Abstract
Purpose
To analyze relationships betweenapparent diffusion coefficient (ADC) and activity parameters of Crohn’s disease, e.g., length and wall thickness, CRP, FCP, MaRIA, CDAI, SES-CD, histologic inflammatory activity score, and the histological fibrotic score, based upon published data.
Materials and methods
MEDLINE library, Scopus, and Embase databases were screened for association between ADC and activity parameters of Crohn’s disease in patients with Crohn’s disease up to Mai 2021. Overall, 21 studies with 1053 patients were identified. The following data were extracted from the literature: number of patients, correlation coefficients between ADC and length as well as wall thickness, CRP, FCP, MaRIA, CDAI, and SES-CD, inflammatory activity score, and fibrotic score. Associations between ADC and activity parameters were analyzed by Spearman’s correlation coefficient. The studies’ methodologic quality was evaluated by using the Quality Assessment of Diagnostic Studies (QUADAS 2) instrument, revealing a low risk of bias.
Results
In the overall sample, the pooled correlation coefficient between ADC and CDAI was −0.8 (95% CI = [−0.94; −0.65]), between ADC and MaRIA −0.66 (95% CI = [−0.79; −0.53]). A strong association was observed between ADC and SES-CD with a pooled correlation of −0.66 (95% CI = [−0.87; −0.46]). The pooled sensitivity to discriminate between involved and non-involved bowel segments was 0.89, with an area under the curve of 0.89
Conclusions
ADC showed strong inverse correlations with CDAI, MaRIA, and SES-CD scores. However, the role of ADC in assessing fibrotic changes in the bowel wall is limited. ADC can reflect acute inflammatory reactions but not systemic inflammation.
Key Points
• ADC value can reflect acute inflammatory reactions but not systemic inflammation.
• ADC is inversely correlated with CDAI, MaRIA, and SES-CD.
• The role of ADC in assessing fibrotic changes in the bowel wall is limited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) is one of the common chronic disorders in the industrialized world with an incidence of 3–20 cases per 100,000 and a wide spectrum of clinical manifestations [1,2,3]. Due to the varying pattern of CD, disease activity must be closely monitored. Severity of disease can be determined with quantitative or semiquantitative assessment of inflammation in the bowel [4].
Aside from laboratory, endoscopic, and enterographic examinations, magnetic resonance enterography (MRE) is the most important imaging modality for monitoring disease activity. It allows non-invasive investigation of the gastrointestinal tract and provides an assessment of inflammatory activity and potential complications in all bowel segments [5,6,7,8,9]. Current MR protocols include rapid MR sequences for data acquisition during a single breath-hold with minimal motion artefacts and rapid morphological sequences with a gadolinium-chelate-enhanced series [10]. However, with rising concerns about gadolinium retention in different organs, particularly the brain, the repeated application of gadolinium-based contrast agents is viewed critically [11, 12]. Therefore, alternative non-enhanced methods for repeated lifelong disease monitoring have gained relevance. MRI protocols usually include diffusion-weighted sequences (DWI-MRE), allowing for qualitative and quantitative assessment of random motion of water molecules in biological tissues. The use of DWI is recommended as an optional sequence for Crohn’s disease by the European Society of Gastrointestinal and Abdominal Radiology in the latest consensus statements [13]. DWI could therefore potentially replace the contrast-enhanced sequences with comparable diagnostic power [6].
Choi et al [14] showed in a meta-analysis that accuracy and diagnostic strength of DWI-MRE in assessing bowel inflammation were overestimated in some studies. The correlation of DWI-derived apparent diffusion coefficient (ADC) with disease activity produced heterogeneous results and clinical relevance of quantitative ADC measurements could not be established due to the limited number of studies available at the time. With a growing interest in DWI-MRE and ADC in CD patients in recent years, this paucity has been largely cleared. A recent meta-analysis involving nine studies with pediatric patients with inflammatory bowel disease reported a sensitivity and specificity of DWI-MRE of 0.93 and 0.95, respectively [15]. In the meta-analysis by Choi et al [14], the data was based mostly on studies explaining the diagnostic value of DWI images and not the quantitative ADC value. Moreover, the published data has been increasingly growing since then, necessitating an updated analysis. To our knowledge, no systematic evaluation of the associations of ADC values with inflammation and fibrosis scores in CD has been performed in an adult population [16,17,18,19,20,21,22,23,24,25,26,27,28,29].
