Abstract
Objectives
This study aimed to identify whether apparent diffusion coefficient (ADC) values and dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) parameters are helpful in distinguishing mesorectal tumor deposits (TD) from metastatic lymph nodes (MLN) in rectal cancer (RC).
Methods
Thirty patients (59 lesions, including 30 TD and 29 MLN) with RC who underwent pretreatment-MRI between February 2016 and August 2018 were enrolled. The morphological features, ADC values, and semi-quantitative parameters of DCE-MRI, including relative enhancement (RE), maximum enhancement (ME), maximum relative enhancement (MRE), time to peak (TTP), wash-in rates (WIR), wash-out rates (WOR), brevity of enhancement (BRE), and area under the curve (AUC) were measured on lesions (TD or MLN) and RC. The parameters were compared between TD and MLN, tumor with and without TD group by using Fisher’s exact test, independent-samples t-test, and Mann-Whitney U test. The ratio (lesion-to-tumor) of the parameters was compared between TD and MLN. Receiver operating characteristic curve analysis and binary logistic regression analysis were used to assess the diagnostic ability of single and combined metrics for distinguishing TD from MLN.
Results
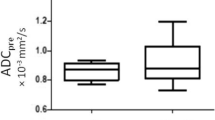
The morphological features, including size, shape, and border, were significantly different between TD and MLN. TD exhibited significantly lower RE, MRE, RE-ratio, MRE-ratio, ADCmin-ratio, and ADCmean-ratio than MLN. RE-ratio showed the highest AUC (0.749) and accuracy (77.97%) among single parameters. The combination of DCE-MRI and DWI parameters together showed higher diagnostic efficiency (AUC = 0.825).
Conclusions
Morphological features, ADC values, and DCE-MRI parameters can preoperatively help distinguish TD from MLN in RC.
Key Points
• DWI and DCE-MRI can facilitate early detection and distinguishing mesorectal TD (tumor deposits) from MLN (metastatic lymph nodes) in rectal cancer preoperatively.
• TD has some specific morphological features, including relatively larger size, lower short- to long-axis ratio, irregular shape, and ill-defined border on T2-weighted MR images in rectal cancer.
• The combination of ADC values and semi-quantitative parameters of DCE-MRI (RE, MRE) can help to improve the diagnostic efficiency of TD in rectal cancer.



Similar content being viewed by others
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- BRE:
-
Brevity of enhancement
- EMVI:
-
Extramural vascular invasion
- FOV:
-
Field of view
- ICC:
-
Intraclass correlation coefficient
- LN:
-
Lymph node
- ME:
-
Maximum enhancement
- MLN:
-
Metastatic lymph nodes
- MRE:
-
Maximum relative enhancement
- NAT:
-
Neoadjuvant therapy
- RC:
-
Rectal cancer
- RE:
-
Relative enhancement
- T2WI:
-
T2-weighted imaging
- TD:
-
Tumor deposits
- TE:
-
Echo time
- TIC:
-
Time-signal intensity curve
- TNM:
-
Tumor-node-metastasis
- TR:
-
Repetition time
- TSE:
-
Turbo spin echo
- TTP:
-
Time to peak
- WIR:
-
Wash-in rates
- WOR:
-
Wash-out rates
References
Moon JY, Lee MR, Ha GW (2022) Prognostic value of tumor deposits for long-term oncologic outcomes in patients with stage III colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis 37:141–151
Zheng H, Zhang J, Liu Y, Wang X (2021) Prognostic value of tumor deposits in locally advanced rectal cancer: a retrospective study with propensity score matching. Int J Clin Oncol 26:1109–1119
Lord AC, Graham Martinez C, D'Souza N, Pucher PH, Brown G, Nagtegaal ID (2019) The significance of tumour deposits in rectal cancer after neoadjuvant therapy: a systematic review and meta-analysis. Eur J Cancer 122:1–8
Nagtegaal ID, Knijn N, Hugen N et al (2017) Tumor deposits in colorectal cancer: improving the value of modern staging-a systematic review and meta-analysis. J Clin Oncol 35:1119–1127
Lord AC, D’Souza N, Pucher PH et al (2017) Significance of extranodal tumour deposits in colorectal cancer: a systematic review and meta-analysis. Eur J Cancer 82:92–102
Weiser MR (2018) AJCC 8th Edition: Colorectal Cancer. Ann Surg Oncol 25:1454–1455
Lord AC, D’Souza N, Shaw A et al (2022) MRI-diagnosed tumour deposits and EMVI status have superior prognostic accuracy to current clinical TNM staging in rectal cancer. Ann Surg 276:334–344
Schaap DP, Voogt ELK, Burger JWA et al (2021) Prognostic implications of MRI-detected EMVI and tumor deposits and their response to neoadjuvant therapy in cT3 and cT4 rectal cancer. Int J Radiat Oncol Biol Phys 111:816–825
Chandramohan A, Mittal R, Dsouza R et al (2022) Prognostic significance of MR identified EMVI, tumour deposits, mesorectal nodes and pelvic side wall disease in locally advanced rectal cancer. Colorectal Dis 24:428–438
Bouquot M, Creavin B, Goasguen N et al (2018) Prognostic value and characteristics of N1c colorectal cancer. Colorectal Dis 20:O248–O255
