Abstract
Objectives
Abbreviated breast MRI (AB-MRI) was introduced to reduce both examination and image reading times and to improve cost-effectiveness of breast cancer screening. The aim of this model-based economic study was to analyze the cost-effectiveness of full protocol breast MRI (FB-MRI) vs. AB-MRI in screening women with dense breast tissue for breast cancer.
Methods
Decision analysis and a Markov model were designed to model the cumulative costs and effects of biennial screening in terms of quality-adjusted life years (QALYs) from a US healthcare system perspective. Model input parameters for a cohort of women with dense breast tissue were adopted from recent literature. The impact of varying AB-MRI costs per examination as well as specificity on the resulting cost-effectiveness was modeled within deterministic sensitivity analyses.
Results
At an assumed cost per examination of $ 263 for AB-MRI (84% of the cost of a FB-MRI examination), the discounted cumulative costs of both MR-based strategies accounted comparably. Reducing the costs of AB-MRI below $ 259 (82% of the cost of a FB-MRI examination, respectively), the incremental cost-effectiveness ratio of FB-MRI exceeded the willingness to pay threshold and the AB-MRI-strategy should be considered preferable in terms of cost-effectiveness.
Conclusions
Our preliminary findings indicate that AB-MRI may be considered cost-effective compared to FB-MRI for screening women with dense breast tissue for breast cancer, as long as the costs per examination do not exceed 82% of the cost of a FB-MRI examination.
Key Points
• Cost-effectiveness of abbreviated breast MRI is affected by reductions in specificity and resulting false positive findings and increased recall rates.
• Abbreviated breast MRI may be cost-effective up to a cost per examination of 82% of the cost of a full protocol examination.
• Abbreviated breast MRI could be an economically preferable alternative to full protocol breast MRI in screening women with dense breast tissue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The superior accuracy of breast MRI in comparison with conventional imaging techniques in screening women at high risk for breast cancer has been suggested by a number of studies; several recent prospective multi-center trials have compared breast MRI to conventional imaging techniques, such as conventional mammography (XM) and ultrasound (US), underlining a higher sensitivity at comparable specificity levels [1,2,3]. However, current international guidelines still do not recommend breast MRI as a screening tool outside of high-risk screening collectives [4,5,6].
Apart from high-risk collectives, the superior diagnostic performance has also been confirmed in screening women at intermediate risk of breast cancer due to their elevated breast density [7, 8]. Dense breast tissue is associated with an increased risk of breast cancer along with a decreased sensitivity in conventional breast imaging (ACR BI-RADS categories C or D) [9].
In order to cope with the scarcity in resource allocation and to make breast MRI more affordable, abbreviated protocols (AB-MRI) have been introduced offering similar sensitivity in comparison to full protocol breast MRI (FB-MRI), yet at the expense of decreased specificity. Initially, AB-MRI was defined as solely pre- and post-contrast sequences with subtracted and maximum-intensity projection images [10]. Recently, a variety of abbreviated protocols have been evaluated. These included additional T2-weighted images, ultrafast contrast-enhanced sequences, or diffusion-weighted images as a contrast-free alternative — all reporting varying specificities [11,12,13,14].
The prospective trials of Comstock and Bakker et al have reported similar sensitivities of AB-MRI and FB-MRI in women of intermediate risk. Comstock et al described a specificity of AB-MRI of 87%, whereas Bakker et al found a specificity of 92% for the full protocol, in line with prior findings [10].
The lower specificity of AB-MRI is associated with a higher number of false positive findings and increased recall rates. Both techniques have been described to be cost-effective in screening women at intermediate risk with an incremental cost-effectiveness ratio (ICER) below commonly accepted willingness to pay thresholds of $100,000 per quality-adjusted life year (QALY) gained [15,16,17].
The lack of a broadly accepted definition for both techniques — abbreviated as well as full-scale protocols — makes the evaluation of AB-MRI in general difficult as every approach leads to a different diagnostic accuracy.
Based on recent data, reductions in specificity that are associated with abbreviating breast MRI protocols were assumed as the key determinant to model the differences between full-scale and abbreviated protocols in the present study.