The aim of the present meta-analysis was to analyze the role of ADC in assessing disease activity in patients with CD.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA) was used for the literature search [30].
Literature search
MEDLINE library, Scopus, and Embase online databases were checked to identify studies for associations between ADC and different activity parameters of Crohn’s disease up to Mai 2021 using the following search criteria: “(Crohn) OR (inflammatory bowel disease) OR (IBD) AND (DWI) OR (diffusion weighted imaging) OR (ADC) OR (apparent diffusion coefficient).” Only papers written in English were included.
Inclusion criteria
The first primary endpoint of the meta-analysis was the reported correlation between quantitative ADC measurements and activity parameters of Crohn’s disease. The second primary endpoint was the reported diagnostic abilities of ADC values for discrimination purposes of acute inflammation and fibrosis.
Studies (or subsets of studies) were included if they satisfied the following criteria:
-
1.
Patients with Crohn’s disease (based on standard clinical, endoscopic, imaging, and histologic criteria);
-
2.
Patients, who underwent MR enterography with DWI sequence quantified by ADC values;
-
3.
Correlation coefficient between ADC and activity parameters of Crohn’s disease;
-
4.
Receiver operating characteristic analysis with reported sensitivity, specificity, and area under the curve (AUC) for the discrimination analysis between involved and non-involved bowel segments.
Exclusion criteria
Exclusion criteria were as follows:
-
1.
Systematic review;
-
2.
Case reports;
-
3.
Conference abstracts, letter, editorials, meta-analysis, guidelines;
-
4.
Non-English language;
-
5.
Studies that analyzed patients with colitis ulcerosa or colitis ulcerosa and Crohn’s disease together.
Two readers (A.S. with 18 years of experience in radiology and B.M. with 9 years of experience in radiology) independently evaluated all articles and studies. In cases of disagreement, a third observer (H.J.M. with 6 years of experience) was consulted to reach a decision in consensus.
Data extraction and quality assessment
Information was extracted on study characteristics (authors, year of publication, study design), demographic and clinical characteristics (sample size, male to female ratio, patient age), activity parameters, and correlation coefficients between ADC and activity of Crohn’s disease. The activity parameters included wall thickness and length, fecal calprotectin (FCP) and C-reactive protein (CRP), a magnetic resonance index of activity (MaRIA) and Crohn’s disease activity index (CDAI), endoscopic activity score (SES-CD), histologic inflammatory activity score, and also the histological fibrosis score.
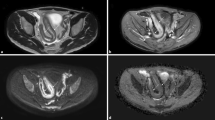
In accordance with a wide spectrum of different activity parameters of Crohn’s disease, we divided all data into subgroups for assessing the correlation with ADC: (1) studies with an investigated correlation between ADC and morphological changes such as length and wall thickness; (2) ADC and laboratory parameters such as FCP and CRP; (3) ADC and activity indices: MaRIA and CDAI; and (4) ADC and SES-CD, histologic inflammatory activity score, and the histological fibrosis score (Fig. 1).
For the present meta-analysis, our search criteria identified 1514 articles. Duplicate records, review articles, case reports, meta-analyses, non-English publications, and articles which were not within the field of interest were excluded (n = 1464) (Fig. 2). As a next step, full-text reviews of the remaining papers (n = 50) were performed. Thereafter, 26 articles were excluded, because they were not in the field of interest and did not contain an analysis of the correlation between ADC and Crohn’s disease activity. Therefore, a total of 21 studies were involved in the analysis (Fig. 1) [16, 18,19,20,21,22,23,24,25,26,27,28,29, 31,32,33,34,35,36,37,38].
The methodologic quality of the studies was evaluated by using the Quality Assessment of Diagnostic Studies (QUADAS 2) instrument [39]. The following parameters were assessed for low, moderate, or high risk of bias: flow and timing, reference standard, index test, and patient selection.
