Abstract
Objective
The aim of this study was to assess whether aortic peak wall stress (PWS) and peak wall rupture index (PWRI) were associated with the risk of abdominal aortic aneurysm (AAA) rupture or repair (defined as AAA events) among participants with small AAAs.
Methods
PWS and PWRI were estimated from computed tomography angiography (CTA) scans of 210 participants with small AAAs (≥ 30 and ≤ 50 mm) prospectively recruited between 2002 and 2016 from two existing databases. Participants were followed for a median of 2.0 (inter-quartile range 1.9, 2.8) years to record the incidence of AAA events. The associations between PWS and PWRI with AAA events were assessed using Cox proportional hazard analyses. The ability of PWS and PWRI to reclassify the risk of AAA events compared to the initial AAA diameter was examined using net reclassification index (NRI) and classification and regression tree (CART) analysis.
Results
After adjusting for other risk factors, one standard deviation increase in PWS (hazard ratio, HR, 1.56, 95% confidence intervals, CI 1.19, 2.06; p = 0.001) and PWRI (HR 1.74, 95% CI 1.29, 2.34; p < 0.001) were associated with significantly higher risks of AAA events. In the CART analysis, PWRI was identified as the best single predictor of AAA events at a cut-off value of > 0.562. PWRI, but not PWS, significantly improved the classification of risk of AAA events compared to the initial AAA diameter alone.
Conclusion
PWS and PWRI predicted the risk of AAA events but only PWRI significantly improved the risk stratification compared to aortic diameter alone.
Key Points
• Aortic diameter is an imperfect measure of abdominal aortic aneurysm (AAA) rupture risk.
• This observational study of 210 participants found that peak wall stress (PWS) and peak wall rupture index (PWRI) predicted the risk of aortic rupture or AAA repair.
• PWRI, but not PWS, significantly improved the risk stratification for AAA events compared to aortic diameter alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abdominal aortic aneurysm (AAA) rupture is responsible for approximately 200,000 deaths per year worldwide [1,2,3]. Maximum AAA diameter is the most established method of estimating AAA rupture risk and is used by clinicians to help select patients for elective AAA repair [1]. Current guidelines recommend that small (< 55 mm diameter in men and < 50 mm in women) asymptomatic AAAs are managed conservatively while larger AAAs are considered for surgical repair [4]. Some large AAAs do not rupture during a patient’s lifetime [5], while 1–2% of small AAAs rupture per year [6], suggesting that AAA diameter is not a perfect measure of rupture risk. Other methods of estimating AAA rupture risk have been proposed including AAA volume, functional imaging (e.g., positron emission tomography), and circulating biomarkers; however, there has been limited uptake of these methods in clinical practice [7, 8]. More accurate and user-friendly methods to estimate AAA rupture risk could benefit patient management.
Finite element analysis (FEA) is an established engineering technique that can non-invasively estimate the peak tensile stress within the AAA wall (peak wall stress) from computed tomography images (Fig. 1) [9]. A recent prospective study reported that the dimensionless ratio of wall stress and wall strength (defined as the ABR) significantly predicted the risk of AAA rupture or repair (AAA events) independent of other risk factors [10]. The ABR was computed by FEA of three-dimensional CT images of the aorta and uniquely incorporated patient-specific aortic wall thickness estimates [11, 12]. Aortic wall thickness measurement required magnetic resonance imaging (MRI) which is not routinely performed in AAA management [10, 13]. Furthermore, the method employed in that study has not been widely studied [10, 13], and required multiple software packages to perform the biomechanical analysis [13].
