol 21:1577–1585. https://doi.org/10.1007/s00330-011-2112-8
Johnson C, Khalilzadeh O, Novelline RA, Choy G (2014) Coronary artery calcification is often not reported in pulmonary CT angiography in patients with suspected pulmonary embolism: An opportunity to improve diagnosis of acute coronary syndrome. AJR Am J Roentgenol 202:725–729. https://doi.org/10.2214/AJR.13.11326
Khan A, Mond DJ, Kallman CE et al (1994) Computed tomography of normal and calcified coronary arteries. J Thorac Imaging 9:1–7. https://doi.org/10.1097/00005382-199424000-00001
Kim YK, Sung YM, Cho SH et al (2014) Reliability analysis of visual ranking of coronary artery calcification on low-dose CT of the thorax for lung cancer screening: comparison with ECG-gated calcium scoring CT. Int J Cardiovasc Imaging 30:81–87. https://doi.org/10.1007/s10554-014-0507-8
Kim SM, Chung MJ, Lee KS et al (2008) Coronary calcium screening using low-dose lung cancer screening: Effectiveness of MDCT with retrospective reconstruction. AJR Am J Roentgenol 190:917–922. https://doi.org/10.2214/AJR.07.2979
Kirsch J, Buitrago I, Mohammed T-LH et al (2012) Detection of coronary calcium during standard chest computed tomography correlates with multi-detector computed tomography coronary artery calcium score. Int J Cardiovasc Imaging 28:1249–1256. https://doi.org/10.1007/s10554-011-9928-9
Krishnam M, Chae EJ, Hernandez-Rangel E et al (2020) Utility of routine non-gated CT chest in detection of subclinical atherosclerotic calcifications of coronary arteries in hospitalised HIV patients. Br J Radiol 93:20190462. https://doi.org/10.1259/bjr.20190462
Kucharczyk MJ, Menezes RJ, McGregor A et al (2011) Assessing the impact of incidental findings in a lung cancer screening study by using low-dose computed tomography. Can Assoc Radiol J 62:141–145. https://doi.org/10.1016/j.carj.2010.02.008
Lai Y-H, Chen HHW, Tsai Y-S (2021) Accelerated coronary calcium burden in breast cancer patients after radiotherapy: a comparison with age and race matched healthy women. Radiat Oncol 16:210. https://doi.org/10.1186/s13014-021-01936-w
Lee S, Suh YJ, Nam K et al (2021) Comparison of artery-based methods for ordinal grading of coronary artery calcium on low-dose chest computed tomography. Eur Radiol 31:8108–8115. https://doi.org/10.1007/s00330-021-07987-7
Lee SY, Kim TH, Han K et al (2021) Feasibility of coronary artery calcium scoring on dual-energy chest computed tomography: A prospective comparison with electrocardiogram-gated calcium score computed tomography. J Clin Med 10:653. https://doi.org/10.3390/jcm10040653
Lessmann N, de Jong PA, Celeng C et al (2019) Sex differences in coronary artery and thoracic aorta calcification and their association with cardiovascular mortality in heavy smokers. JACC Cardiovasc Imaging 12:1808–1817. https://doi.org/10.1016/j.jcmg.2018.10.026
Lichtenstein G, Perlman A, Shpitzen S et al (2018) Correlation between coronary artery calcification by non-cardiac CT and Framingham score in young patients. PLoS One 13:e0195061. https://doi.org/10.1371/journal.pone.0195061
Liu Y, Chen X, Liu X et al (2022) Accuracy of non-gated low-dose non-contrast chest CT with tin filtration for coronary artery calcium scoring. Eur J Radiol Open 9:100396. https://doi.org/10.1016/j.ejro.2022.100396
Machino R, Shimoyama K, Oku K et al (2023) Prevalence of coronary calcification on preoperative computed tomography and its management in thoracic surgery. Surg Today 53:62–72. https://doi.org/10.1007/s00595-022-02532-5
MacRedmond R, Logan PM, Lee M et al (2004) Screening for lung cancer using low dose CT scanning. Thorax 59:237–241. https://doi.org/10.1136/thx.2003.008821
Majeed A, Ruane B, Shusted CS et al (2022) Frequency of statin prescription among individuals with coronary artery calcifications detected through lung cancer screening. Am J Med Qual 37:388–395. https://doi.org/10.1097/JMQ.0000000000000053