Data synthesis and analysis
The correlations between ADC and activity parameters of Crohn’s disease were calculated by Spearman’s correlation coefficient. The reported Pearson’s correlation coefficient was recalculated into Spearman’s correlation coefficients according to the previous description [40].
The statistical analysis of the meta-analysis was calculated in program RevMan 5.3 (computer program, version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). The heterogeneity was determined by using the inconsistency index I2 [41, 42] and defined as not important with a value of index between 0 and 40%; moderate—between 30 and 60%; substantial heterogeneity—50–90%; and finally considerable—more than 75% [43]. DerSimonian and Laird’s [44] random-effects models with inverse-variance weights were estimated without any further correction.
Results
The 21 included studies comprised 1053 patients, of which 496 patients (47%) were female and 577 male (53%). There were 11 (52%) prospective and 10 (48%) retrospective studies. The size of the study population ranged from 20 to 229 patients with an average age of 26.5 years. Three studies reported results on pediatric patients [16, 37, 38], whereas the other studies only investigated adult study populations. Detailed characteristics of all studies are shown in Table 1.
The QUADAS-2 assessment revealed an overall low to moderate risk of bias in the included studies. The reference standard for inflammation differed between studies as some studies used histopathological assessment and some only clinical severity, which can result in bias. The patient selection can be considered relatively free from bias, as only three studies included pediatric patients with inherent differences from the adult population. Across studies, ADC values were measured as ADCmean values within a region of interest (ROI) of the inflamed bowel segment.
Correlations between ADC and MR morphological changes
In 2 studies including 74 patients, data about relationships between ADC and extent of bowel affection were reported. The pooled correlation coefficient between these parameters was −0.06 (95% CI = [−0.39, 0.28]), p = 0.74, heterogeneity τ2 = 0.06 (p = 0.04), I2 = 69%, test for overall effect Z = 0.33 (Fig. 3a). Associations between wall thickness and ADC were analyzed in 5 studies comprising 233 patients. The pooled correlation coefficient was −0.43 (95% CI = [−0.65; −0.22]), p < 0.00001, heterogeneity τ2 = 0.04 (p = 0.002), I2 = 76%, test for overall effect Z = 3.92 (Fig. 3b).
Correlation between ADC and disease activity scores
In 6 studies with 465 patients, a strong association between ADC and MaRIA was shown with a pooled correlation coefficient of −0.66 (95% CI = [−0.79; −0.53]), p < 0.000001, heterogeneity τ2 = 0.02 (p < 0.0001), I2 = 83%, test for overall effect Z = 10.15 (Fig. 4a).
Correlations between ADC and CDAI were reported in 2 studies (95 patients). The pooled correlation coefficient was −0.8 (95% CI = [−0.94; −0.65]), p < 0.000001, heterogeneity τ2 = 0.01 (p = 0.06), I2 = 71%, test for overall effect Z = 10.73 (Fig. 4b).
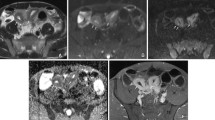
In addition, correlations between ADC and morphological parameters, like SES-CD, histological fibrotic score, and histologic inflammatory score, were evaluated (Fig. 5a–c).
In 4 studies with 193 patients, associations between ADC and SES-CD were analyzed. The pooled correlation coefficient was −0.66 (95% CI = [−0.87; −0.46]), p < 0.000001, heterogeneity τ2 = 0.04 (p < 0.0001), I2 = 88%, test for overall effect Z = 6.40 (Fig. 5a).
Correlations between ADC and histological fibrotic score were reported in 6 studies (166 patients). The pooled correlation coefficient was 0.49 CI (95% CI = [−0.61; −0.37]), p < 0.000001, heterogeneity τ2 = 0.00 (p = 0.47), I2 = 0%, test for overall effect Z = 7.96 (Fig. 5b).
In 3 studies (91 patients), relationships between ADC and histologic inflammatory score were investigated. The pooled correlation coefficient was −0.51 (95% CI = [−0.84, −0.18]), p = 0.003, heterogeneity τ2 = 0.07 (p = 0.0004), I2 = 82%, test for overall effect Z = 3.00 (Fig. 5c).