A prior meta-analysis [9] found that the peak wall rupture index (PWRI, i.e., the ratio between aortic wall stress and strength estimated assuming a constant wall-thickness) [14, 15], but not peak wall stress (PWS), was significantly greater in ruptured than asymptomatic intact AAAs of similar diameter. Both measurements can be estimated from contrast-enhanced computed tomography angiograms (CTA) using one software package [15, 16] with good repeatability [9, 11, 17, 18]. The studies included in prior reviews [9, 19] were of cross-sectional design and ostensibly included patients with large AAAs. There is a lack of observational studies investigating the association between PWS and PWRI with the future risk of AAA events among individuals with small AAAs (maximum orthogonal aortic diameter of ≥ 30 and ≤ 50 mm) [10, 20]. Such data is required to assess whether PWS and PWRI can predict the risk of future AAA events amongst people with a low risk of AAA rupture [10, 20]. Furthermore, it is unclear whether PWS and PWRI can improve the classification of risk of AAA events in comparison to using AAA diameter alone. The primary objective of this prospective observational study was to assess whether baseline PWS and PWRI were independently associated with the risk of future AAA events among individuals with small AAAs. The secondary objective was to examine whether PWS and PWRI significantly improved the stratification of risk of AAA events over using AAA diameter alone.
Methods
Study design and participants
Participants were recruited from sites across Australia, the USA, and Netherlands between 29/05/2002 and 24/06/2016 via two sources. Firstly participants were included from those taking part in an ongoing multi-centre prospective cohort study of people with a range of peripheral vascular diseases [20, 21]. Secondly, participants were included from an international multi-centre trial of patients with small AAAs, which showed that telmisartan did not slow AAA growth, as previously reported [22]. Participants were eligible for the current study if they had a small infra-renal (maximum orthogonal aortic diameter of ≥ 30 and ≤ 50 mm) asymptomatic intact AAA which had been imaged by a CTA [11]. CTAs needed to have a slice thickness of 3 mm or less and visualise the whole infra-renal aorta including the bifurcation into the common iliac arteries [11]. Patients with symptomatic or ruptured AAAs were excluded. Written informed consent was obtained from all participants. The study was performed in accordance with the Helsinki declaration and ethical approval was granted from institutional ethics committees (HREC/09/QTHS/117; HREC/14/QTHS/203; HREC/13/QTHS/125) [21,22,23].
Participant characteristics
Risk factors and medication prescription records were collected at the time of enrolment into the study [21,22,23]. Coronary heart disease (CHD) was defined by a history of myocardial infarction, angina, or coronary revascularisation [24, 25]. Current smoking was defined as smoking within the last month based on participants’ history. Hypertension, diabetes, and chronic obstructive pulmonary disease (COPD) were defined by a prior diagnosis or treatment for these conditions [21,22,23]. Blood pressure was measured at recruitment using a digital monitor (Omron Intellisense, HEM-907) after participants had rested supine for a 20-min period [23, 26]. Prescriptions for aspirin, anticoagulants, statins, calcium channel blockers, beta-blockers, and metformin were obtained from medical records.
CTA
CTAs were performed using institutional scanners at each participating hospital with departmental-specific image acquisition protocols as previously reported [11, 21,22,23]. All CTAs were transferred to the core imaging reading site (Townsville, Australia), where they were analysed using the Philips MxView Visualisation Workstation using the Advance Vessel Analysis application (v7) [11, 21,22,23]. This programme was used to estimate maximum orthogonal aortic diameter using a validated protocol as previously described [8, 11, 27]. A region of interest (ROI) was selected, which included the region marked by the slice inferior to the origin of the lowest renal artery (excluding accessory arteries) to the slice superior to the aortic bifurcation. Within this ROI, the aorta was scouted by the operator to identify the region of maximal diameter by performing many measurements [8, 11, 27]. Anterior–posterior outer-to-outer orthogonal diameters were estimated by tracing the lumen of the infrarenal aorta and measuring perpendicular to this axis. The measurement was recorded to the nearest 0.1 mm [8, 11, 27]. The reproducibility of this method has been previously assessed (coefficient of variation < 4%) [27].