Mascalchi M, Puliti D, Romei C et al (2021) Moderate-severe coronary calcification predicts long-term cardiovascular death in CT lung cancer screening: The ITALUNG trial. Eur J Radiol 145:110040. https://doi.org/10.1016/j.ejrad.2021.110040
McConachie P, McKay E, Crane A et al (2022) Accurate measurement of coronary artery calcium in cancer patients using the CT component of PET/CT scans. Nucl Med Commun 43:159–165. https://doi.org/10.1097/MNM.0000000000001503
Mendoza DP, Kako B, Digumarthy SR et al (2020) Impact of significant coronary artery calcification reported on low-dose computed tomography lung cancer screening. J Thorac Imaging 35:129–135. https://doi.org/10.1097/RTI.0000000000000458
Mets OM, Vliegenthart R, Gondrie MJ et al (2013) Lung cancer screening CT-based prediction of cardiovascular events. JACC Cardiovasc Imaging 6:899–907. https://doi.org/10.1016/j.jcmg.2013.02.008
Muller L, Sewchuran T, Durand M (2021) Prevalence of incidental premature cardiac calcifications in an HIV-infected South African population using conventional computed tomography chest radiography. South Afr J HIV Med 22:1241. https://doi.org/10.4102/sajhivmed.v22i1.1241
Niedermeier S, Wania R, Lampart A et al (2022) Incidental CT findings in the elderly with low-energy falls: Prevalence and implications. Diagnostics (Basel) 12:354. https://doi.org/10.3390/diagnostics12020354
Nguyen PTH, Coche E, Goffin E et al (2007) Prevalence and determinants of coronary and aortic calcifications assessed by chest CT in renal transplant recipients. Am J Nephrol 27:329–335. https://doi.org/10.1159/000102978
OʼHare PE, Ayres JF, OʼRourke RL et al (2014) Coronary artery calcification on computed tomography correlates with mortality in chronic obstructive pulmonary disease. J Comput Assist Tomogr 38:753–759. https://doi.org/10.1097/rct.0000000000000119
Ohmoto-Sekine Y, Yanagibori R, Amakawa K et al (2016) Prevalence and distribution of coronary calcium in asymptomatic Japanese subjects in lung cancer screening computed tomography. J Cardiol 67:449–454. https://doi.org/10.1016/j.jjcc.2015.06.010
Ota K, Nakanishi R, Hashimoto H et al (2022) Association between coronary artery calcium score on non-contrast chest computed tomography and all-cause mortality among patients with congestive heart failure. Heart Vessels 37:262–272. https://doi.org/10.1007/s00380-021-01906-y
Phillips WJ, Johnson C, Law A et al (2019) Comparison of framingham risk score and chest-CT identified coronary artery calcification in breast cancer patients to predict cardiovascular events. Int J Cardiol 289:138–143. https://doi.org/10.1016/j.ijcard.2019.01.056
Phillips WJ, Johnson C, Law A et al (2018) Reporting of coronary artery calcification on chest CT studies in breast cancer patients at high risk of cancer therapy related cardiac events. Int J Cardiol Heart Vasc 18:12–16. https://doi.org/10.1016/j.ijcha.2018.02.001
Pieszko K, Shanbhag AD, Lemley M et al (2022) Reproducibility of quantitative coronary calcium scoring from PET/CT attenuation maps: comparison to ECG-gated CT scans. Eur J Nucl Med Mol Imaging 49:4122–4132. https://doi.org/10.1007/s00259-022-05866-x
Priola AM, Priola SM, Giaj-Levra M et al (2013) Clinical implications and added costs of incidental findings in an early detection study of lung cancer by using low-dose spiral computed tomography. Clin Lung Cancer 14:139–148. https://doi.org/10.1016/j.cllc.2012.05.005
Ramchand J, Bansal A, Saeedan MB et al (2021) Incidental thoracic aortic dilation on chest computed tomography in patients with atrial fibrillation. Am J Cardiol 140:78–82. https://doi.org/10.1016/j.amjcard.2020.10.059
Rasmussen T, Kober L, Abdulla J et al (2015) Coronary artery calcification detected in lung cancer screening predicts cardiovascular death. Scand Cardiovasc J 49:159–167. https://doi.org/10.3109/14017431.2015.1039572