Consecutively, we aim to investigate the role of AB-MRI in screening women with dense breast tissue in relation to FB-MRI with a focus on the following objectives:
-
1)
To evaluate the economic potential of AB-MRI compared to FB-MRI,
-
2)
To examine various constellations of diagnostic performance parameters and costs with regard to cost-effectiveness, and
-
3)
To determine a “cut-off” value that would allow AB-MRI to be cost-effective.
Material and methods
Screening collective and input parameters
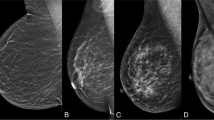
This cost-effectiveness analysis is based on recently published data on AB-MRI and FB-MRI, evaluated in prospective, multi-center screening trials and compared to x-ray-based techniques, i.e., x-ray mammography (XM) and digital breast tomosynthesis (DBT) [7, 8]. The underlying studies revealed unprecedented data on screening women at intermediate risk of breast cancer due to dense breast tissue. Both average age and pre-test probability of a malignant lesion were comparable in the screening collectives, which were reported at about 55 years and 1.6%, respectively. While the sensitivity of AB-MRI and FB-MRI was equivalent at 95.7% and 95.2%, respectively, the specificity of AB-MRI was significantly lower compared to a full protocol examination (86.7% and 92.0%, respectively). Diagnostic performance of XM was estimated based on recent literature [2, 3, 18,19,20].
Input parameters
Input parameters for this economic evaluation were collected from recent literature (Table 1) closely following international recommendations on the conduct and methodological practice of cost-effectiveness analyses [22, 33, 34].
Estimates for the quality of life (QOL) of each state of the model were extracted from literature. Based on the size of the tumor and stage of disease, lower levels of utility were assumed for larger tumors in order to reflect therapy-related differences in quality of life [26,27,28]. Long-term QOL was assumed to be impaired in patients with extensive surgery and systemic treatment as opposed to QOL after treatment of small tumors. The absence of breast cancer was characterized by unimpaired utility levels.
Medicare current procedural terminology (CPT) codes and reported average costs were used to model the costs of diagnostic procedures and breast cancer therapy [23,24,25]. Since commonly accepted costs per examination of AB-MRI are unavailable, Medicare costs of a regular MRI examination of both breasts were applied in the base case analysis and varied in sensitivity analyses. Breast cancer incidence and tumor-unrelated as well as tumor-related death rates and the probability of R0 resection and nodal disease were extracted from literature [21, 29,30,31,32].
Economic modelling and cost-effectiveness analysis
Decision model
In order to integrate results in a broader perspective and to allow for a translational comparison, we included not only MR-based screening modalities but also x-ray-based techniques. A decision model including the screening modalities was designed, and the outcomes true positive, false positive, true negative, and false negative were defined for each screening strategy (Fig. 1a). The probability of each outcome depended on the pre-test probability of a malignant lesion and the diagnostic accuracy of each modality.
a Decision-tree including the four screening strategies and the corresponding outcomes true positive, false negative, true negative, and false positive. b Markov model with Markov states and their corresponding quality of life (QOL). The likelihood of detecting a breast tumor in two-yearly screening depends on the sensitivity of the screening method. Death is possible at any state. The Markov model has been published recently and refined for this analysis and patient collective [15, 17]. AB-MRI, abbreviated breast magnetic resonance imaging; DBT, digital breast tomosynthesis; FB-MRI, full protocol breast magnetic resonance mammography; QOL, quality of life; XM, x-ray mammography
Markov model
As described in previous publications, we adapted a Markov model for two-yearly screening programs for this study [15, 35]. Markov states included the absence of disease, undetected and detected breast cancer, long-term follow-up after initial treatment and death (Fig. 1b). False positive findings resulted in follow-up examinations and loss in quality of life. False negative findings resulted in delayed detection of breast malignancy and increased likelihood of advanced disease with more invasive and costly therapies. Positive findings in XM, DBT, and FB-MRI were histologically clarified by biopsy whereas positive findings of AB-MRI were verified or followed up by a full protocol examination and in case of a confirmed finding, resulted in biopsy. A screening interval of 2 years was assumed for the collective of women with dense breast tissue.