Biomechanical analysis
PWS and PWRI were estimated from the FEA of CTAs using commercially available software (A4 Research 5.0, VASCOPS GmbH) as previously described [9, 11, 14]. PWS estimated the maximum tensile stress to which the aortic wall was subjected based on AAA morphology and blood pressure (BP). PWRI estimated the maximum ratio between wall stress and the estimated local aortic wall strength [9, 11]. Three-dimensional (3D) reconstructions of the AAA were created from an ROI using the boundaries as defined earlier. The 3D model was processed into a hexahedral mesh to prevent volume locking of incompressible solids [11, 14]. AAA wall strength was estimated using a statistical model incorporating intra-luminal thrombus thickness, AAA diameter, and sex as previously described [11, 14, 16]. Wall strength values related to the variables included in this model were estimated from tensile testing of human AAA wall specimens, as described previously [16, 28]. The AAA FEA model was pressurised by inputting BP, which in turn estimated the mechanical stress on the aortic wall [9, 11, 14, 16]. The main analysis used patient-specific BP at recruitment to compute PWS and PWRI. A sensitivity analysis was performed using a standardized BP of 140/80 mmHg consistent with the approach of prior studies [9, 11]. Biomechanical analyses were performed by a medical doctor who received 12 months of training in FEA. The intra-observer reproducibility of PWS in asymptomatic intact AAAs has previously been reported (coefficient of variation 2.7%) [11].
Definition and assessment of outcome
The primary outcome was AAA events defined as AAA rupture or repair [29, 30]. This was recorded through prospective follow-up which included clinical reviews, medical record reviews, and linked data on inpatient admissions as previously described [21,22,23]. Decisions regarding the requirement for surgical repair were at the discretion of the treating vascular surgeon but were consistent with current international guidelines [1, 4]. Surgical repair was performed by a vascular surgeon. Participants were censored at the first outcome event, or at the date of the last review or linked data request if an outcome event did not occur.
Sample size
The sample size for the present study was based on the planned Cox regression analyses to assess the associations between PWS/ PWRI and the risk of AAA events. Based on previous studies of patients with small AAAs, the rate of AAA events was estimated to be 20% over 2 years [10, 23, 31]. The Cox proportion hazard analyses were planned to include 3 covariates (AAA diameter, statin prescription, and age). It was estimated that at least 200 individuals would lead to a well-powered analysis in order to attain at least 10 outcome events per degree of freedom according to Monte-Carlo simulations [32].
Data analysis
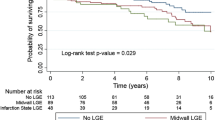
Nominal data were compared between groups using the Pearson χ2 test. Most continuous variables were not normally distributed according to Q–Q plots and Kolmogorov–Smirnov testing and therefore non-parametric Mann–Whitney U tests were used to compare groups. Kaplan–Meier curves with the log-rank test were used to compare the proportion of participants having AAA events. Cox proportional hazard analyses were undertaken to assess the association between PWS and PWRI with AAA events. To examine whether PWS and PWRI were independently associated with AAA events Cox proportional hazard analyses were adjusted for age, male sex, statin prescription, and AAA diameter. These variables were selected for adjustment as they were different (p < 0.100) between participants who had an AAA event and those who did not. Results were presented as hazard ratios (HR) and 95% confidence intervals (CI). HRs were expressed per 1 standard deviation increase in PWS or PWRI. A sub-analysis was performed which was restricted to female participants. A correlation matrix of coefficients in the Cox models was used to assess if there was co-linearity between variables included in the regression analyses [33, 34]. A correlation coefficient ≥ 0.60 was considered to indicate a high likelihood of co-linearity and was not found with any of the variables included in the final models [33,34,35]. Whether PWS and PWRI with or without clinical risk factors significantly improved stratification of risk of AAA events over using AAA diameter alone was examined using the net reclassification index (NRI) [22]. Clinical risk factors included were diabetes and current smoking as these are recognised risk factors for AAA growth [4, 36]. Classification and regression tree analysis (CART) was used to determine the optimal predictive cut-off of variables that were found to best stratify the risk of AAA events. The sample was segregated according to a decision tree consisting of progressive binary splits as previously described [37]. Every value of each predictive variable was considered as a potential split and the optimal split was based on the impurity criterion [38]. The maximum p value for a split was set at 0.050. A sensitivity analysis was performed in which a standardized BP of 140/80 mmHg was used to calculate PWS and PWRI. Data were analysed using the Stata v16.1 (StataCorp LP) software package. p values of < 0.05 were accepted to be significant for all analyses.
