Abstract
Objectives
Adipose tissue radiodensity in computed tomography (CT) performed before surgeries can predict surgical difficulty. Despite its clinical importance, little is known about what influences radiodensity. This study combines desorption electrospray ionization mass spectrometry imaging (DESI-MSI) and electrospray ionization (ESI) with machine learning to unveil how chemical composition of adipose tissue determines its radiodensity.
Methods
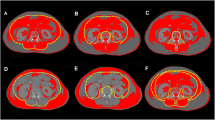
Patients in the study underwent abdominal surgeries. Before surgery, CT radiodensity of fat near operated sites was measured. Fifty-three fat samples were collected and analyzed by DESI-MSI, ESI, and histology, and then sorted by radiodensity, demographic parameters, and adipocyte size. A non-negative matrix factorization (NMF) algorithm was developed to differentiate between high and low radiodensities.
Results
No associations between radiodensity and patient age, gender, weight, height, or fat origin were found. Body mass index showed negative correlation with radiodensity. A substantial difference in chemical composition between adipose tissues of high and low radiodensities was observed. More radiodense tissues exhibited greater abundance of high molecular weight species, such as phospholipids of various types, ceramides, cholesterol esters and diglycerides, and about 70% smaller adipocyte size. Less radiodense tissue showed high abundance of short acyl-tail fatty acids.
Conclusions
This study unveils the connection between abdominal adipose tissue radiodensity and its chemical composition. Because the radiodensity of the fat around the surgical site is associated with surgical difficulty, it is important to understand how adipose tissue composition affects this parameter. We conclude that fat tissue with a higher content of various phospholipids and waxy lipids is more CT radiodense.
Clinical relevance statement
This study establishes the connection between the CT radiodensity of adipose tissue and its chemical composition. Clinicians may use this information for preoperative planning of surgical procedures, potentially modifying their surgical approach (for example, performing partial nephrectomy openly rather than laparoscopically).
Key Points
• Adipose tissue radiodensity values in computed tomography images taken prior to the surgery can potentially predict surgery difficulty.
• Fifty-three human specimens were analyzed by advanced mass spectrometry, molecular imaging, and machine learning to establish the key features that determine Hounsfield units’ values of adipose tissue.
• The findings of this research will enable clinicians to better prepare for surgical procedures and select operative strategies.
Graphical abstract







Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CNN:
-
Convolutional neural networks
- CT:
-
Computed tomography
- DESI-MSI:
-
Desorption electrospray ionization mass spectrometry imaging
- ESI:
-
Electrospray ionization
- FWHM:
-
Full width at half maximum
- H&E:
-
Hematoxylin and eosin
- HCD:
-
Higher energy collisional dissociation
- HU:
-
Hounsfield units
- LC-MS:
-
Liquid chromatography–mass spectrometry
- LR:
-
Linear regression
- m/z :
-
Mass to charge ratio
- ML:
-
Machine learning
- MS:
-
Mass spectrometry
- MSE:
-
Mean square error
- NMF:
-
Non-negative matrix factorization algorithm
- Q-TOF:
-
Quadrupole time-of-flight
- SD:
-
Standard deviation
- SIM:
-
Selected ion monitoring
References
Lamvu G, Zolnoun D, Boggess J, Steege JF (2004) Obesity: physiologic changes and challenges during laparoscopy. Am J Obstet Gynecol 191(2):669–674
McIlwaine K, Manwaring J, Ellett L et al (2014) The effect of patient body mass index on surgical difficulty in gynaecological laparoscopy. Aust N Z J Obstet Gynaecol 54(6):564–569
Feliciano EMC, Winkels RM, Meyerhardt JA, Prado CM, Afman LA, Caan BJ (2021) Abdominal adipose tissue radiodensity is associated with survival after colorectal cancer. Am J Clin Nutr 114(6):1917–1924
Brown JC, Caan BJ, Meyerhardt JA et al (2018) The deterioration of muscle mass and radiodensity is prognostic of poor survival in stage I-III colorectal cancer: a population-based cohort study (C-SCANS). J Cachexia Sarcopenia Muscle 9(4):664–672
Murphy RA, Register TC, Shively CA et al (2014) Adipose tissue density, a novel biomarker predicting mortality risk in older adults. J Gerontol A Biol Sci Med Sci 69(1):109–117
Shah RV, Allison MA, Lima JA et al (2016) Abdominal fat radiodensity, quantity and cardiometabolic risk: the Multi-Ethnic Study of Atherosclerosis. Nutr Metab Cardiovasc Dis 26(2):114–122
Kwon SS, Choi K, Da Nam B et al (2021) Epicardial adipose tissue radiodensity is associated with all-cause mortality in patients undergoing hemodialysis. Sci Rep 11(1):23090
Tilves C, Zmuda JM, Kuipers AL et al (2020) Associations of thigh and abdominal adipose tissue radiodensity with glucose and insulin in nondiabetic African-ancestry men. Obesity 28(2):404–411
Kim WH, Kim CG, Kim DW (2012) Optimal CT number range for adipose tissue when determining lean body mass in whole-body F-18 FDG PET/CT studies. Nucl Med Mol Imaging 46(4):294–299