Reiter MJ, Nemesure A, Madu E et al (2018) Frequency and distribution of incidental findings deemed appropriate for S modifier designation on low-dose CT in a lung cancer screening program. Lung Cancer 120:1–6. https://doi.org/10.1016/j.lungcan.2018.03.017
Rodriguez-Granillo GA, Reynoso E, Capunay C et al (2017) Impact on mortality of coronary and non-coronary cardiovascular findings in non-gated thoracic CT by malignancy status. Eur J Radiol 93:169–177. https://doi.org/10.1016/j.ejrad.2017.05.030
Roehl AB, Hein M, Kroencke J et al (2021) Cardiovascular evaluation of liver transplant patients by using coronary calcium scoring in ECG-synchronized computed tomographic scans. J Clin Med 10:5148. https://doi.org/10.3390/jcm10215148
Roth BJ, Meyer CA (1997) Coronary artery calcification at CT as a predictor for cardiac complications of thoracic surgery. J Comput Assist Tomogr 21:619–622. https://doi.org/10.1097/00004728-199707000-00018
Schiffer WB, Deych E, Lenihan DJ, Zhang KW (2021) Coronary and aortic calcification are associated with cardiovascular events on immune checkpoint inhibitor therapy. Int J Cardiol 322:177–182. https://doi.org/10.1016/j.ijcard.2020.08.024
Secchi F, Di Leo G, Zanardo M et al (2017) Detection of incidental cardiac findings in noncardiac chest computed tomography. Medicine (Baltimore) 96:e7531. https://doi.org/10.1097/MD.0000000000007531
Selvaraj S, Khan MS, Vidula MK et al (2021) Incremental prognostic value of visually estimated coronary artery calcium in patients undergoing positron emission tomography imaging. Open Heart 8:e001648. https://doi.org/10.1136/openhrt-2021-001648
Shao L, Yan AT, Lebovic G et al (2017) Prognostic value of visually detected coronary artery calcification on unenhanced non-gated thoracic computed tomography for prediction of non-fatal myocardial infarction and all-cause mortality. J Cardiovasc Comput Tomogr 11:196–202. https://doi.org/10.1016/j.jcct.2017.03.004
Shemesh J, Henschke CI, Shaham D et al (2010) Ordinal scoring of coronary artery calcifications on low-dose CT scans of the chest is predictive of death from cardiovascular disease. Radiology 257:541–548. https://doi.org/10.1148/radiol.10100383
Shemesh J, Henschke CI, Farooqi A et al (2006) Frequency of coronary artery calcification on low-dose computed tomography screening for lung cancer. Clin Imaging 30:181–185. https://doi.org/10.1016/j.clinimag.2005.11.002
Shipe ME, Maiga AW, Deppen SA et al (2021) Preoperative coronary artery calcifications in veterans predict higher all-cause mortality in early-stage lung cancer: a cohort study. J Thorac Dis 13:1427–1433. https://doi.org/10.21037/jtd-20-2102
Souza VF, dos Santos AASMD, Mesquita CT et al (2020) Quantification of calcified coronary plaques by chest computed tomography: correlation with the calcium score technique. Arq Bras Cardiol 115:493–500. https://doi.org/10.36660/abc.20190235
Suh YJ, Lee JW, Shin SY, et al (2020) Coronary artery calcium severity grading on non-ECG-gated low-dose chest computed tomography: a multiple-observer study in a nationwide lung cancer screening registry. Eur Radiol 30:. https://doi.org/10.1007/s00330-020-06707-x
Sverzellati N, Cademartiri F, Bravi F et al (2012) Relationship and prognostic value of modified coronary artery calcium score, FEV1, and emphysema in lung cancer screening population: the MILD trial. Radiology 262:460–467. https://doi.org/10.1148/radiol.11110364
Tahir I, Marquardt JP, Mercaldo ND et al (2022) Utility of noncancerous chest CT features for predicting overall survival and noncancer death in patients with stage I lung cancer treated with stereotactic body radiotherapy. AJR Am J Roentgenol 219:579–589. https://doi.org/10.2214/AJR.22.27484
Takei N, Suzuki M, Tanabe N et al (2021) Combined assessment of pulmonary arterial enlargement and coronary calcification predicts the prognosis of patients with chronic obstructive pulmonary disease. Respir Med 185:106520. https://doi.org/10.1016/j.rmed.2021.106520