Zheng K, Zheng N, Xin C et al (2020) The prognostic significance of tumor deposit count for colorectal cancer patients after radical surgery. Gastroenterol Res Pract 2020:2052561
Bai R, Tan Y, Li D et al (2021) Development and validation of a novel prognostic nomogram including tumor deposits could better predict survival for colorectal cancer: a population-based study. Ann Transl Med 9:620
Kitamura K, Shida D, Sekine S et al (2021) Comparison of model fit and discriminatory ability of the 8th edition of the tumor-node-metastasis classification and the 9th edition of the Japanese classification to identify stage III colorectal cancer. Int J Clin Oncol 26:1671–1678
Pei JP, Zhang CD, Liang Y et al (2020) A modified pathological N stage including status of tumor deposits in colorectal cancer with nodal metastasis. Front Oncol 10:548692
Bates DDB, Homsi ME, Chang KJ, Lalwani N, Horvat N, Sheedy SP (2022) MRI for rectal cancer: staging, mrCRM, EMVI, lymph node staging and post-treatment response. Clin Colorectal Cancer 21:10–18
Horvat N, Carlos Tavares Rocha C, Clemente Oliveira B, Petkovska I, Gollub MJ (2019) MRI of rectal cancer: tumor staging, imaging techniques, and management. Radiographics 39:367–387
Atre ID, Eurboonyanun K, Noda Y et al (2021) Utility of texture analysis on T2-weighted MR for differentiating tumor deposits from mesorectal nodes in rectal cancer patients, in a retrospective cohort. Abdom Radiol (NY) 46:459–468
Wacquet J, Pote N, Cazals-Hatem D, Maggiori L, Panis Y, Guedj N (2021) Smooth muscular layer: a new helpful criterion to reclassify tumor deposits into metastatic lymph nodes in patients with colo-rectal adenocarcinoma. Ann Diagn Pathol 54:151771
Gabriel WB, Dukes C, Bussey HJR (1935) Lymphatic spread in cancer of the rectum. Br J Surgery 23:395–413
Wunsch K, Muller J, Jahnig H, Herrmann RA, Arnholdt HM, Markl B (2010) Shape is not associated with the origin of pericolonic tumor deposits. Am J Clin Pathol 133:388–394
Lord AC, Moran B, Abulafi M et al (2020) Can extranodal tumour deposits be diagnosed on MRI? Protocol for a multicentre clinical trial (the COMET trial). BMJ Open 10:e033395
Moreau B, Iannessi A, Hoog C, Beaumont H (2018) How reliable are ADC measurements? A phantom and clinical study of cervical lymph nodes. Eur Radiol 28:3362–3371
Dijkhoff RAP, Beets-Tan RGH, Lambregts DMJ, Beets GL, Maas M (2017) Value of DCE-MRI for staging and response evaluation in rectal cancer: a systematic review. Eur J Radiol 95:155–168
Liu HL, Zong M, Wei H et al (2018) Differentiation between malignant and benign breast masses: combination of semi-quantitative analysis on DCE-MRI and histogram analysis of ADC maps. Clin Radiol 73:460–466
Mazaheri Y, Akin O, Hricak H (2017) Dynamic contrast-enhanced magnetic resonance imaging of prostate cancer: a review of current methods and applications. World J Radiol 9:416–425
Dijkhoff RAP, Maas M, Martens MH et al (2017) Correlation between quantitative and semiquantitative parameters in DCE-MRI with a blood pool agent in rectal cancer: can semiquantitative parameters be used as a surrogate for quantitative parameters? Abdom Radiol (NY) 42:1342–1349
Liu L, Hu L, Zeng Q et al (2021) Dynamic contrast-enhanced MRI of nasopharyngeal carcinoma: correlation of quantitative dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) parameters with hypoxia-inducible factor 1alpha expression and tumor grade/stage. Ann Palliat Med 10:2238–2253
Nagtegaal ID, Quirke P (2007) Colorectal tumour deposits in the mesorectum and pericolon; a critical review. Histopathology 51:141–149
Kargol J, Rudnicki W, Kenig J et al (2021) Diffusion-weighted magnetic resonance imaging of 103 patients with rectal adenocarcinoma identifies the apparent diffusion coefficient as an imaging marker for tumor invasion and regional lymph node involvement. Med Sci Monit 27:e934941
Colakoglu Er H, Erden A (2017) Mean ADC values discriminate rectal mucinous carcinomafrom rectal nonmucinous adenocarcinoma. Turk J Med Sci 47:1520–1525
Oberholzer K, Menig M, Pohlmann A et al (2013) Rectal cancer: assessment of response to neoadjuvant chemoradiation by dynamic contrast-enhanced MRI. J Magn Reson Imaging 38:119–126
Funding
This work has received funding from Beijing Municipal Natural Science Foundation (No.7222316) and the Fundamental Research Funds for the Central Universities (No. 3332020077).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Hongliang Sun.
Conflict of interest
Authors declare that they have no conflict of interest.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 328 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, Q., Xu, Y., Wang, J. et al. Distinguishing mesorectal tumor deposits from metastatic lymph nodes by using diffusion-weighted and dynamic contrast-enhanced magnetic resonance imaging in rectal cancer. Eur Radiol 33, 4127–4137 (2023). https://doi.org/10.1007/s00330-022-09328-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09328-8