Correlation between ADC and blood inflammatory markers
Associations between ADC and CRP were shown in 5 studies with a total number of 216 patients and represented a weak pooled correlation—0.35 (95% CI = [−0.60, −0.09]), p = 0.008, heterogeneity τ2 = 0.07 (p = 0.0004), I2 = 81%, test for overall effect Z = 2.64 (Fig. 6a).
Association between ADC and FCP was reported in 3 studies (139 patients). The pooled correlation coefficient was 0.59 (95% CI = [−0.72, −0.47]), p < 0.00001, heterogeneity τ2 = 0.00 (p = 0.28), I2 = 21%, test for overall effect Z = 9.21 (Fig. 6b).
Diagnostic accuracy of ADC values
The diagnostic value of ADC values was reported in 15 studies. The overall pooled sensitivity to discriminate between involved and non-involved bowel segments was 0.89, the specificity was 0.81, and the AUC was 0.89
For studies only investigating the discriminatory power between no/mild fibrosis to moderate/strong fibrosis, the AUC was 0.84, whereas for studies investigating only acute inflammation, the AUC was 0.91.
Discussion
The present meta-analysis showed inverse associations between ADC values and disease activity scores in patients with Crohn’s disease. No strong correlation was found for the extent of bowel affection. MRE is performed routinely for most patients with CD due to its excellent diagnostic accuracy. In recent years DWI has become increasingly important in the assessment of bowel inflammation and may complement or potentially replace contrast-enhanced sequences [10]. Our results show that ADC measurements can be applied for disease monitoring in CD. To the best of our knowledge, this is the first comprehensive meta-analysis assessing the correlation of ADC with disease activity parameters in CD. ADC values could therefore potentially be employed as an imaging biomarker to guide treatment decisions. However, there is a clear need for proven threshold values and DWI method standardization.
A strong inverse correlation (ρ = −0.80) was observed in the correlation between ADC and CDAI. This finding may be significant in clinical practice. CDAI is used as a gold standard for the clinical evaluation of patients with CD. However, its reproducibility may be limited due to significant inter-observer error, even when performed by experienced physicians [45]. The strong association between ADC and CDAI could be a complement or even an alternative to symptom-guided evaluation. Our results can be considered robust as the total number of patients in the analyzed studies (n = 95) was large and reported results were standardized by age groups.
We also found a significant association between ADC and MaRIA score (ρ = −0.66). Strong associations were identified in all papers except for one work by Hectors et al [29], in which the long acquisition time of 9 min can be considered unfeasible. The prospective study by Straksyte et al [18], with a large number of patients (n = 229), showed a strong inverse correlation between ADC and MaRIA and Clermont indices. Considering the results of the cumulative correlation index as well as the prospective data, ADC measurements may have a strong potential for clinical practice and may be more easily reproduced than the MaRIA score.
We identified a strong correlation between ADC values and SES-CD (ρ = −0.66). This indicates the potential of ADC in assessing bowel inflammation. Our results are in line with the study by Buisson et al [33], showing a correlation between ADC and the depth and size of inflammatory ulcerations. The evaluation of inflammatory and fibrotic changes plays a crucial role in CD treatment [21]. Bowel fibrosis is one of the main causes of hospitalization and surgical resection in CD patients [26]. In the last years, a number of studies have been published investigating possible ways to assess and differentiate inflammatory changes from fibrotic histological alterations in bowel walls in patients with CD [20, 21, 24, 26, 28, 32]. Li et al [24] have reported that fibrotic and non-fibrotic bowel wall alterations could be differentiated by means of ADC. Also, mild inflammatory changes could be distinguished from severe ones. However, the ability of ADC to evaluate bowel fibrosis seems to decrease with increasing degrees of bowel inflammation [26].