Economic analysis
The model-based cost-effectiveness analysis was conducted with a dedicated software for economic modelling and decision analysis (TreeAge Pro 2020, TreeAge Software). The perspective of the US healthcare system was chosen and costs were measured in US-$. Outcomes were modeled by using QALYs in order to consider both the length and quality of life. International recommendations for discounting costs and outcomes at an annual discount rate of 3% were applied [22]. Various willingness to pay (WTP) thresholds of $ 50,000 per QALY and $ 100,000 per QALY were assumed [36, 37]. Costs and effects were simulated for a time frame of 30 years.
Modelling outcomes and value of AB-MRI
In the base case scenario, costs per examination of AB-MRI were assumed to equal a full protocol MRI acquisition. In subsequent deterministic sensitivity analyses, costs were reduced and the resulting cost-effectiveness was evaluated. Since the reported specificity is the main difference between abbreviated and FB-MRI, and a range of values has been reported recently, specificity was varied within plausible ranges in the sensitivity analyses.
When the cost per examination of AB-MRI is assumed smaller than the cost of FB-MRI, the incremental cost-effectiveness ratio can be calculated. When reducing the costs per examination of AB-MRI below a certain value (threshold 1), the average cumulative costs of the AB-MRI-strategy will become smaller than those of the FB-MRI-strategy. Due to its superior effectiveness, FB-MRI will still be cost-effective at a WTP threshold of $ 50,000 per QALY ($ 100,000 per QALY), until the cost per examination of AB-MRI is reduced below threshold 2 (threshold 3). AB-MRI will be the dominant strategy if costs per examination of AB-MRI are below threshold 2 or threshold 3, depending on the WTP.
In order to indicate the economic value of AB-MRI for varying costs per examination and specificity of AB-MRI, a two-way sensitivity analysis was conducted to determine the preferred modality in terms of the net monetary benefit.
Results
Cost-effectiveness analysis
Assuming the same cost per examination for AB-MRI as for a full protocol examination in the base-case analysis, i.e., $ 314 per examination, AB-MRI and FB-MRI resulted in average cumulative costs of $ 9,779 and $ 9,283 and outcomes of 19.25 and 19.26 QALYs, respectively. AB-MRI performed worse than FB-MRI in this simulation due to its inferior diagnostic performance, hence increased false positive findings and higher expenses for follow-up examinations.
To put the results in a broader perspective, we respectively included cumulative costs and outcomes for conventional imaging as well: cumulative costs and effects over a time horizon of 30 years were larger for MR-based diagnostic procedures than for x-ray-based procedures in the base case analysis (Table 2 and Fig. 2).
Cost-effectiveness graph for the screening strategies. Varying costs per examination of abbreviated breast MRI (AB-MRI) from US-$ 220 to US-$ 314 were assumed, which equals the cost of a full protocol breast MRI (FB-MRI). MR-based screening modalities result in higher effectiveness compared to x-ray-based modalities, but also higher average costs. AB-MRI, abbreviated breast magnetic resonance imaging; DBT, digital breast tomosynthesis; FB-MRI, full protocol breast magnetic resonance mammography; QALY, quality-adjusted life year; XM, x-ray mammography
Abbreviating breast MRI
In the next step, the assumed cost per examination of AB-MRI was reduced and the model outputs and the resulting cost-effectiveness were evaluated accordingly.
Reducing the cost per examination of AB-MRI resulted in decreased discounted cumulative costs over the time horizon of 30 years and improved cost-effectiveness in terms of ICER and net monetary benefits (Table 2, Fig. 3 and Fig. 4).