Kim YJ, Lee SH, Kim TY, Park JY, Choi SH, Kim KG (2013) Body fat assessment method using CT images with separation mask algorithm. J Digit Imaging 26(2):155–162
Din MU, Raiko J, Saari T et al (2017) Human brown fat radiodensity indicates underlying tissue composition and systemic metabolic health. J Clin Endocrinol Metab 102(7):2258–2267
Starekova J, Reeder SB (2020) Liver fat quantification: where do we stand? Abdom Radiol (NY) 45(11):3386–3399
Bhullar AS, Anoveros-Barrera A, Dunichand-Hoedl A et al (2020) Lipid is heterogeneously distributed in muscle and associates with low radiodensity in cancer patients. J Cachexia Sarcopenia Muscle 11(3):735–747
Ebadi M, Dunichand-Hoedl AR, Rider E et al (2022) Higher subcutaneous adipose tissue radiodensity is associated with increased mortality in patients with cirrhosis. JHEP Rep 4(7):100495
Wiseman JM, Ifa DR, Song Q, Cooks RG (2006) Tissue imaging at atmospheric pressure using desorption electrospray ionization (DESI) mass spectrometry. Angew Chem Int Ed 45(43):7188–7192
Margulis K, Chiou AS, Aasi SZ, Tibshirani RJ, Tang JY, Zare RN (2018) Distinguishing malignant from benign microscopic skin lesions using desorption electrospray ionization mass spectrometry imaging. Proc Natl Acad Sci U S A 115(25):6347
Leuschner J, Schmidt M, Fernsel P, Lachmund D, Boskamp T, Maass P (2018) Supervised non-negative matrix factorization methods for MALDI imaging applications. Bioinformatics 35(11):1940–1947
Boskamp T, Lachmund D, Oetjen J et al (2017) A new classification method for MALDI imaging mass spectrometry data acquired on formalin-fixed paraffin-embedded tissue samples. Biochim Biophys Acta Proteins Proteom 1865(7):916–926
Nijs M, Smets T, Waelkens E, De Moor B (2021) A mathematical comparison of non-negative matrix factorization related methods with practical implications for the analysis of mass spectrometry imaging data. Rapid Commun Mass Spectrom 35(21):e9181
Keenan MR, Kotula PG (2004) Accounting for Poisson noise in the multivariate analysis of ToF-SIMS spectrum images. Surf Interface Anal 36(3):203–212
Deepaisarn S, Tar PD, Thacker NA, Seepujak A, McMahon AW (2018) Quantifying biological samples using linear Poisson independent component analysis for MALDI-ToF mass spectra. Bioinformatics 34(6):1001–1008
Piehowski PD, Davey AM, Kurczy ME et al (2009) Time-of-flight secondary ion mass spectrometry imaging of subcellular lipid heterogeneity: Poisson counting and spatial resolution. Anal Chem 81(14):5593–5602
Verbeeck N, Caprioli RM, Van de Plas R (2020) Unsupervised machine learning for exploratory data analysis in imaging mass spectrometry. Mass Spectrom Rev 39(3):245–291
Eberlin LS, Ferreira CR, Dill AL, Ifa DR, Cheng L, Cooks RG (2011) Nondestructive, histologically compatible tissue imaging by desorption electrospray ionization mass spectrometry. Chembiochem 12(14):2129–2132
Baba S, Jacene HA, Engles JM, Honda H, Wahl RL (2010) CT Hounsfield units of brown adipose tissue increase with activation: preclinical and clinical studies. J Nucl Med 51(2):246–250
Murano I, Barbatelli G, Parisani V et al (2008) Dead adipocytes, detected as crown-like structures, are prevalent in visceral fat depots of genetically obese mice. J Lipid Res 49(7):1562–1568
Ebadi M, Tandon P, Moctezuma-Velazquez C et al (2018) Low subcutaneous adiposity associates with higher mortality in female patients with cirrhosis. J Hepatol 69(3):608–616
Acknowledgements
This research was conducted using the Spatial Metabolomics Unit founded with the help of the Wolfson Foundation and the Wolfson Foundation Charity Trust (award reference PR/oys/jw/md/eh/22747/22641) and the Metabolomics Core Unit, Shared Research Facility, Faculty of Medicine-Hebrew University. This research was supported by Israel Science Foundation (grant number 1840/20), United States–Israel Binational Science Foundation (grant number 2019237), Israel Cancer Research Fund (grant number 20-204-RCDA), Council for Higher Education, Israel (Alon Fellowship), David R. Bloom Center for Pharmaceutical Sciences and The Alex Grass Center for Drug Design and Synthesis.
Funding
The authors state that this work has not received any funding in addition to the grants listed in the Acknowledgements.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is O. Gofrit.
Conflict of Interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and Biometry
One of the authors (E. Bentov-Arava) has significant statistical expertise.
No complex statistical methods were necessary for this paper.
Informed Consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical Approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
NA
Methodology
• Prospective
• Observational
• One Institution study
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zoabi, A., Bentov-Arava, E., Sultan, A. et al. Adipose tissue composition determines its computed tomography radiodensity. Eur Radiol 34, 1635–1644 (2024). https://doi.org/10.1007/s00330-023-09911-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09911-7