Results
Participant characteristics
A total of 210 participants were included and followed up for a median of 2.0 (interquartile range [IQR] 1.9, 2.8) years. During this time, 45 (21%) participants had an AAA event including 43 who had an AAA repair and 2 that had an AAA rupture. Repairs included 36 endovascular and 7 open surgical repairs. The baseline characteristics of participants in relation to whether they later had an AAA event are presented in Table 1. Participants who had an AAA event had a significantly larger initial maximum orthogonal aortic diameter (median [IQR], 44.4 [40.8, 47.0] vs 40.2 [36.5, 42.8] mm; p < 0.001) and were significantly younger at the time of recruitment than those not having an event (p = 0.038). No significant differences in sex, current smoking, diabetes, CHD, BP, and other risk factors between groups were identified (see Table 1).
Association between PWS and PWRI at entry and AAA events
PWS and PWRI at entry were significantly greater in participants who later had an AAA event compared to those that did not (p < 0.001 and p < 0.001 respectively; see Table 1). Figure 2 illustrates the proportion of participants who had an AAA event in relation to the tertiles of PWS and PWRI measured at entry. A greater proportion of participants grouped in tertile 3 of PWS and PWRI had an AAA event compared to individuals in tertile 1 (log-rank test p < 0.001 and p < 0.001 for PWS and PWRI respectively). Findings from the Cox proportional hazard analysis are reported in Table 2. In the unadjusted analysis, both higher PWS and PWRI at entry were associated with a significantly higher risk of an AAA event. In the adjusted analysis both higher PWS (HR 1.56, 95% CI 1.19, 2.06; p = 0.001) and PWRI (HR 1.74, 95% CI 1.29, 2.34; p < 0.001) were associated with a significantly increased risk of AAA events. In the sub-analysis restricted to female participants, high PWRI, but not PWS, was associated with an increased risk of AAA events (Supplementary Table 1).
Ability of PWS and PWRI to improve stratification of risk of AAA events
PWRI (NRI 0.42 95% CI 0.09, 0.75; p = 0.013), but not PWS (NRI 0.26 95% CI − 0.07, 0.59; p = 0.124), significantly improved the classification of risk of AAA events compared to AAA diameter alone. Models incorporating clinical risk factors, AAA diameter, and PWRI (but not PWS) significantly improved the classification of risk of AAA events compared to AAA diameter alone (Table 3). All baseline variables that were different between participants that did and did not have an AAA event (p < 0.100) were entered into the CART analyses. PWS and PWRI contributed to the stratification of risk of AAA events, estimated between HR 0.52 and 7.37. PWRI was identified as the best single risk stratification measure for AAA events, using a cut-off value of 0.562 (Fig. 3). Participants with PWRI ≥ 0.562 were significantly more likely to experience a AAA event than those with PWRI < 0.562 (Cox proportional HR for AAA events: 5.55; 95% CI 2.67, 11.57, p < 0.001; Fig. 4).
Classification and regression tree analysis (CART) for AAA events. Variables different (p < 0.100) between participants who had events and those who did not have events (age, statin prescription, peak wall stress [PWS], peak wall rupture index [PWRI], and AAA diameter) were entered into the analysis. The maximum p-value for a split was set at 0.050. N, numbers of individuals in subgroup; F, events; HR, hazard ratio
Sensitivity analysis in which PWS and PWRI were estimated using a standardized BP
Using PWS and PWRI estimated using a standardized blood pressure of 140/80 mmHg did not substantially change findings from the main analysis (Supplementary Tables 2 to 4).
Discussion
The main finding of this investigation was that both higher PWS and PWRI were associated with a higher risk of AAA events after adjustment for other risk factors. PWRI was identified as the best risk stratification measure of AAA events in the CART analysis. When compared to AAA diameter alone, PWRI, but not PWS significantly improved the classification of risk of AAA events. Similarly, models including clinical risk factors, AAA diameter, and PWRI also improved the classification of the risk of AAA events compared to diameter alone. The findings are commensurate with a recent meta-analysis of case–control studies that reported that PWRI, but not PWS, was greater in ruptured than asymptomatic intact AAAs of similar diameter [9]. Overall, the findings suggest that PWRI can independently predict AAA events and may add to AAA diameter in stratifying the risk for events in patients with small AAAs. PWRI could potentially assist clinicians in identifying small AAA patients who may benefit from more frequent follow-up or better medical management; however, larger studies are required to investigate this.