Trpkov C, Savtchenko A, Liang Z et al (2021) Visually estimated coronary artery calcium score improves SPECT-MPI risk stratification. Int J Cardiol Heart Vasc 35:100827. https://doi.org/10.1016/j.ijcha.2021.100827
Uretsky S, Chokshi N, Kobrinski T et al (2015) The interplay of physician awareness and reporting of incidentally found coronary artery calcium on the clinical management of patients who underwent noncontrast chest computed tomography. Am J Cardiol 115:1513–1517. https://doi.org/10.1016/j.amjcard.2015.02.051
van Assen M, Martin SS, Varga-Szemes A et al (2021) Automatic coronary calcium scoring in chest CT using a deep neural network in direct comparison with non-contrast cardiac CT: A validation study. Eur J Radiol 134:109428. https://doi.org/10.1016/j.ejrad.2020.109428
van der Bijl N, Klok FA, Huisman M v et al (2016) Coronary or thoracic artery calcium score in provoked and unprovoked pulmonary embolism: a case-control study. J Thrombos Haemost 14:931–935. https://doi.org/10.1111/jth.13289
Velangi PS, Kenny B, Hooks M et al (2021) Impact of 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncardiac chest CT scans on lung cancer screening CT reporting. Int J Cardiovasc Imaging 37:2777–2784. https://doi.org/10.1007/s10554-021-02241-z
Wang X, Xin R, Shan D et al (2022) Incremental value of noncontrast chest computed tomography-derived parameters in predicting subclinical carotid atherosclerosis: from the PERSUADE study. J Thorac Imaging. https://doi.org/10.1097/RTI.0000000000000655
Wang K, Malkin HE, Patchett ND et al (2022) Coronary artery calcifications and cardiac risk after radiation therapy for stage III lung cancer. Int J Radiat Oncol Biol Phys 112:188–196. https://doi.org/10.1016/j.ijrobp.2021.08.017
Wenning C, Vrachimis A, Pavenstädt H-J et al (2021) Coronary artery calcium burden, carotid atherosclerotic plaque burden, and myocardial blood flow in patients with end-stage renal disease: A non-invasive imaging study combining PET/CT and 3D ultrasound. J Nucl Cardiol 28:2660–2670. https://doi.org/10.1007/s12350-020-02080-w
West BH, Low CG, Bista BB et al (2019) Significance of coronary artery calcium found on non–electrocardiogram-gated computed tomography during preoperative evaluation for liver transplant. Am J Cardiol 124:278–284 https://doi.org/10.1016/j.amjcard.2019.04.025
Williams MC, van Beek EJR, Hill AT, Murchison JT (2021) Coronary artery calcification on thoracic computed tomography is an independent predictor of mortality in patients with bronchiectasis. J Thorac Imaging 36:166–173. https://doi.org/10.1097/RTI.0000000000000553
Williams MC, Murchison JT, Edwards LD et al (2014) Coronary artery calcification is increased in patients with COPD and associated with increased morbidity and mortality. Thorax 69:718–723. https://doi.org/10.1136/thoraxjnl-2012-203151
Williams MC, Morley NCD, Muir KC et al (2019) Coronary artery calcification is associated with mortality independent of pulmonary embolism severity: a retrospective cohort study. Clin Radiol 74:973.e7-973.e14. https://doi.org/10.1016/j.crad.2019.08.023
Williams KA Sr, Kim JT, Holohan KM (2013) Frequency of unrecognized, unreported, or underreported coronary artery and cardiovascular calcification on noncardiac chest CT. J Cardiovasc Comput Tomogr 7:167–172. https://doi.org/10.1016/j.jcct.2013.05.003
Wu M-T, Yang P, Huang Y-L et al (2008) Coronary arterial calcification on low-dose ungated MDCT for lung cancer screening: Concordance study with dedicated cardiac CT. AJR Am J Roentgenol 190:923–928. https://doi.org/10.2214/AJR.07.2974
Xia C, Vonder M, Pelgrim GJ et al (2020) High-pitch dual-source CT for coronary artery calcium scoring: a head-to-head comparison of non-triggered chest versus triggered cardiac acquisition: High-pitch chest versus cardiac CT for calcium scoring. J Cardiovasc Comput Tomogr. https://doi.org/10.1016/j.jcct.2020.04.013
