Abstract
Objectives
To investigate the ability of the currently used ultrasound-based malignancy risk stratification systems for thyroid neoplasms (ATA, AACE/ACE/AME, K-TIRADS, EU-TIRADS, ACR-TIRADS and C-TIRADS) in distinguishing follicular thyroid carcinoma (FTC) from follicular thyroid adenoma (FTA). Additionally, we evaluated the ability of these systems in correctly determining the indication for biopsy.
Methods
Three hundred twenty-nine follicular neoplasms with definitive postoperative histopathology were included. The nodules were categorized according to each of six stratification systems, based on ultrasound findings. We dichotomized nodules into the positive predictive group of FTC (high and intermediate risk) and negative group of FTC based on the classification results. Missed biopsy was defined as neoplasms that were diagnosed as FTCs but for which biopsy was not indicated based on lesion classification. Unnecessary biopsy was defined as neoplasms that were diagnosed as FTAs but for whom biopsy was considered indicated based on classification. The diagnostic performance and missed and unnecessary biopsy rates were evaluated for each stratification system.
Results
The area under the curve of each system for distinguishing follicular neoplasms was < 0.700 (range, 0.511–0.611). The missed biopsy rates were 9.0–22.4%. The missed biopsy rates for lesions ≤ 4 cm and lesions sized 2–4 cm were 16.2–35.1% and 0–20.0%, respectively. Unnecessary biopsy rates were 65.3–93.1%. In ≤ 4 cm group, the unnecessary biopsy rates were 62.2–89.7%.
Conclusion
The malignancy risk stratification systems can select appropriate nodules for biopsy in follicular neoplasms, while they have limitations in distinguishing follicular neoplasms and reducing unnecessary biopsy. Specific stratification systems and recommendations should be established for follicular neoplasms.
Key Points
• Current ultrasound-based malignancy risk stratification systems of thyroid nodules had low efficiency in the characterization of follicular neoplasms.
• The adopted stratification systems showed acceptable performance for selecting FTC for biopsy but unsatisfactory performance for reducing unnecessary biopsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Both follicular thyroid adenoma (FTA) and follicular thyroid carcinoma (FTC) originate from follicular cells [1]. FTC is the second most common thyroid malignancy accounting for 10–15% of all malignant thyroid tumors. FTC shows a high propensity for hematogenous spread and 15% to 27% of these patients develop distant metastasis [2, 3]. Compared with papillary thyroid carcinoma (PTC), which is the most common subtype of thyroid cancer (approximately 80%), patients with FTC have a twofold higher risk of lung metastasis and tenfold higher risk of bone metastasis resulting in worse survival outcomes [2, 4, 5]. However, preoperative differentiation of FTC from its benign counterpart (FTA) is an inherently challenging aspect of management of thyroid nodules.
Ultrasound is the first-line imaging tool to evaluate the risk of malignancy and for formulating the optimal management strategy, including determining the indication for fine-needle aspiration (FNA), and informing treatment decision-making (surgical resection, monitoring, or no follow-up) [6]. Use of a single parameter for ultrasound evaluation may lead to inter-observer variability resulting in suboptimal sensitivity and specificity [7]. To standardize the evaluation of malignant thyroid nodules, various clinical societies have recently developed ultrasound-based malignancy risk stratification systems [8,9,10,11,12,13]. Based on the different versions of the Thyroid Imaging Reporting and Data System (TIRADS), several “pattern-based” systems and “score-based” systems have been established. The former are represented by 2015 ATA (American Thyroid Association), AACE/ACE/AME (American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinology), K-TIRADS (Korean Society of Thyroid Radiology), and EU-TIRADS (European Thyroid Association). The latter include ACR-TIRADS (American College of Radiology) and C-TIRADS (2020 Chinese Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules). All these systems have shown reliable performance for the diagnosis and for selecting candidates for FNA [14,15,16,17].