Maximum aortic diameter is used in clinical practice to determine when AAA repair should be recommended but has a number of limitations including substantial measurement error [1, 7]. Biomechanical measurements have been proposed for predicting AAA progression but the evidence to support them has been limited [9, 19]. PWS and PWRI are among the most widely studied biomechanical measures [9, 19, 20] although all prior investigations have been of retrospective and case–control design, had small sample sizes, and focused on large AAAs [9, 19]. The current investigation had a number of strengths in comparison to these prior studies such as the inclusion of prospectively collected data and the study of individuals with small AAAs. While the main analysis used patient-specific blood pressure to compute PWS and PWRI, a sensitivity analysis using standardised blood pressure was also performed. It remains unclear which method is most appropriate [9]; nevertheless, the findings were similar in both analyses. Furthermore, a sub-analysis restricted to female participants demonstrated a similar finding to the main analysis.
Although PWS and PWRI can be performed using semi-automated methods [11, 15], FEA is time and resource intensive (~40 min per CTA scan [13, 18]) in comparison to other simpler measures of rupture risk such as AAA diameter [9, 14]. It is therefore important that biomechanical measures have a demonstrated benefit in predicting events to support their use in clinical practice. The current study suggested that PWRI was independently predictive of AAA events and may improve the classification of the risk of events compared to using AAA diameter alone. Further larger observational studies with longer follow-ups are required to confirm or refute the findings of this study.
This investigation has a number of limitations including its small sample size and relatively short follow-up time which was comparable to a recent observational study [10]. The decision to perform surgical repair was at the discretion of the treating vascular surgeon and a standardised protocol was not followed for this study [4]. AAA diameter prior to repair could not be reliably obtained from medical records given the substantial variability in AAA diameter measurement methods and reporting used in routine clinical practise [7]. Importantly there are a number of limitations of FEA, which need to be addressed [9, 19, 20]. Firstly, there remains no standardised approach by which FEA is performed and significant heterogeneity in methods has been reported in prior reviews [9, 19]. Furthermore, there is currently no accurate method by which wall thickness and strength can be estimated from CTA [9, 28]. In the current study, aortic wall strength was estimated from previously reported tensile testing of human wall specimens [11, 14, 16] and a standardised wall thickness was assumed for PWRI estimates. Recent studies suggest that wall thickness can be estimated from MRI [10, 13]; however, this may not be feasible in routine clinical practice. Some factors which may influence aortic biomechanical forces were not investigated in this study such as intra-luminal thrombus and aneurysm flow volume [39, 40]. Lastly, participants were recruited from a limited number of vascular centres, and further investigation is needed to examine whether the findings are repeatable in other populations.
In conclusion, this study suggested that PWS and PWRI can independently predict the risk of AAA events in individuals with small aneurysms. PWRI, but not PWS, significantly improved the stratifying of risk of events compared to aortic diameter alone.