Yang X, Jiang Y, Xie M et al (2022) Nongated computed tomography predicts perioperative cardiovascular risk in lung cancer surgery. Ann Thorac Surg 114:2050–2057. https://doi.org/10.1016/j.athoracsur.2022.04.023
Yu C, Ng ACC, Ridley L et al (2021) Incidentally identified coronary artery calcium on non-contrast CT scan of the chest predicts major adverse cardiac events among hospital inpatients. Open Heart 8:e001695. https://doi.org/10.1136/openhrt-2021-001695
Zimmermann GS, Fingerle AA, Müller-Leisse C et al (2020) Coronary calcium scoring assessed on native screening chest CT imaging as predictor for outcome in COVID-19: An analysis of a hospitalized German cohort. PLoS One 15:e0244707. https://doi.org/10.1371/journal.pone.0244707
Zorzi A, Brunetti G, Cardaioli F et al (2021) Coronary artery calcium on standard chest computed tomography predicts cardiovascular events after liver transplantation. Int J Cardiol 339:219–224. https://doi.org/10.1016/j.ijcard.2021.06.046
Agatston AS, Janowitz WR, Hildner FJ et al (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. https://doi.org/10.1016/0735-1097(90)90282-T
Jensen JC, Dardari ZA, Blaha MJ et al (2020) Association of Body Mass Index With Coronary Artery Calcium and Subsequent Cardiovascular Mortality. Circulation: Cardiovascular Imaging 13:e009495 https://doi.org/10.1161/CIRCIMAGING.119.009495
Altintas S, van Workum S, Kok M et al (2023) BMI is not independently associated with coronary artery calcification in a large single‐center CT cohort. Obes Sci Pract 9:172–178. https://doi.org/10.1002/osp4.636
Kovacic JC, Lee P, Baber U et al (2012) Inverse relationship between body mass index and coronary artery calcification in patients with clinically significant coronary lesions. Atherosclerosis 221:176–182. https://doi.org/10.1016/j.atherosclerosis.2011.11.020
Wetscherek MTA, McNaughton E, Majcher V et al (2023) Incidental coronary artery calcification on non-gated CT thorax correlates with risk of cardiovascular events and death. Eur Radiol 33:4723–4733. https://doi.org/10.1007/s00330-023-09428-z
Valenti V, Ó Hartaigh B, Heo R et al (2015) A 15-year warranty period for asymptomatic individuals without coronary artery calcium: a prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging 8:900–909. https://doi.org/10.1016/j.jcmg.2015.01.025
Sarwar A, Shaw LJ, Shapiro MD et al (2009) Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2:675–688. https://doi.org/10.1016/j.jcmg.2008.12.031
Graby J, Soto-Hernaez J, Murphy D, et al (2023) Coronary artery calcification on routine CT has prognostic and treatment implications for all ages. Clin Radiol 78:412–420. https://doi.org/10.1016/j.crad.2023.02.007
Funding
Michelle C. Williams (FS/ICRF/20/26002) is supported by the British Heart Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor for this publication is Michelle C. Williams.
Conflicts of interest
The authors of this manuscript declare relationships with the following companies:
Michelle C. Williams has given talks for Canon Medical Systems, Siemens Healthineers and Novartis.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Informed consent was not required for this study.
Ethical approval
Institutional Review Board approval was not required because this is a systematic review and meta-analysis.
Study subjects or cohorts overlap
When multiple publications based on the same trial were identified, only the largest sample size was included to avoid duplicate reporting.
Methodology
-
Systematic review and meta-analysis
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Osborne-Grinter, M., Ali, A. & Williams, M.C. Prevalence and clinical implications of coronary artery calcium scoring on non-gated thoracic computed tomography: a systematic review and meta-analysis. Eur Radiol 34, 4459–4474 (2024). https://doi.org/10.1007/s00330-023-10439-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10439-z