One-way sensitivity analysis for varying costs per examination of abbreviated breast MRI (AB-MRI). The resulting incremental cost-effectiveness ratio (ICER) of full protocol breast MRI (FB-MRI) compared to AB-MRI is indicated for varying specificities of FB-MRI (a) and varying specificities of AB-MRI (b). For a specificity of 92%, FB-MRI is cost-saving if the cost per examination of AB-MRI is larger than $ 263 (threshold 1). The ICER of FB-MRI is below a willingness to pay threshold of $100,000 per QALY if the cost per examination of AB-MRI is between $ 259 and $ 263 (threshold 2), indicating AB-MRI to be cost-effective below $ 259. AB-MRI, abbreviated breast magnetic resonance imaging; FB-MRI, full protocol breast magnetic resonance mammography; ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life year
Two-way sensitivity analysis of the net monetary benefit for varying cost per examination and varying specificity of abbreviated breast MRI (AB-MRI). The color-coded area indicates the dominant strategy at a given cost and specificity of AB-MRI. The smaller the cost and the higher the specificity of AB-MRI, the more likely it ought to be preferred to full protocol breast MRI (FB-MRI). AB-MRI, abbreviated breast magnetic resonance imaging; FB-MRI, full protocol breast magnetic resonance mammography
At a cost per examination of $ 263 for AB-MRI (84% of the MEDICARE cost of a FB-MRI examination), the average cumulative costs of both MR-based strategies were comparable (Fig. 3). When the cost per examination of $ 259 was assumed for AB-MRI (82% of the cost of a FB-MRI examination), the average cumulative costs decreased to $ 9,249. Comparing FB-MRI to AB-MRI in a collective of 1,000 women, this resulted in incremental costs of $ 31,827 and incremental effects of 0.32 QALYs for FB-MRI, which is reflected by an ICER of $ 100,000 per QALY (WTP threshold). Reducing the cost of AB-MRI below $ 259, the average cumulative costs over the time horizon of 30 years were reduced even further, so that the ICER of FB-MRI compared to AB-MRI exceeded the WTP threshold of $ 100,000 per QALY and the AB-MRI strategy ought to be preferred. This means that the cost per examination of AB-MRI would be required not to exceed $ 259 (82% of the cost of a FB-MRI examination), in order to stay cost-effective. Any cost above this threshold would deem FB-MRI a feasible and cost-effective alternative.
Sensitivity analysis
Abbreviating breast MRI affects the performance of the technique mainly in terms of specificity, i.e., its reduced specificity and a higher number of false positive findings. To evaluate the impact of varying specificities on the model outputs, sensitivity analyses were conducted. The cost cut-off at which the AB-MRI strategy may be considered cost equal to the FB-MRI strategy (threshold 1) and the threshold at which AB-MRI should be preferred over FB-MRI (threshold 2) were simulated (Table 3). For example, at a specificity of 95% for FB-MRI and 87% for AB-MRI, the cumulative costs of both strategies were equal when the cost per examination of AB-MRI was set to $ 260 (83% of the cost of a FB-MRI examination). Below costs per examination of $ 253 (81%), FB-MRI was no longer a cost-effective alternative based on a WTP threshold of $ 100,000 per QALY. This emphasizes the need for AB-MRI to not exceed $ 253 in order to stay cost-effective in this scenario.
Figure 4 indicates which strategy was to be preferred in terms of net monetary benefit when cost per examination of AB-MRI and specificity of AB-MRI were varied.
Discussion
The superior diagnostic performance of breast MRI in screening women with dense breast tissue for breast cancer in comparison to x-ray-based techniques has been investigated and confirmed in recent prospective multi-center studies [7, 8].
A significant reduction in interval cancer rates as an accepted surrogate marker for mortality [38] was observed in the DENSE trial when screening women with elevated breast tissue densities with breast MRI compared to XM [8]. A recent publication demonstrated that additionally to its diagnostic benefit, FB-MRI may also be considered cost-effective in this setting, evaluating long-term costs and outcomes of screening women at intermediate risk of breast cancer due to their elevated breast density [15].
AB-MRI was introduced in 2014 in order to reduce both examination as well as image reading time, i.e., the costs per examination, while maintaining an acceptable diagnostic performance for reasons of cost-effectiveness [10]. The initial concept by Kuhl et al comprised only one pre- and one post-contrast acquisition with computation of a first post-contrast subtracted image and a maximum-intensity projection-image. In the following years, various protocols with and without contrast agent, some only based on diffusion-weighted imaging or ultrafast contrast-enhanced sequences, have been proposed in order to make breast MRI supposedly less expensive and thereby more cost-effective [11,12,13,14]. However, the reduction in examination costs at the expense of reduced specificity must economically be considered a trade-off.