As mentioned above, there are considerable differences in the incidence rates of various thyroid cancer subtypes [2]. In previous studies that evaluated these systems, the vast majority of malignant specimens were PTCs (88.9 to 99.6%) [18], which may have introduced an element of bias. Ultrasonographic features of FTC and PTC are considerably different [3]. The established malignant features, including hypoechogenicity, irregular margins, microcalcifications, and nonparallel orientation, are more common in PTC than in FTC.
Currently, few studies have focused on the value of ultrasound-based malignancy risk stratification systems in patients with follicular neoplasms [19,20,21]. The performance of these systems in distinguishing FTC from FTA and in correctly determining the indications for biopsy is uncertain. Thus, we hypothesized that the relevant conclusions reported in the past could not be simply extrapolated to follicular tumors.
In this study, we aimed to investigate the performance of the currently used systems in the context of follicular neoplasms. For this purpose, we compared the ability of the current systems in distinguishing FTC from FTA. Additionally, we assessed whether these systems can help identify the nodules that require a biopsy and can reduce the rate of unnecessary biopsies.
Materials and methods
This retrospective study was approved by the Institutional Review Board, and the requirement for informed consent to review images and medical records was waived.
Patients
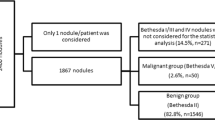
From January 2014 to May 2020, 441 consecutive patients (455 nodules) with thyroid follicular neoplasms proven by histopathological examination of the surgical specimens following thyroidectomy at a tertiary referral center were included in this study. Fourteen patients were pathologically confirmed to have two lesions each (4 with FTCs and 10 with FTAs). For these patients, the larger nodule among the two lesions was selected. The exclusion criteria were as follows: absence of preoperative thyroid US images (n = 55); uncertain match between imaging findings and histopathological results (n = 8). Because hyperfunctioning nodules do not require FNA [8], definitive or suspected hot nodules were also excluded (n = 49).
Ultrasonography
Ultrasonography examinations of thyroid glands and cervical regions were performed with Aplio 500 (Toshiba Medical System), HI Vision Ascendus (Hitachi Medical Corporation), or HI Vision Preirus (Hitachi Medical Corporation) ultrasound instruments equipped with 5–12-MHz linear array transducers. The following ultrasound features of each neoplasm were recorded and reviewed by 2 researchers who were blinded to the diagnosis: maximum diameter (cm); location (left, right, or isthmus); composition (spongiform, cystic, mixed, or solid); echogenicity (anechoic, hyperechoic, isoechoic, hypoechoic, or very hypoechoic); margin (smooth, ill-defined, or irregular); calcification (absent, microcalcification, macrocalcification, or rim calcification); shape (round to oval or irregular); orientation in transverse view (parallel or nonparallel); hypoechoic peripheral halo (absence or presence); vascularization (absent, perinodular, intranodular, or mixed); and the location of the solid component for mixed-content nodules (eccentric or non-eccentric). The presence of other hyperechoic foci (comet-tail artifacts or indeterminate), extrathyroidal extension, and suspicious cervical lymph node was also investigated. Any disagreement between the 2 researchers with respect to these features was resolved by consensus.
Categorization according to the risk stratification systems
Based on retrospective analysis of ultrasound features, each thyroid nodule was categorized using the six stratification systems: 2015 ATA, AACE/ACE/AME, K-TIRADS, EU-TIRADS, ACR-TIRADS, and C-TIRADS [8,9,10,11,12,13]. For statistical analysis, firstly, the nodules were dichotomized into the positive predictive group of FTC (high and intermediate suspicion according to 2015 ATA; high and intermediate risk according to AACE/ACE/AME; high and intermediate suspicion according to K-TIRADS; high and intermediate risk according to EU-TIRADS; category 4 and 5 according to ACR TI-RADS; category 4B to 5 according to C-TIRADS) and negative predictive group of FTC (benign, very low, and low suspicion according to 2015 ATA; low risk according to AACE/ACE/AME; benign and low suspicion according to K-TIRADS; benign and low risk according to EU-TIRADS; category 1 to 3 according to ACR-TIRADS; category 2 to 4A according to C-TIRADS).