Abbreviations
- 3D:
-
Three-dimensional
- AAA:
-
Abdominal aortic aneurysm
- BP:
-
Blood pressure
- CART:
-
Classification and regression tree analysis
- CHD:
-
Coronary heart disease
- CI:
-
Confidence intervals
- COPD:
-
Chronic obstructive pulmonary disease
- CTA:
-
Computed tomography angiography
- FEA:
-
Finite element analysis
- HR:
-
Hazard ratio
- MRI:
-
Magnetic resonance imaging
- NRI:
-
Net reclassification index
- PWRI:
-
Peak wall rupture index
- PWS:
-
Peak wall stress
- ROI:
-
Region of interest
References
Golledge J (2019) Abdominal aortic aneurysm: update on pathogenesis and medical treatments. Nat Rev Cardiol 16:225–242
Abubakar I, Tillmann T, Banerjee A (2015) Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385:117–171
Sampson UK, Norman PE, Fowkes FGR et al (2014) Global and regional burden of aortic dissection and aneurysms: mortality trends in 21 world regions, 1990 to 2010. Glob Heart 9(171–180):e110
Wanhainen A, Verzini F, Van Herzeele I et al (2020) European Society for Vascular Surgery (ESVS) 2019 Clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms (vol 57, pg 8, 2019). Eur J Vasc Endovasc Surg 59:494–494
Cao P, De Rango P, Verzini F et al (2011) Comparison of surveillance versus aortic endografting for small aneurysm repair (CAESAR): results from a randomised trial. Eur J Vasc Endovasc Surg 41:13–25
Participants TUSAT (1998) Mortality results for randomised controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. Lancet 352:1649–1655
Golledge J, Norman PE, Murphy MP, Dalman RL (2017) Challenges and opportunities in limiting abdominal aortic aneurysm growth. J Vasc Surg 65:225–233
Golledge J, Wolanski P, Parr A, Buttner P (2008) Measurement and determinants of infrarenal aortic thrombus volume. Eur Radiol 18:1987–1994
Singh TP, Moxon JV, Gasser TC, Golledge J (2021) Systematic review and meta-analysis of peak wall stress and peak wall rupture index in ruptured and asymptomatic intact abdominal aortic aneurysms. J Am Heart Assoc 10:e019772
Doyle BJ, Bappoo N, Syed MB et al (2020) Biomechanical assessment predicts aneurysm related events in patients with abdominal aortic aneurysm. Eur J Vasc Endovasc Surg 60:365–373
Singh T, Moxon J, Iyer V, Gasser TC, Jenkins J, Golledge J (2021) Comparison of peak wall stress and peak wall rupture index in ruptured and asymptomatic intact abdominal aortic aneurysms. Br J Surg 108:652–658
Siika A, Lindquist Liljeqvist M, Hultgren R, Gasser TC, Roy J (2018) Aortic lumen area is increased in ruptured abdominal aortic aneurysms and correlates to biomechanical rupture risk. J Endovasc Ther 25:750–756
Joldes GR, Miller K, Wittek A, Forsythe RO, Newby DE, Doyle BJ (2017) BioPARR: a software system for estimating the rupture potential index for abdominal aortic aneurysms. Sci Rep 7:1–15
Gasser TC, Nchimi A, Swedenborg J et al (2014) A novel strategy to translate the biomechanical rupture risk of abdominal aortic aneurysms to their equivalent diameter risk: method and retrospective validation. Eur J Vasc Endovasc Surg 47:288–295
Gasser TC (2016) Biomechanical rupture risk assessment. Aorta 4:42–60
Geest JPV, Wang DH, Wisniewski SR, Makaroun MS, Vorp DA (2006) Towards a noninvasive method for determination of patient-specific wall strength distribution in abdominal aortic aneurysms. Ann Biomed Eng 34:1098–1106
Teutelink A, Cancrinus E, van de Heuvel D, Moll F, de Vries J-P (2012) Preliminary intraobserver and interobserver variability in wall stress and rupture risk assessment of abdominal aortic aneurysms using a semiautomatic finite element model. J Vasc Surg 55:326–330
Hyhlik-Dürr A, Krieger T, Geisbüsch P, Kotelis D, Able T, Böckler D (2011) Reproducibility of deriving parameters of AAA rupture risk from patient-specific 3D finite element models. J Endovasc Ther 18:289–298
Khosla S, Morris D, Moxon J, Walker PJ, Gasser T, Golledge J (2014) Meta-analysis of peak wall stress in ruptured, symptomatic and intact abdominal aortic aneurysms. Br J Surg 101:1350–1357
Groeneveld ME, Meekel JP, Rubinstein SM et al (2018) Systematic review of circulating, biomechanical, and genetic markers for the prediction of abdominal aortic aneurysm growth and rupture. J Am Heart Assoc 7:e007791
Golledge J, Cronin O, Iyer V, Bradshaw B, Moxon JV, Cunningham MA (2013) Body mass index is inversely associated with mortality in patients with peripheral vascular disease. Atherosclerosis 229:549–555