Recently, Comstock et al demonstrated a significantly higher rate of breast cancer detection for AB-MRI compared to DBT [7]. Instead of applying only one method of abbreviation, Comstock et al accepted various abbreviated protocols in their multi-center study with 48 participating imaging centers, with pre- and post-contrast sequences and T2-weighted imaging as long as a total examination time of 10 minutes was not exceeded. A recent publication demonstrated that AB-MRI may be cost-effective compared to DBT in screening women with dense breast tissue [17].
From an economical perspective, however, the degree of abbreviation and the resulting cost-effectiveness of the different forms of abbreviating protocols is of major interest when extending MR-based breast cancer screening to a population level. This led to the main goal of the present study as to determine the optimal balance of price vs. specificity of AB-MRI — assuming a standard Medicare reimbursement for breast MRI of $ 314.
A reduction of imaging specificity resulted in an increase of false positive findings and follow-up scan rates as well as a reduction in quality of life of the affected women. These downsides need to be put in relation to these cost reductions achieved by AB-MRI. However, AB-MRI has only rarely been investigated within clinical trials investigating intermediate-risk collectives. Up to this day, there is no broadly accepted definition as to the effective reduction of costs by applying different sets of abbreviated protocols. We therefore varied the costs per examination of AB-MRI in our study within our sensitivity analyses.
Comparing the specificities for breast MRI in a screening setting for women with dense breast tissue, we were able to determine a cut-off value of approximately 80% of the Medicare reimbursement of a FB-MRI examination ($ 259).
In other words: Assuming a reduced specificity of AB-MRI in an intermediate-risk population, the cost of AB-MRI should not exceed $ 259 in order to be preferred in terms of cost-effectiveness. This analysis may be considered the first step towards an understanding of the economic potential of AB-MRI on a population-based level.
However, some limitations of the model-based economic evaluation need to be considered:
The selected WTP thresholds of $ 50,000–$ 100,000 have been subject to scientific debate, yet have been applied to the U.S healthcare system by the majority of economic evaluations and represent the commonly accepted standard.
A Markov model can only represent an approximation of clinical reality and is characterized by its input parameters. The values of the diagnostic performance are based on two randomized prospective multi-center studies that were conducted in slightly different populations with different baseline risks: the DENSE trial included women with breast density category D, whereas Comstock et al included women with categories C and D. Breast tissue density hereby represents certainly only one risk factor among others that can contribute to an intermediate risk profile.
Importantly, sensitivity and specificity of breast MRI are independent from mammographic breast tissue density [39]. Therefore, the absolute values of diagnostic performance reported by Comstock and Bakker could reasonably be applied to this study population. An average pre-test probability of malignancy as reported by Comstock and Bakker and an average incidence rate were included into the economic model for comparing both screening strategies in order to deal with the heterogeneity of the two underlying studies. Further, the study design was independent from breast density as diagnostic performances of both FB-MRI and AB-MRI are unaffected by breast tissue density; the goal was merely to compare different specificity levels of the underlying methods of examination. Comparing different risk-stratified screening strategies across various screening populations with different grades of breast tissue density was not an aim of this analysis. The comparison of MR-based techniques with XM and DBT was not feasible since performance measures of x-ray-based techniques were acquired from different populations with divergent breast tissue densities.
In the DENSE concept biennial screening with conventional mammography was supplemented with breast MRI. Comstock et al on the contrary applied annual screening. Evidence-based recommendations on the selection of appropriate screening intervals for screening women with dense breasts with MRI are so far unavailable. We therefore selected a biennial screening interval for our economic evaluation, until prospective data comparing annual with biennial in terms of diagnostic performance and effects on mortality are scientifically explored further. Recent literature has suggested the potential economic value of a 4-year screening interval [40]. However, we did not include overly distant screening intervals of 4 years or more into our analysis since empirical outcome data on the interval cancer rates and stages of screening-detected breast cancer are unavailable as of today.
Additionally, both studies only describe the results of only the first screening round. However, recent findings of the second screening round of the DENSE trial indicate a decrease of false positives when breast MRI is routinely applied as a screening tool [41]. Even though the initial definition of protocol abbreviation as described by Kuhl et al suggested a FB-MRI examination after an initially suspicious finding, abbreviated protocols have not been clearly defined or standardized so far. Comstock et al included varying protocols as defined above and did not consider appending a FB-MRI examination in case of unclear findings.