Secondly, based on the risk stratification recommendations, the nodules were retrospectively divided into 2 categories: “indication for FNA” and “no indication for FNA” (Supplementary 1). Missed biopsy was defined as any case of FTC nodule for which FNA was not indicated based on the risk stratification system. Unnecessary biopsy was defined as any case of FTA for which FNA was considered indicated based on the risk stratification system. Missed biopsy rate and unnecessary biopsy rate were calculated for each of the six systems.
In addition, nodules that did not conform to any category according to the systems were included in the non-classifiable group. For non-classifiable nodules, FNA was only considered to be recommended if suspicious cervical lymph nodes were present.
Data and statistical analysis
Nominal and ordinal variables are expressed as frequencies and proportions, while continuous variables were expressed as mean ± standard deviation (SD) and range. Between-group differences with respect to demographic, clinical, and ultrasound features were assessed using independent two-sample t test or rank-sum test for continuous variables and chi-square test or Fisher’s exact test for nominal variables. Data pertaining to the distribution of lesions in various categories according to the risk stratification systems were analyzed using Mann–Whitney U test or Kruskal–Wallis test for ordinal variables. Based on the established cutoff, diagnostic performance of the systems was assessed using receiver operating characteristic (ROC) curve analysis. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and area under the ROC curves (AUC) were calculated with 95% confidence intervals (95% CI). AUCs of each system were compared using the DeLong method. Missed biopsy rates and unnecessary biopsy rates were compared using Cochran’s Q test, respectively. All statistical analyses were performed using SPSS (version 23.0, IBM) or MedCalc software (version 19.0.4) software. Two-sided p values < 0.05 were considered indicative of statistical significance.
Results
A total of 329 patients (329 nodules) were included in this study. These included 216 (65.7%) women and 113 (34.3%) men; the mean age of patients was 43.5 ± 14.3 years (range, 3–82).
Baseline
Of the 329 follicular neoplasms, 262 (79.6%) were diagnosed as FTAs and 67 (20.4%) were diagnosed as FTCs based on histopathological examination of surgical specimens The mean maximum diameter of the follicular neoplasms was 3.6 ± 1.7 cm (range, 0.6–12.1). The most common ultrasound presentation of follicular neoplasm in our cohort was solid (76.3%), isoechoic (79.0%), smooth margin (92.1%), non-calcification (85.7%), round to oval (96.0%), and parallel (99.7%) nodule with peripheral halo (59.0%) and mixed vascularization (93.1%) (Table 1). There were no significant differences between FTA and FTC with respect to age, sex, maximum diameter, nodule location, orientation, peripheral halo, extrathyroidal extension, or other hyperechoic foci (comet-tail artifacts or indeterminate) (p > 0.05). However, there were significant differences with respect to following ultrasound features: hypoechoic (15.3% vs 26.9%, p = 0.026), ill-defined margin (4.2% vs 20.9%, p < 0.001), calcifications (10.7% vs 20.84%, p < 0.001), microcalcifications (3.1% vs 11.9%, p = 0.003), irregular shape (1.1% vs 14.9%, p < 0.001), suspicious cervical lymph node (0% vs 4.5%, p = 0.008), and the location of the solid component in mixed-content nodules (25.4% vs 80.0%, p = 0.023) (detailed comparisons among FTC subtypes in Supplementary 2).
The most frequent classification was low suspicion by 2015 ATA (64.7%), intermediate risk by AACE/ACE/AME (89.0%), low suspicion by K-TIRADS (78.5%), low risk by EU-TIRADS (76.5%), TR3 by ACR-TIRADS (56.3%), and TR4A by C-TIRADS (68.1%) (Table 1). Statistical comparisons between FTA and FTC showed significant differences in distributions according to the six systems respectively, while no significant difference was found among FTC subtypes (Table 2).