Previously published studies reported a weak correlation between ADC values and length and thickness of bowel wall inflammation [16, 29]. Our analysis confirmed these results. Shortcomings of the available data, however, must be considered. First, only children were investigated in the included studies. Inflammatory bowel wall changes in children are not associated with fibrosis or fat accumulation, unlike in the adult population. In addition, no standardized measurement of the bowel length and thickness exists, particularly when bowel loops have a complex geometrical form or when bowel peristaltic is not sufficiently suppressed. Standardization of all images of different patients with many causes of wall thickening, like edema, fibrosis, or fat accumulation, or with different bowel distention or peristaltic suppression is challenging [46, 47]. Therefore, the correlation between these parameters and ADC may not be considered reproducible and reliable.
Regarding laboratory data, our findings also support previously published studies, in which Caruso et al [20], Dillman et al [16], and Zhu et al [31] each reported a weak inverse correlation between ADC and CRP. It remains unclear which inflammatory tissue alterations have the strongest impact on diffusion restriction. Zhu et al [31] hypothesized increased cell density in the bowel wall due to influx of lymphocytes, cell swelling, and increased viscosity due to granulomas and micro-abscess. All these processes also lead to a rise in CRP levels. The weak correlation indicates that ADC reduction allows the assessment of local inflammatory changes in the bowel but not of the systematic response, which is reflected by CRP. Thus, both parameters likely reflect distinctive aspects of disease activity.
Our results showed an inverse correlation between ADC and FCP (−0.59), confirming results reported by Dillman et al [16] and Klang et al [22]. FCP increases with inflammatory activity due to neutrophil migration to the gastrointestinal tract and is therefore a common marker of gut inflammation [48]. Restricted diffusion as expressed by ADC in combination with FCP may therefore improve disease monitoring, detect early subclinical inflammatory processes, and lead to better patient outcomes.
One outlier of the present analysis was the study by Hectors et al [29], which showed negative results for clinical parameters. One reason for this could be the employed IVIM technique in the study. The authors reported promising results for the differentiation between normal and abnormal bowel for IVIM-DWI parameters, being superior to ADC values alone. More data are needed to elucidate the potential of the IVIM-DWI technique.
The present results can lead to the hypothesis that ADC values can be used as a valuable imaging biomarker to assess disease severity, presumably better than morphological imaging. ADC measurements may serve as a diagnostic cornerstone for treatment decisions side by side with established clinical parameters like serological inflammation markers.
Our meta-analysis has some limitations. First, many of the included studies were retrospective in nature. Second, it was not possible to standardize the different age groups throughout, and as a result, the heterogeneity was substantial. Third, the acquired data was obtained on different MRI scanners with different technical parameters (magnetic strength, b-values, and acquisition time). In addition, the patients’ preparation was not standardized. However, this reflects clinical routine with resulting heterogeneity. Unfortunately, we could not address this by further sub-analyses due to the small number of patients involved in the studies and were thus unable to perform a meta-regression analysis. Fourth, the reference standard to assess inflammation was different throughout the studies. Some used surgical specimens for inflammation, whereas others used endoscopic evaluation. Fifth, this systematic review was not filed in a register, which can result in possible bias regarding the data collection. Furthermore, despite many included studies, some of our subgroups have a small number of patients.
In conclusion, our meta-analysis shows that ADC may be a significant tool for CD disease activity, albeit for selective parameters. We identified moderate-to-strong associations between ADC and CDAI, MaRIA, and SES-CD scores. However, the role of ADC in assessing fibrotic changes in the bowel wall is limited. ADC values can reflect acute inflammatory reactions but no systemic inflammation.