Just as FB-MRI is merely defined by its fixed reimbursement and not ultimately by the composition of its protocol, further research as to the optimal degree of abbreviation and set of sequences is needed.
Further studies are required in order to analyze the role of other sources of varying specificity, such as reader experience.
At the same time, technical advances, e.g., by parallel imaging, allow for shorter examination times without possible detriments to diagnostic performance [42]. Hence, the gap between abbreviated protocols and full protocols may diminish to some extent in the future. Based on these developments, we deem recommendations on the role of AB-MRI in screening women with dense breasts premature as of today.
In conclusion, our preliminary findings offer a first delineation of the economic value of AB-MRI compared to FB-MRI and indicate certain cost thresholds that should not be exceeded in order to maintain a preferable cost-effectiveness of AB-MRI over FB-MRI.
Abbreviations
- AB-MRI:
-
Abbreviated breast MRI
- DBT:
-
Tomosynthesis
- FB-MRI:
-
Full protocol breast MRI
- ICER:
-
Incremental cost-effectiveness ratio
- MRI:
-
Magnetic resonance imaging
- PSA:
-
Probabilistic sensitivity analysis
- QALY:
-
Quality-adjusted life year
- QOL:
-
Quality of life
- WTP:
-
Willingness to pay
References
Riedl CC, Luft N, Bernhart C et al (2015) Triple-modality screening trial for familial breast cancer underlines the importance of magnetic resonance imaging and questions the role of mammography and ultrasound regardless of patient mutation status, age, and breast density. J Clin Oncol 33:1128–1135. https://doi.org/10.1200/JCO.2014.56.8626
Sardanelli F, Podo F, Santoro F et al (2011) Multicenter surveillance of women at high genetic breast cancer risk using mammography, ultrasonography, and contrast-enhanced magnetic resonance imaging (the High Breast Cancer Risk Italian 1 Study): final results. Invest Radiol 46:94–105. https://doi.org/10.1097/RLI.0b013e3181f3fcdf
Kuhl C, Weigel S, Schrading S et al (2010) Prospective multicenter cohort study to refine management recommendations for women at elevated familial risk of breast cancer: the EVA Trial. J Clin Oncol 28:1450–1457. https://doi.org/10.1200/JCO.2009.23.0839
Sardanelli F, Aase HS, Álvarez M, et al (2017) Position paper on screening for breast cancer by the European Society of Breast Imaging (EUSOBI) and 30 national breast radiology bodies from Austria, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Israel, Lithuania, Moldova, The Netherlands, Norway, Poland, Portugal, Romania, Serbia, Slovakia, Spain, Sweden, Switzerland and Turkey. Eur Radiol 27:2737–2743. 10.1007/s00330-016-4612-z
Sardanelli F, Boetes C, Borisch B et al (2010) Magnetic resonance imaging of the breast: recommendations from the EUSOMA working group. Eur J Cancer 46:1296–1316. https://doi.org/10.1016/j.ejca.2010.02.015
Mann RM, Balleyguier C, Baltzer PA et al (2015) Breast MRI: EUSOBI recommendations for women’s information. Eur Radiol 25:3669–3678. https://doi.org/10.1007/s00330-015-3807-z
Comstock CE, Gatsonis C, Newstead GM et al (2020) Comparison of abbreviated breast MRI vs digital breast tomosynthesis for breast cancer detection among women with dense breasts undergoing screening. JAMA 323:746. https://doi.org/10.1001/jama.2020.0572
Bakker MF, de Lange SV, Pijnappel RM et al (2019) Supplemental MRI screening for women with extremely dense breast tissue. N Engl J Med 381:2091–2102. https://doi.org/10.1056/NEJMoa1903986
Boyd NF, Guo H, Martin LJ et al (2007) Mammographic density and the risk and detection of breast cancer. N Engl J Med 356:227–236. https://doi.org/10.1056/NEJMoa062790
Kuhl CK, Schrading S, Strobel K et al (2014) Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection-a novel approach to breast cancer screening with MRI. J Clin Oncol Off J Am Soc Clin Oncol 32:2304–2310. https://doi.org/10.1200/JCO.2013.52.5386