Performance of the stratification systems
The diagnostic indices of the six systems depending on predictive classifications are presented in Table 3. The AUCs for the six systems ranged from 0.511 to 0.611. K-TIRADS, EU-TIRADS, ACR-TIRADS, and C-TIRADS indicated statistical value for FTC (AUCs = 0.573–0.611, p < 0.05). The AUC of C-TIRADS for differentiating FTC from FTA was the highest among all systems (0.611; 95% CI, 0.556–0.664) (sensitivity: 26.9% (95% CI, 16.8 to 39.1%); specificity: 95.4% (95% CI, 92.1 to 97.6%); PPV: 60.0% (95% CI, 43.2 to 74.7%); NPV: 83.6% (95% CI, 81.5 to 85.5%)). AUCs of the statistical value systems were no significant difference (p > 0.05).
Notably, of the 27 non-classifiable nodules (8.2%, 27 of 329) according to 1 or more systems, 14 (20.9%, 14 of 67) were FTCs and 13 (5.0%, 13 of 262) were FTAs (Table 4). All cases were classifiable according to ACR-TIRADS and C-TIRADS.
The performance of the six systems in correctly determining the indication for biopsy and reducing unnecessary biopsy is shown in Table 5. The lowest missed biopsy rate was found with K-TIRADS (9.0%), and the highest with ACR-TIRADS and AACE/ACE/AME (22.4%). The missed biopsy rates were significantly different between the six systems (p = 0.049), but not in pairwise comparisons. ACR-TIRADS was associated with the lowest unnecessary biopsy rate (65.3%), while K-TIRADS was associated with the highest unnecessary biopsy rate (93.1%). The unnecessary biopsy rates were significantly different among the six systems (p < 0.001). The unnecessary biopsy rates of ACR-TIRADS (65.3%) and C-TIRADS (67.9%) were lower than those of the other systems.
We further performed sub-group analysis based on nodule size. The missed biopsy rates for lesions ≤ 4 cm ranged from 16.2 to 35.1%; the missed biopsy rates for lesions sized 2–4 cm ranged from 0 to 20.0%; there was no significant difference between the six systems with respect to missed biopsy rate for lesions ≤ 4 cm or lesions sized 2–4 cm (p = 0.135 and p = 0.075, respectively). The systems with the lowest and highest unnecessary biopsy rate for lesions ≤ 4 cm were ACR-TIRADS (62.2%) and K-TIRADS (89.7%), respectively. The unnecessary biopsy rates (≤ 4 cm) were significantly different among the six systems (p < 0.001). ACR-TIRADS (62.2%) and C-TIRADS (70.5%) had lower unnecessary biopsy rates than the other systems.
Discussion
Our study showed that the stratification systems did not help distinguish FTA from FTC. In addition, while the systems showed acceptable performance for correctly determining the indication for biopsy in FTC, the performance with respect to reducing unnecessary biopsy was unsatisfactory.
In this study, on using high or intermediate suspicious stratification as the positive cutoff for FTC, the AUCs of all six systems (0.511 to 0.611) were less than 0.700. A Korean study that focused on the performance of K-TIRADS in classifying follicular neoplasms found the low efficiency of K-TIRADS using the same cutoff (AUC = 0.575, p = 0.439) [19]. However, Liu et al reported acceptable performances of 2015 ATA (AUC = 0.744, p < 0.001) and ACR-TIRADS (AUC = 0.744, p < 0.001) for distinguishing follicular neoplasms [20]. In our study, AUCs of K-TIRADS, EU-TIRADS, ACR-TIRADS, and C-TIRADS were disappointing (AUC = 0.573–0.611, p < 0.05). It may be difficult to improve clinical management of nodules based on these systems. The poor performance is attributable to the fact that follicular neoplasms present with substantially overlapping ultrasound features, and FTCs rarely present with features favoring malignancy as described in the current systems, such as nonparallel, markedly hypoechoic, irregular margin, and microcalcifications [3, 22, 23]. A recent meta-analysis identified sonographic features for differentiating between FTA and FTC and found that tumor protrusion, presence of calcifications (irrespective of type), irregular margins, marked hypoechogenicity, and irregular shape were associated with high risk of FTC [24]. Our group found similar high-risk features, such as presence of calcifications (10.7% vs 20.84%, p < 0.001) and irregular shape (1.1% vs 14.9%, p < 0.001). Therefore, future systems may need to reassess the significance of these features in distinguishing follicular neoplasms.