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- CD:
-
Crohn’s disease
- CDAI:
-
Crohn’s disease activity index
- CRP:
-
C-reactive protein
- DWI-MRE:
-
Diffusion-weighted sequences
- FCP:
-
Fecal calprotectin
- MaRIA:
-
Magnetic resonance index of activity
- MRE:
-
Magnetic resonance enterography
- SES-CD:
-
Endoscopic activity score
References
Feuerstein JD, Cheifetz AS (2017) Crohn disease: epidemiology, diagnosis, and management. Mayo Clin Proc 92:1088–1103
Stidham RW, Higgins PDR (2018) Colorectal cancer in inflammatory bowel disease. Clinics Colon Rectal Surg 31:168–178. https://doi.org/10.1055/s-0037-1602237
Ungaro RC, Aggarwal S, Topaloglu O et al (2020) Systematic review and meta-analysis: efficacy and safety of early biologic treatment in adult and paediatric patients with Crohn’s disease. Aliment Pharmacol Ther 51:831–842
Iborra M, Juliá B, Arranz MDM et al (2019) Management and outcomes of patients with Crohn’s disease with first vs multiple surgeries: results from the PRACTICROHN study. Gastroenterol Rep 7:411–418. https://doi.org/10.1093/gastro/goz029
Rimola J, Alvarez-Cofiño A, Pérez-Jeldres T et al (2017) Increasing efficiency of MRE for diagnosis of Crohn’s disease activity through proper sequence selection: a practical approach for clinical trials. Abdom Radiol (NY) 42:2783–2791. https://doi.org/10.1007/s00261-017-1203-7
Seo N, Park SH, Kim KJ et al (2016) MR enterography for the evaluation of small-bowel inflammation in Crohn disease by using diffusion-weighted imaging without intravenous contrast material: a prospective noninferiority study. Radiology 278:762–772
Kim JS, Jang HY, Park SH et al (2017) MR enterography assessment of bowel inflammation severity in Crohn disease using the MR Index of Activity Score: modifying roles of DWI and effects of contrast phases. AJR Am J Roentgenol 208:1022–1029. https://doi.org/10.2214/AJR.16.17324
Church PC, Greer M-LC, Cytter-Kuint R et al (2017) Magnetic resonance enterography has good inter-rater agreement and diagnostic accuracy for detecting inflammation in pediatric Crohn disease. Pediatr Radiol 47:565–575. https://doi.org/10.1007/s00247-017-3790-4
Minordi LM, Larosa L, Papa A et al (2019) Assessment of Crohn’s disease activity: magnetic resonance enterography in comparison with clinical and endoscopic evaluations. J Gastrointestin Liver Dis 1(28):213–224. https://doi.org/10.15403/jgld-183. PMID: 31204402
Ninivaggi V, Missere M, Restaino G et al (2016) MR-enterography with diffusion weighted imaging: ADC values in normal and pathological bowel loops, a possible threshold ADC value to differentiate active from inactive Crohn’s disease. Eur Rev Med Pharmacol Sci 20:4540–4546
Mallio CA, Piervincenzi C, Carducci F et al (2020) Within-network brain connectivity in Crohn’s disease patients with gadolinium deposition in the cerebellum. Neuroradiology 62:833–841. https://doi.org/10.1007/s00234-020-02415-x
Choi JW, Moon WJ (2019) Gadolinium deposition in the brain: current updates. Korean J Radiol 20:134–147
Yu H, Shen YQ, Tan FQ et al (2019) Quantitative diffusion-weighted magnetic resonance enterography in ileal Crohn’s disease: a systematic analysis of intra and interobserver reproducibility. World J Gastroenterol 25:3619–3633. https://doi.org/10.3748/wjg.v25.i27.3619
Choi SH, Kim KW, Lee JY et al (2015) Diffusion-weighted magnetic resonance enterography for evaluating bowel inflammation in Crohn’s disease: a systematic review and meta-analysis. Inflamm Bowel Dis 22:669–679. https://doi.org/10.1097/MIB.0000000000000607
Kim PH, Yoon HM, Jung AY, Lee JS, Cho YA (2022) Diagnostic performance of diffusion-weighted imaging for evaluation of bowel inflammation in paediatric inflammatory bowel disease: a systematic review and meta-analysis. J Crohns Colitis 16:68–78