Golledge J, Ewels C, Muller R, Walker PJ (2014) Association of chronic kidney disease categories defined with different formulae with major adverse events in patients with peripheral vascular disease. Atherosclerosis 232:289–297
Golledge J, Pinchbeck J, Tomee SM et al (2020) Efficacy of telmisartan to slow growth of small abdominal aortic aneurysms: a randomized clinical trial. JAMA Cardiol 5:1374–1381
Ankle Brachial Index Collaboration (2008) Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA 300:197
Singh T, Morris D, Smith S, Moxon J, Golledge J (2017) Systematic review and meta-analysis of the association between C-reactive protein and major cardiovascular events in patients with peripheral artery disease. Eur J Vasc Endovasc Surg 54:220–233
Thomas Manapurathe D, Moxon JV, Krishna SM et al (2019) Cohort study examining the association between blood pressure and cardiovascular events in patients with peripheral artery disease. J Am Heart Assoc 8:e010748
Parr A, Jayaratne C, Buttner P, Golledge J (2011) Comparison of volume and diameter measurement in assessing small abdominal aortic aneurysm expansion examined using computed tomographic angiography. Eur J Radiol 79:42–47
Raghavan ML, Webster MW, Vorp DA (1996) Ex vivo biomechanical behavior of abdominal aortic aneurysm: assessment using a new mathematical model. Ann Biomed Eng 24:573–582
Golledge J, Moxon J, Singh T, Bown M, Mani K, Wanhainen A (2020) Lack of an effective drug therapy for abdominal aortic aneurysm. J Intern Med 288:6–22
Abola MTB, Golledge J, Miyata T et al (2020) Asia-Pacific consensus statement on the management of peripheral artery disease: a report from the Asian Pacific Society of Atherosclerosis and Vascular Disease Asia-Pacific Peripheral Artery Disease Consensus Statement Project Committee. J Atheroscler Thromb 27:809–907
Golledge J, Singh TP (2021) Effect of blood pressure lowering drugs and antibiotics on abdominal aortic aneurysm growth: a systematic review and meta-analysis. Heart 107:1465–1471
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49:1373–1379
Farrar DE, Glauber RR (1967) Multicollinearity in regression analysis: the problem revisited. Rev Econ Stat 92–107
Mansfield ER, Helms BP (1982) Detecting multicollinearity. Am Stat 36:158–160
Grewal R, Cote JA, Baumgartner H (2004) Multicollinearity and measurement error in structural equation models: implications for theory testing. Mark Sci 23:519–529
Sweeting M, Thompson S, Brown L, Powell J (2012) Meta-analysis of individual patient data to examine factors affecting growth and rupture of small abdominal aortic aneurysms. Br J Surg 99:655–665
Morris D, Singh T, Moxon J et al (2017) Assessment and validation of a novel angiographic scoring system for peripheral artery disease. Br J Surg 104:544–554
Marshall RJ (2001) The use of classification and regression trees in clinical epidemiology. J Clin Epidemiol 54:603–609
Singh TP, Wong SA, Moxon JV, Gasser TC, Golledge J (2019) Systematic review and meta-analysis of the association between intraluminal thrombus volume and abdominal aortic aneurysm rupture. J Vasc Surg 70(2065–2073):e2010
Niklas N, Gutowski P, Kazimierczak A, Rynio P (2022) Abdominal aortic aneurysm morphology as an essential criterion for stratifying the risk of aneurysm rupture. J Clin Med 11:933
Acknowledgements
We thank all investigators involved in the TEDY trial. A full list of principal investigators and trial coordinators has been included in the Supplement.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This research was supported by grants from the National Health and Medical Research Council (1180736; 1022752), BUPA, The Heart Foundation, and Queensland Government. The Stanford arm of the TEDY trial was sponsored by Medtronic Inc., Santa Rosa, CA. JG holds a Practitioner Fellowship from the NHMRC (1117601) and a Senior Clinical Research Fellowship from the Queensland Government. JVM holds an Advance Queensland Mid-Career fellowship from the Queensland Government. TPS holds a Junior Doctor Research Fellowship from the Queensland Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jonathan Golledge.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• observational
• multicenter study
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singh, T.P., Moxon, J.V., Gasser, T.C. et al. Association between aortic peak wall stress and rupture index with abdominal aortic aneurysm–related events. Eur Radiol 33, 5698–5706 (2023). https://doi.org/10.1007/s00330-023-09488-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09488-1