In addition, our study found that “pattern-based” systems (2015 ATA, AACE/ACE/AME, K-TIRADS, and EU-TIRADS) had more limitations in the classification of follicular neoplasms than previously reported in the literature [19,20,21], in contrast to the “score-based” systems (ACR-TIRADS and C-TIRADS). Given the limitations of pattern-based systems in the classification of follicular neoplasms, these systems should incorporate findings, such as undetermined composition, irregular shape, iso/hyperechoic with microcalcification and ill-defined margin (Table 4), or switch to “score-based” systems in the future.
In our cohort, the missed biopsy rates for all FTCs ranged from 9.0 to 22.4% and for FTCs ≤ 4 cm ranged from 16.2 to 35.1%, which is concordant with the study by Castellana et al [21] in which 0 to 31% of FTCs were missed. Therefore, we believe that all six systems assessed in this study are effective tools to select FTC for FNA in clinical practice. In fact, previous studies have shown that follicular neoplasms are large [22,23,24,25,26,27]. The mean maximum diameter of FTC (3.9 ± 2.1 cm) in our study was higher than any threshold proposed for ultrasound-based malignancy risk stratification systems. The highest maximum diameter was up to 12.1 cm, which is the main reason for the high performance in selecting FTC for FNA. Besides, the size of FTC at the time of management is important. FTCs larger than 2 cm have a higher risk of distant metastasis and are associated with worse prognosis [28]. In our study, a satisfactory performance (0 to 20.0%) was also seen for FTCs sized 2 to 4 cm. Apart from unclassifiable nodules, missed FTCs were classified as category 2 and 3 by ACR-TIRADS, and as category 3 by C-TIRADS. There were 4 FTC lesions that were missed by both systems, including a solid isoechoic nodule and three mixed (predominantly solid) isoechoic nodules, which are generally considered indicative of benignity. Therefore, meticulous care should be exercised while managing non-high risk nodules as well.
However, correctly determining the indication for biopsy is only a step towards further diagnostic workup, since the definitive distinction between follicular neoplasms is only based on postoperative histopathology [3]. The risk of malignancy associated with a FNA reading of Bethesda IV (follicular neoplasm or suspicious for a follicular neoplasm) is 10–40% and that with Bethesda III (atypia of undetermined significance or follicular lesion of undetermined significance) is 6–18% [29]. The possibility of FTC in lesions with the above suspicious malignant cytological findings is uncertain. In previous studies, 10.8% follicular neoplasm (FN) and 1.2% follicular lesion of undetermined significance (FLUS) were eventually found to be FTCs [30, 31]. As an extreme example, 1379 thyroid nodules with FNA findings consistent with FN were not diagnosed as FTC after surgery [32]. Other studies have shown that the efficacy of TIRADS depends on the incidence of PTC in the study population [33] and that suspicious ultrasound features may not be useful in predicting malignancy of FLUS [34]. Therefore, due discretion is required due to the limitations of cytology in the diagnosis of FTC.