Dillman JR, Smith EA, Sanchez R et al (2016) DWI in pediatric small-bowel Crohn disease: are apparent diffusion coefficients surrogates for disease activity in patients receiving infliximab therapy? AJR Am J Roentgenol 207:1002–1008. https://doi.org/10.2214/AJR.16.16477
Zhu J, Zhang F, Luan Y, et al (2016) Can dynamic contrast-enhanced MRI (DCE-MRI) and diffusion-weighted MRI (DW-MRI) evaluate inflammation disease. Medicine (Baltimore) 95. https://doi.org/10.1097/MD.0000000000003239
Strakšyte V, Kiudelis G, Gineikiene I et al (2020) Diffusion-weighted magnetic resonance enterocolonography in assessing Crohn disease activity. Pol Arch Intern Med 130:734–740. https://doi.org/10.20452/pamw.15w487
Wu YC, Lin XH, Zheng XY et al (2020) Dynamic contrast-enhanced magnetic resonance imaging and diffusion-weighted imaging in the activity staging of terminal ileum Crohn’s disease. World J Gastroenterol 26:6057–6073. https://doi.org/10.3748/wjg.v26.i39.6057
Caruso A, Angriman I, Scarpa M et al (2020) Diffusion-weighted magnetic resonance for assessing fibrosis in Crohn’s disease. Abdom Radiol (NY) 45:2327–2335. https://doi.org/10.1007/s00261-019-02167-0
Du J fang, Lu B lan, Huang S yun, et al (2021) A novel identification system combining diffusion kurtosis imaging with conventional magnetic resonance imaging to assess intestinal strictures in patients with Crohn’s disease. Abdom Radiol (NY) 46:936–947. https://doi.org/10.1007/s00261-020-02765-3
Klang E, Kopylov U, Eliakim R, et al (2017) Diffusion-weighted imaging in quiescent Crohn’s disease: correlation with inflammatory biomarkers and video capsule endoscopy. Clin Radiol 72:798.e7-798.e13. https://doi.org/10.1016/j.crad.2017.04.006
Li XH, Sun CH, Mao R et al (2017) Diffusion-weighted MRI enables to accurately grade inflammatory activity in patients of ileocolonic Crohn’s disease: results from an observational study. Inflamm Bowel Dis 23:244–253. https://doi.org/10.1097/MIB.0000000000001001
Li XH, Mao R, Huang SY et al (2018) Characterization of degree of intestinal fibrosis in patients with Crohn disease by using magnetization transfer MR imaging. Radiology 287:494–503. https://doi.org/10.1148/radiol.2017171221
Abd-El Khalek Abd-Alrazek A, Fahmy DM (2018) Diagnostic value of diffusion-weighted imaging and apparent diffusion coefficient in assessment of the activity of Crohn disease: 1.5 or 3 T. J Comput Assist Tomogr 42:688–696. https://doi.org/10.1097/RCT.0000000000000754
Zhang MC, Li XH, Huang SY et al (2019) IVIM with fractional perfusion as a novel biomarker for detecting and grading intestinal fibrosis in Crohn’s disease. Eur Radiol 29:3069–3078. https://doi.org/10.1007/s00330-018-5848-6
Cheng J, Wang K, Leng X et al (2019) Evaluating the inflammatory activity in Crohn’s disease using magnetic resonance diffusion kurtosis imaging. Abdom Radiol (NY) 44:2679–2688. https://doi.org/10.1007/s00261-019-02013-3
Li X hua, Mao R, Huang S yun, et al (2019) Ability of DWI to characterize bowel fibrosis depends on the degree of bowel inflammation. Eur Radiol 29:2465–2473. https://doi.org/10.1007/s00330-018-5860-x
Hectors SJ, Gordic S, Semaan S et al (2019) Diffusion and perfusion MRI quantification in ileal Crohn’s disease. Eur Radiol 29:993–1002. https://doi.org/10.1007/s00330-018-5627-4
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:332–336
Zhu J, Zhang F, Luan Y et al (2016) Can dynamic contrast-enhanced MRI (DCE-MRI) and diffusion-weighted MRI (DW-MRI) evaluate inflammation disease. Medicine (Baltimore) 95:1–9. https://doi.org/10.1097/MD.0000000000003239
Tielbeek JAW, Ziech MLW, Li Z et al (2014) Evaluation of conventional, dynamic contrast enhanced and diffusion weighted MRI for quantitative Crohn’s disease assessment with histopathology of surgical specimens. Eur Radiol 24:619–629. https://doi.org/10.1007/s00330-013-3015-7
