Abstract
Objectives
To describe a novel long-axis multimodal navigation assisted technique — the so-called Eiffel Tower technique — aimed at integrating recent technological improvements for the routine treatment of sacral insufficiency fractures.
Materials and methods
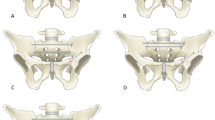
The long-axis approach described in the present study aimed at consolidating the sacral bone according to biomechanical considerations. The purpose was (i) to cement vertically the sacral alae all along and within the lateral fracture lines, resembling the pillars of a tower, and (ii) to reinforce cranially with a horizontal S1 landing zone (or dense central bone) resembling the first level of the tower. An electromagnetic navigation system was used in combination with CT and fluoroscopic guidance to overtop extreme angulation challenges. All patients treated between January 2019 and October 2021 in a single tertiary center were retrospectively reviewed.
Results
A description of the technique is provided. Twelve female patients (median age: 80 years [range: 32 to 94]) were treated for sacral insufficiency fractures with the “Eiffel Tower” technique. The median treatment delay was 8 weeks (range: 3 to 20) and the initial median pain assessed by the visual analogue scale was 7 (range: 6 to 8). Pain was successfully relieved (visual analogue score < 3) for 9 patients (75%) and persisted for 2 patients (17%). One patient was lost during the follow-up. No complication was noted.
Conclusion
The “Eiffel Tower” multimodal cementoplasty integrates recent technological developments, in particular electromagnetic navigation, with the purpose of reconstructing the biomechanical chain of the sacral bone.
Key Points
• Sacral insufficiency fractures are common and can be efficiently treated with percutaneous sacroplasty.
• The long axis sacroplasty approach can be challenging given both the shape of the sacral bone and the angulation to reach the target lesion.
• The “Eiffel Tower” technique is a novel approach using electromagnetic navigation to expand the concept of the long axis route, adding a horizontal S1 landing zone.



Similar content being viewed by others
Abbreviations
- AP :
-
Antero-posterior
- CBCT :
-
Cone-beam CT
- CT :
-
Computed tomography
- EMNS:
-
Electromagnetic navigation system
- MRI :
-
Magnetic resonance imaging
- PC :
-
Percutaneous cementoplasty
- PMMA :
-
Poly-methyl-methacrylate
- SI :
-
Sacroiliac
- SIF :
-
Sacral insufficiency fracture
- SIJ :
-
Sacroiliac joint
References
Lourie H (1982) Spontaneous osteoporotic fracture of the sacrum: an unrecognized syndrome of the elderly. JAMA 248:715–717
Santolini E, Kanakaris NK, Giannoudis PV (2020) Sacral fractures: issues, challenges, solutions. EFORT Open Rev 5:299–311
Urits I, Orhurhu V, Callan J et al (2020) Sacral insufficiency fractures: a review of risk factors, clinical presentation, and management. Curr Pain Headache Rep 24:10
Pereira LP, Clarençon F, Cormier E et al (2013) Safety and effectiveness of percutaneous sacroplasty: a single-centre experience in 58 consecutive patients with tumours or osteoporotic insufficient fractures treated under fluoroscopic guidance. Eur Radiol 23:2764–2772
Lin JT, Lane JM (2003) Sacral Stress Fractures. Journal of Women's Health 12:879–888
Garant M (2002) Sacroplasty: a new treatment for sacral insufficiency fracture. J Vasc Interv Radiol 13:1265–1267
Pommersheim W, Huang-Hellinger F, Baker M, Morris P (2003) Sacroplasty: a treatment for sacral insufficiency fractures. AJNR Am J Neuroradiol 24:1003–1007
Frey ME, Warner C, Thomas SM et al (2017) Sacroplasty: a ten-year analysis of prospective patients treated with percutaneous sacroplasty: literature review and technical considerations. Pain Physician 20:E1063–e1072
Smith DK, Dix JE (2006) Percutaneous sacroplasty: long-axis injection technique. AJR Am J Roentgenol 186:1252–1255
Kao F-C, Hsu Y-C, Chen T-S, Liu P-H, Tu Y-K (2021) Combination of long- and short-axis alar sacroplasty techniques under fluoroscopic guidance for osteoporotic sacral insufficiency fracture. J Orthop Surg Res 16:269–269
Frey ME, Depalma MJ, Cifu DX, Bhagia SM, Carne W, Daitch JS (2008) Percutaneous sacroplasty for osteoporotic sacral insufficiency fractures: a prospective, multicenter, observational pilot study. Spine J 8:367–373
Frey ME, DePalma MJ, Cifu DX, Bhagia SM, Daitch JS (2007) Efficacy and safety of percutaneous sacroplasty for painful osteoporotic sacral insufficiency fractures: a prospective, multicenter trial. Spine (Phila Pa 1976) 32:1635–1640
Durand P, Moreau-Gaudry A, Silvent AS et al (2017) Computer assisted electromagnetic navigation improves accuracy in computed tomography guided interventions: a prospective randomized clinical trial. PLoS One 12:e0173751
Moulin B, Tselikas L, De Baere T et al (2020) CT guidance assisted by electromagnetic navigation system for percutaneous fixation by internal cemented screws (FICS). Eur Radiol 30:943–949
Teriitehau C, Rabeh H, Pessis E, Sénéchal Q, Besse F, Bravetti M (2020) Reduction of patient radiation dose during percutaneous CT vertebroplasty: impact of a new computer-assisted navigation (CAN) system. Radioprotection 55:11–16
Mahmood B, Pasternack J, Razi A, Saleh A (2019) Safety and efficacy of percutaneous sacroplasty for treatment of sacral insufficiency fractures: a systematic review. J Spine Surg 5:365–371
Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH (2012) The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat 221:537–567
Peretz AM, Hipp JA, Heggeness MH (1998) The internal bony architecture of the sacrum. Spine (Phila Pa 1976) 23:971–974
Denis F, Davis S, Comfort T (1988) Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res 227:67–81
Kinoshita H, Miyakoshi N, Kobayashi T, Abe T, Kikuchi K, Shimada Y (2019) Comparison of patients with diagnosed and suspected sacral insufficiency fractures. J Orthop Sci 24:702–707
Deschamps F, de Baere T, Hakime A et al (2016) Percutaneous osteosynthesis in the pelvis in cancer patients. Eur Radiol 26:1631–1639
Premat K, Clarençon F, Bonaccorsi R, Degos V, Cormier É, Chiras J (2017) Reinforced cementoplasty using dedicated spindles in the management of unstable malignant lesions of the cervicotrochanteric region. Eur Radiol 27:3973–3982
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Pr Frederic Clarencon.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because of the type of study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boeken, T., Shotar, E., Cormier, É. et al. The “Eiffel Tower” technique: novel long-axis sacroplasty under electromagnetic navigation assistance; feasibility and descriptive study. Eur Radiol 32, 7640–7646 (2022). https://doi.org/10.1007/s00330-022-08825-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08825-0