Kul S, Metin Y, Kul M et al (2018) Assessment of breast mass morphology with diffusion-weighted MRI: beyond apparent diffusion coefficient. J Magn Reson Imaging 48:1668–1677. https://doi.org/10.1002/jmri.26175
Yamada T, Kanemaki Y, Okamoto S, Nakajima Y (2018) Comparison of detectability of breast cancer by abbreviated breast MRI based on diffusion-weighted images and postcontrast MRI. Jpn J Radiol 36:331–339. https://doi.org/10.1007/s11604-018-0731-6
Goto M, Sakai K, Yokota H et al (2019) Diagnostic performance of initial enhancement analysis using ultra-fast dynamic contrast-enhanced MRI for breast lesions. Eur Radiol 29:1164–1174. https://doi.org/10.1007/s00330-018-5643-4
Strahle DA, Pathak DR, Sierra A et al (2017) Systematic development of an abbreviated protocol for screening breast magnetic resonance imaging. Breast Cancer Res Treat 162:283–295. https://doi.org/10.1007/s10549-017-4112-0
Kaiser CG, Dietzel M, Vag T, Froelich MF (2020) Cost-effectiveness of MR-mammography vs conventional mammography in screening patients at intermediate risk of breast cancer - a model-based economic evaluation. Eur J Radiol:109355. https://doi.org/10.1016/j.ejrad.2020.109355
Froelich MF, Kaiser CG (2020) Cost-effectiveness of MR-mammography as a solitary imaging technique in women with dense breasts: an economic evaluation of the prospective TK-Study. Eur Radiol. https://doi.org/10.1007/s00330-020-07129-5
Tollens F, Baltzer PAT, Dietzel M et al (2021) Cost-effectiveness of digital breast tomosynthesis vs. abbreviated breast MRI for screening women with intermediate risk of breast cancer-how low-cost must MRI be? Cancers 13. https://doi.org/10.3390/cancers13061241
Pisano ED, Hendrick RE, Yaffe MJ et al (2008) Diagnostic accuracy of digital versus film mammography: exploratory analysis of selected population subgroups in DMIST. Radiology 246:376–383. https://doi.org/10.1148/radiol.2461070200
Leach MO, Boggis CRM, Dixon AK et al (2005) Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study (MARIBS). Lancet 365:1769–1778. https://doi.org/10.1016/S0140-6736(05)66481-1
Kuhl CK, Schrading S, Leutner CC et al (2005) Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol Off J Am Soc Clin Oncol 23:8469–8476. https://doi.org/10.1200/JCO.2004.00.4960
Richardson LC (2016) Patterns and trends in age-specific black-white differences in breast cancer incidence and mortality – United States, 1999–2014. MMWR Morb Mortal Wkly Rep 65:. 10.15585/mmwr.mm6540a1
Sanders GD, Neumann PJ, Basu A et al (2016) Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA 316:1093–1103. https://doi.org/10.1001/jama.2016.12195
Fleming MM, Hughes DR, Golding LP et al (2019) Digital breast tomosynthesis implementation: considerations for emerging breast cancer screening bundled payment models. J Am Coll Radiol 16:902–907. https://doi.org/10.1016/j.jacr.2018.11.025
Hunter SA, Morris C, Nelson K et al (2017) Digital breast tomosynthesis: cost-effectiveness of using private and Medicare insurance in community-based health care facilities. AJR Am J Roentgenol 208:1171–1175. https://doi.org/10.2214/AJR.16.16987
Blumen H, Fitch K, Polkus V (2016) Comparison of treatment costs for breast cancer, by tumor stage and type of service. Am Health Drug Benefits 9:23–32
Brady MJ, Cella DF, Mo F et al (1997) Reliability and validity of the functional assessment of cancer therapy-breast quality-of-life instrument. J Clin Oncol Off J Am Soc Clin Oncol 15:974–986. https://doi.org/10.1200/JCO.1997.15.3.974
Ahern CH, Shih Y-CT, Dong W et al (2014) Cost-effectiveness of alternative strategies for integrating MRI into breast cancer screening for women at high risk. Br J Cancer 111:1542–1551. https://doi.org/10.1038/bjc.2014.458