Buisson A, Hordonneau C, Goutte M et al (2015) Diffusion-weighted magnetic resonance imaging is effective to detect ileocolonic ulcerations in Crohn’s disease. Aliment Pharmacol Ther 42:452–460. https://doi.org/10.1111/apt.13287
Buisson A, Joubert A, Montoriol PF et al (2013) Diffusion-weighted magnetic resonance imaging for detecting and assessing ileal inflammation in Crohn’s disease. Aliment Pharmacol Ther 37:537–545. https://doi.org/10.1111/apt.12201
Li XH, Sun CH, Mao R et al (2015) Assessment of activity of Crohn disease by diffusion-weighted magnetic resonance imaging. Medicine (Baltimore):94. https://doi.org/10.1097/MD.0000000000001819
Caruso A, D’Incà R, Scarpa M et al (2014) Diffusion-weighted magnetic resonance for assessing ileal Crohn’s disease activity. Inflamm Bowel Dis 20:1575–1583. https://doi.org/10.1097/MIB.0000000000000128
Ream JM, Dillman JR, Adler J et al (2013) MRI diffusion-weighted imaging (DWI) in pediatric small bowel Crohn disease: correlation with MRI findings of active bowel wall inflammation. Pediatr Radiol 43:1077–1085. https://doi.org/10.1007/s00247-013-2712-3
Neubauer H, Pabst T, Dick A et al (2013) Small-bowel MRI in children and young adults with Crohn disease: retrospective head-to-head comparison of contrast-enhanced and diffusion-weighted MRI. Pediatr Radiol 43:103–114. https://doi.org/10.1007/s00247-012-2492-1
Whiting P, Rutjes AWS, Reitsma JB et al (2003) The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 3:1–13. https://doi.org/10.1186/1471-2288-3-25
Chalkidou A, Landau DB, Odell EW et al (2012) Correlation between Ki-67 immunohistochemistry and 18F-Fluorothymidine uptake in patients with cancer: a systematic review and meta-analysis. Eur J Cancer 48:3499–3513. https://doi.org/10.1016/j.ejca.2012.05.001
Zamora J, Abraira V, Muriel A et al (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6. https://doi.org/10.1186/1471-2288-6-31
Leeflang MMG, Kraaijpoel N (2008) Systematic reviews of diagnostic test accuracy in CMI. Clin Microbiol Infect 24:1115–1116
Yoon HM, Suh CH, Kim JR et al (2017) Diagnostic performance of magnetic resonance enterography for detection of active inflammation in children and adolescents with inflammatory bowel disease a systematic review and diagnostic meta-analysis. JAMA Pediatr 171:1208–1216. https://doi.org/10.1001/jamapediatrics.2017.3400
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Controll Clin Trials 7:177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Freeman HJ (2008) Use of the Crohn’s disease activity index in clinical trials of biological agents. World J Gastroenterol 14:4127–4130. https://doi.org/10.3748/wjg.14.4127
Sinha R, Rawat S (2013) MRI enterography with divided dose oral preparation: effect on bowel distension and diagnostic quality. Indian J Radiol Imaging 23:86–91. https://doi.org/10.4103/0971-3026.113623
Dai M, Zhang T, Li Q et al (2019) The bowel preparation for magnetic resonance enterography in patients with Crohn’s disease: study protocol for a randomized controlled trial. Trials:20. https://doi.org/10.1186/s13063-018-3101-x
Tibble J, Teahon K, Thjodleifsson B et al (2000) A simple method for assessing intestinal inflammation in Crohn’s disease. Gut 47:506–513. https://doi.org/10.1136/gut.47.4.506
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Alexey Surov.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was not required because no individual patient data were analyzed. Only aggregate patient data were analyzed in this meta-analysis.
Methodology
• retrospective
• meta-analysis
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thormann, M., Melekh, B., Bär, C. et al. Apparent diffusion coefficient for assessing Crohn’s disease activity: a meta-analysis. Eur Radiol 33, 1677–1686 (2023). https://doi.org/10.1007/s00330-022-09149-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09149-9