In previous studies involving papillary carcinoma as the primary malignant tumor, unnecessary biopsy rates with ultrasound-based malignancy risk stratification systems were generally lower than 50% [14,15,16,17]. However, our study found higher unnecessary biopsy rates in patients with follicular neoplasm. In our study, FNA was considered indicated for 65.3% to 93.1% of all FTAs and for 62.2% to 89.7% of FTAs sized ≤ 4 cm. We believe that this result is mainly due to the large size of follicular neoplasms [22,23,24,25,26,27]. Furthermore, our study showed that the unnecessary biopsy rates with use of “pattern-based” systems were higher than those with use of “score-based” systems irrespective of the lesion size because of the different criteria for determining the indications for biopsy. According to “pattern-based” systems, FNA is not indicated only when nodules with special patterns exceed the above size threshold [8,9,10,11], such as entirely spongiform and pure cyst nodules (3.3% and 0% of FTAs, respectively). In “score-based” systems [12, 13], FNA is not indicated for nodules that are classified as category 1 and 2 by ACR-TIRADS or as category 2 and 3 by C-TIRADS, irrespective of the size. In our study, a certain proportion of FTAs was categorized in the “no biopsy” group by the ACR-TIRADS and C-TIRADS (23.6% and 26.4% of FTAs, respectively).
Currently, there is an impetus on reducing unnecessary biopsy of thyroid nodules, because of the low rate of malignancy and the generally good prognosis of the most common thyroid malignancy (PTC) [8]. Nevertheless, FTC exhibits a more aggressive biological behavior than PTC. Although the precise diagnosis of follicular neoplasms requires postoperative histopathology, preoperative biopsy and further molecular testing may provide supplementary information aiding the differential diagnosis of follicular neoplasms [35]. Thus, deliberately avoiding biopsy and further testing for follicular neoplasms require careful consideration. Recently, some studies have demonstrated the value of molecular testing for follicular neoplasms. For example, a study using next-generation sequencing reported that the presence of FLT3 and TP53 with no RET mutations was consistent with FTC and the absence of FLT3 and TP53 with the presence of RET mutations was consistent with FTA [36]. Another study investigating DNA methylation haplotype block markers identified 70 DNA methylation markers that were significantly different between the FTC and FTA samples [37].
There are several limitations of our study. First, this was a single-center retrospective study. Only patients with a confirmed postoperative diagnosis of thyroid follicular neoplasm were included. Patients who did not undergo surgery were missed, which may have introduced an element of selection bias. Additionally, 126 nodules (27.7%, 126 of 455) were excluded which may also have resulted in selection bias. Finally, only non-dynamic images were available for recording the ultrasound features which may have affected the accuracy of data.
In conclusion, the currently used malignancy risk stratification systems for thyroid nodules showed poor ability in distinguishing FTA from FTC. The performance of these systems in selecting nodules for biopsy was acceptable, but the performance with respect to reducing unnecessary biopsy was unsatisfactory. Our findings indicate the need to develop a specific stratification system and recommendations for follicular neoplasms.
Abbreviations
- 2015 ATA:
-
2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer
- AACE/ACE/AME:
-
American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinology Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules (2016 Update)
- ACR-TIRADS:
-
American College of Radiology Thyroid Imaging Reporting and Data System
- AUC:
-
Areas under the receiving operator characteristics curve
- AUS:
-
Atypia of undetermined significance
- CI:
-
Confidence intervals
- C-TIRADS:
-