Polsky D, Mandelblatt JS, Weeks JC et al (2003) Economic evaluation of breast cancer treatment: considering the value of patient choice. J Clin Oncol 21:1139–1146. https://doi.org/10.1200/JCO.2003.03.126
Arias E (2019) United States Life Tables, 2017. Natl Vital Stat Rep 68:1–66
Wishart GC, Azzato EM, Greenberg DC et al (2010) PREDICT: a new UK prognostic model that predicts survival following surgery for invasive breast cancer. Breast Cancer Res 12:R1. https://doi.org/10.1186/bcr2464
Lombardi A, Pastore E, Maggi S et al (2019) Positive margins (R1) risk factors in breast cancer conservative surgery. Breast Cancer (Dove Med Press) 11:243–248. https://doi.org/10.2147/BCTT.S210788
Heil J, Rauch G, Szabo AZ et al (2013) Breast cancer mastectomy trends between 2006 and 2010: association with magnetic resonance imaging, immediate breast reconstruction, and hospital volume. Ann Surg Oncol 20:3839–3846. https://doi.org/10.1245/s10434-013-3097-0
Husereau D, Drummond M, Petrou S et al (2013) Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Value Health 16:e1–e5. https://doi.org/10.1016/j.jval.2013.02.010
Husereau D, Drummond M, Petrou S et al (2013) Consolidated Health Economic Evaluation Reporting Standards (CHEERS)--explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health 16:231–250. https://doi.org/10.1016/j.jval.2013.02.002
Kaiser CG, Dietzel M, Vag T et al (2021) Impact of specificity on cost-effectiveness of screening women at high risk of breast cancer with magnetic resonance imaging, mammography and ultrasound. Eur J Radiol 137:109576. https://doi.org/10.1016/j.ejrad.2021.109576
Cameron D, Ubels J, Norström F (2018) On what basis are medical cost-effectiveness thresholds set? Clashing opinions and an absence of data: a systematic review. Glob Health Action 11:. https://doi.org/10.1080/16549716.2018.1447828
Woods B, Revill P, Sculpher M, Claxton K (2016) Country-level cost-effectiveness thresholds: initial estimates and the need for further research. Value Health 19:929–935. https://doi.org/10.1016/j.jval.2016.02.017
Perry N, Broeders M, de Wolf C et al (2008) European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition--summary document. Ann Oncol 19:614–622. https://doi.org/10.1093/annonc/mdm481
Benndorf M, Baltzer PAT, Vag T et al (2010) Breast MRI as an adjunct to mammography: does it really suffer from low specificity? a retrospective analysis stratified by mammographic BI-RADS classes. Acta Radiol 51:715–721. https://doi.org/10.3109/02841851.2010.497164
Geuzinge HA, Bakker MF, Heijnsdijk EAM et al (2021) Cost-effectiveness of magnetic resonance imaging screening for women with extremely dense breast tissue. J Natl Cancer Inst djab119. https://doi.org/10.1093/jnci/djab119
Veenhuizen SGA, de Lange SV, Bakker MF et al (2021) Supplemental breast MRI for women with extremely dense breasts: results of the second screening round of the DENSE Trial. Radiology 203633. https://doi.org/10.1148/radiol.2021203633
Filli L, Ghafoor S, Kenkel D et al (2016) Simultaneous multi-slice readout-segmented echo planar imaging for accelerated diffusion-weighted imaging of the breast. Eur J Radiol 85:274–278. https://doi.org/10.1016/j.ejrad.2015.10.009
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is CG Kaiser.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Several of the authors have significant statistical expertise.
Informed consent
Written informed consent was not required for this study.
Ethical approval
Institutional Review Board was not required.
Methodology
• not applicable
• not applicable
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tollens, F., Baltzer, P.A.T., Dietzel, M. et al. Economic potential of abbreviated breast MRI for screening women with dense breast tissue for breast cancer. Eur Radiol 32, 7409–7419 (2022). https://doi.org/10.1007/s00330-022-08777-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08777-5