2020 Chinese Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules
- EU-TIRADS:
-
European Thyroid Association Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules in Adults
- FLUS:
-
Follicular lesion of undetermined significance
- FN:
-
Follicular neoplasm
- FNA:
-
Fine-needle aspiration
- FTA:
-
Follicular thyroid adenoma
- FTC:
-
Follicular thyroid carcinoma
- K-TIRADS:
-
Revised Korean Society of Thyroid Radiology Consensus Statement and Recommendations
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- PTC:
-
Papillary thyroid carcinoma
- SD:
-
Standard deviation
- SFN:
-
Suspicious for a follicular neoplasm
- TIRADS:
-
Thyroid Imaging Reporting and Data System
References
McHenry CR, Phitayakorn R (2011) Follicular adenoma and carcinoma of the thyroid gland. Oncologist 16:585–593
Achebrook-Kilfoy B, Grogan RH, Ward MH, Kaplan E, Devesa SS (2013) Follicular thyroid cancer incidence patterns in the United States, 1980–2009. Thyroid 23:1015–1021
Grani G, Lamartina L, Durante C, Filetti S, Cooper DS (2018) Follicular thyroid cancer and Hurthle cell carcinoma: challenges in diagnosis, treatment, and clinical management. Lancet Diabetes Endocrinol 6:500–514
Chow SM, Law SC, Au SK et al (2002) Differentiated thyroid carcinoma: comparison between papillary and follicular carcinoma in a single institute. Head Neck 24:670–677
Chow SM, Law SC, Mendenhall WM et al (2002) Follicular thyroid carcinoma: prognostic factors and the role of radioiodine. Cancer 95:488–498
Durante C, Grani G, Lamartina L, Filetti S, Mandel SJ, Cooper D (2018) The diagnosis and management of thyroid nodules: a review. JAMA 319:914–924
Choi SH, Kim EK, Kim SJ, Kwak JY (2014) Thyroid ultrasonography: pitfalls and techniques. Korean J Radiol 15:267
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26:1–133
Gharib H, Papini E, Garber JR et al (2016) American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules–2016 Update. Endocr Pract 22:622–629
Shin JH, Baek JH, Chung J et al (2016) Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology Consensus Statement and Recommendations. Korean J Radiol 17:370–395
Russ G, Bonnema SJ, Erdogan MF, Durante C, Ngu R, Leenhardt L (2017) European Thyroid Association Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules in Adults: The EU-TIRADS. Eur Thyroid J 6:225–237
Tessler FN, Middleton WD, Grant EG et al (2017) ACR Thyroid Imaging, Reporting and Data System (TI-RADS): white paper of the ACR TI-RADS Committee. J Am Coll Radiol 14:587–595
Zhou JQ, Yin LX, Wei X et al (2020) 2020 Chinese guidelines for ultrasound malignancy risk stratification of thyroid nodules: the C-TIRADS. Endocrine 70:256–279
Ospina NS, Iñiguez-Ariza NM, Castro MR (2020) Thyroid nodules: diagnostic evaluation based on thyroid cancer risk assessment. BMJ. https://doi.org/10.1136/bmj.l6670
Castellana M, Castellana C, Treglia G et al (2020) Performance of five ultrasound risk stratification systems in selecting thyroid nodules for FNA. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgz170
Kim PH, Suh CH, Baek JH, Chung SR, Choi YJ, Lee JH (2020) Unnecessary thyroid nodule biopsy rates under four ultrasound risk stratification systems: a systematic review and meta-analysis. Eur Radiol. https://doi.org/10.1007/s00330-020-07384-6
Grani G, Lamartina L, Ascoli V et al (2019) Reducing the number of unnecessary thyroid biopsies while improving diagnostic accuracy: toward the “right” TIRADS. J Clin Endocrinol Metab 104:95–102
Trimboli P, Castellana M, Piccardo A et al (2020) The ultrasound risk stratification systems for thyroid nodule have been evaluated against papillary carcinoma. A meta-analysis. Rev Endocr Metab Disord. https://doi.org/10.1007/s11154-020-09592-3
Park JW, Kim DW, Kim D, Baek JW, Lee YJ, Baek HJ (2017) Korean thyroid imaging reporting and data system features of follicular thyroid adenoma and carcinoma: a single-center study. Ultrasonography 36(4):349–354
Liu BJ, Zhang YF, Zhao CK, Wang HX, Li MX, Xu HX (2020) Conventional ultrasound characteristics, TI-RADS category and shear wave speed measurement between follicular adenoma and follicular thyroid carcinoma. Clin Hemorheol Microcirc 75(3):291–301
Castellana M, Piccardo A, Virili C et al (2020) Can ultrasound systems for risk stratification of thyroid nodules identify follicular carcinoma? Cancer Cytopathol 128:250–259
Sillery JC, Reading CC, Charboneau JW, Henrichsen TL, Hay ID, Mandrekar JN (2010) Thyroid follicular carcinoma: sonographic features of 50 cases. AJR Am J Roentgenol 194(1):44–54
Ou D, Yao J, Jin J et al (2020) Ultrasonic identification and regression analysis of 294 thyroid follicular tumors. J Cancer Res Ther 16(5):1056–1062
Borowczyk M, Woliński K, Więckowska B et al (2021) Sonographic features differentiating follicular thyroid cancer from follicular adenoma-a meta-analysis. Cancers (Basel). https://doi.org/10.3390/cancers13050938
Yoon JH, Kim EK, Youk JH, Moon HJ, Kwak JY (2014) Better understanding in the differentiation of thyroid follicular adenoma, follicular carcinoma, and follicular variant of papillary carcinoma: a retrospective study. Int J Endocrinol 2014:321595
Kim H, Shin JH, Hahn SY et al (2019) Prediction of follicular thyroid carcinoma associated with distant metastasis in the preoperative and postoperative model. Head Neck 41:2507–2513
Kuo TC, Wu MH, Chen KY, Hsieh MS, Chen A, Chen CN (2020) Ultrasonographic features for differentiating follicular thyroid carcinoma and follicular adenoma. Asian J Surg 43(1):339–346
Machens A, Holzhausen HJ, Dralle H (2005) The prognostic value of primary tumor size in papillary and follicular thyroid carcinoma. Cancer 103:2269–2273
Cibas ES, Ali SZ (2017) The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid 27:1341–1346
Wu MH, Chen KY, Hsieh MS, Chen A, Chen CN (2021) Risk stratification in patients with follicular neoplasm on cytology: use of quantitative characteristics and sonographic patterns. Front Endocrinol (Lausanne) 30(12):614630
Hong HS, Lee JY (2019) diagnostic performance of ultrasound patterns by K-TIRADS and 2015 ATA Guidelines in Risk Stratification of Thyroid Nodules and Follicular Lesions of Undetermined Significance. AJR Am J Roentgenol 213(2):444–450
Conzo G, Avenia N, Ansaldo GL et al (2017) Surgical treatment of thyroid follicular neoplasms: results of a retrospective analysis of a large clinical series. Endocrine 55:530–538
Słowińska-Klencka D, Wysocka-Konieczna K, Klencki M, Popowicz B (2020) Diagnostic value of six Thyroid Imaging Reporting and Data Systems (TIRADS) in cytologically equivocal thyroid nodules. J Clin Med 9(7):2281
Baser H, Cakir B, Topaloglu O et al (2017) Diagnostic accuracy of Thyroid Imaging Reporting and Data System in the prediction of malignancy in nodules with atypia and follicular lesion of undetermined significance cytologies. Clin Endocrinol (Oxf) 86(4):584–590
Pstrag N, Ziemnicka K, Bluyssen H, Wesoly J (2018) Thyroid cancers of follicular origin in a genomic light: in-depth overview of common and unique molecular marker candidates. Mol Cancer 17:116
Borowczyk M, Szczepanek-Parulska E, Dbicki S et al (2019) Differences in mutational profile between follicular thyroid carcinoma and follicular thyroid adenoma identified using next generation sequencing. Int J Mol Sci 20(13)
Zhang H, Zhang ZZ, Liu XD et al (2021) DNA methylation haplotype block markers efficiently discriminate follicular thyroid carcinoma from follicular adenoma. J Clin Endocrinol Metab 106(4):1011–1021
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jian Kuang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
-
•retrospective
-
•diagnostic or prognostic study/observational
-
•performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lin, Y., Lai, S., Wang, P. et al. Performance of current ultrasound-based malignancy risk stratification systems for thyroid nodules in patients with follicular neoplasms. Eur Radiol 32, 3617–3630 (2022). https://doi.org/10.1007/s00330-021-08450-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08450-3