Abstract
Objectives
We evaluated the influence of image reconstruction kernels on the diagnostic accuracy of CT-derived fractional flow reserve (FFRCT) compared to invasive FFR in patients with coronary artery disease.
Methods
Sixty-nine patients, in whom coronary CT angiography was performed and who were further referred for invasive coronary angiography with FFR measurement via pressure wire, were retrospectively included. CT data sets were acquired using a third-generation dual-source CT system and rendered with medium smooth (Bv40) and sharp (Bv49) reconstruction kernels. FFRCT was calculated on-site using prototype software. Coronary stenoses with invasive FFR ≤ 0.80 were classified as significant. Agreement between FFRCT and invasive FFR was determined for both reconstruction kernels.
Results
One hundred analyzed vessels in 69 patients were included. Twenty-five vessels were significantly stenosed according to invasive FFR. Using a sharp reconstruction kernel for FFRCT resulted in a significantly higher correlation with invasive FFR (r = 0.74, p < 0.01 vs. r = 0.58, p < 0.01; p = 0.04) and a higher AUC in ROC curve analysis to correctly identify/exclude significant stenosis (AUC = 0.92 vs. AUC = 0.82 for sharp vs. medium smooth kernel, respectively, p = 0.02). A FFRCT value of ≤ 0.8 using a sharp reconstruction kernel showed a sensitivity of 88% and a specificity of 92% for detecting ischemia-causing lesions, resulting in a diagnostic accuracy of 91%. The medium smooth reconstruction kernel performed worse (sensitivity 60%, specificity 89%, accuracy 82%).
Conclusion
Compared to invasively measured FFR, FFRCT using a sharp image reconstruction kernel shows higher diagnostic accuracy for detecting lesions causing ischemia, potentially altering decision-making in a clinical setting.
Key Points
• Image reconstruction parameters influence the diagnostic accuracy of simulated fractional flow reserve derived from coronary computed tomography angiography.
• Using a sharp kernel image reconstruction algorithm delivers higher diagnostic accuracy compared to medium smooth kernel image reconstruction (gold standard invasive fractional flow reserve).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary computed tomography (CT) is an established anatomic imaging modality for exclusion and detection of coronary artery stenoses; it carries a “class I” indication for the workup of coronary artery disease (CAD) in specific patient populations. However, assessment of the physiologic relevance of coronary stenoses based on anatomy remains difficult and ischemia testing for guiding revascularization decisions is recommended.
In the absence of sufficient information from previous stress testing, the hemodynamic significance of coronary stenoses can be assessed with invasive fractional flow reserve (FFR). An FFR-based approach has repeatedly been shown to be superior to relying on angiography alone regarding clinical outcome [1,2,3,4], and FFR-based decision-making has emerged as the gold standard for performing or deferring percutaneous coronary intervention [5].
With the help of computational fluid dynamics, non-invasive FFR values are generated from coronary computed tomography angiography (cCTA) data sets (CT-derived FFR, FFRCT) and thus add hemodynamic information to pure anatomic images [6].
Several trials have reported a good correlation of FFRCT with invasive FFR. Furthermore, compared to invasive FFR, the diagnostic accuracy of FFRCT for detecting ischemia-causing coronary lesions could be shown to be better than cCTA alone [7,8,9]. Minimizing artifacts and the use of nitroglycerin and beta blocker are key factors for achieving a high diagnostic accuracy of FFRCT [7,8,9].
Since the determination of FFRCT requires a high degree of anatomic information and spatial resolution, it is conceivable that the choice of reconstruction kernels used in the process of generating CT image data sets impacts the results of FFRCT. Reconstruction kernels can be compared to image filters that determine the balance between image noise and spatial resolution within the obtained data set. A “sharp” reconstruction kernel is very useful for assessment of coronary arteries when pronounced atherosclerosis is present and especially in the presence of calcifications. The influence of image reconstruction kernels on the diagnostic performance of FFRCT has not yet been investigated.
The aim of this study was to assess the influence of using “sharp” versus “smooth” reconstruction kernels on the accuracy of FFRCT, which was determined by comparison to invasively measured FFR.
Materials and methods
Study design and patient population
This is a single-center, retrospective analysis. Patients referred for cCTA between April 2015 and February 2019 were screened for inclusion in this analysis. Exclusion criteria were non-diagnostic cCTA data sets, coronary anomalies, the presence of a chronic total obstruction or prior stent implantation in the vessel of interest, and any status post coronary artery bypass grafting as well as the presence of ostial left main or ostial right coronary stenosis. Sixty-nine patients with an invasive coronary angiogram within 2 months after cCTA and invasive FFR measurement during which the wire position was unambiguously documented by fluoroscopy were included in this study.
CT data acquisition and image reconstruction
Coronary CT angiography was performed using a third-generation dual-source CT system (Somatom Force, Siemens Healthineers). Patients with heart rates > 60 bpm were given atenolol p.o. and/or metoprolol i.v. All patients received nitroglycerin sublingually prior to the scan. The acquisition protocol was chosen according to patient characteristics. ECG-triggered prospective axial acquisition was performed in most patients. Patients with persistent heart rates > 70 bpm in spite of medication or with frequent ectopic beats were examined using spiral acquisition with retrospectively ECG-gated image reconstruction. Patients < 45 years old with heart rates < 55 bpm were examined using prospectively ECG-triggered high-pitch spiral acquisition. Coronary calcium screening CT was performed in most patients before administering contrast agent. The scan range extended from the proximal ascending aorta to the caudal aspect of the heart. For coronary CT angiography, tube voltage (ranging from 90 to 120 mV) and tube current time product (450 to 650 mAs) were adjusted to the patient’s body weight and calcium score. Contrast agent transit time was determined by giving a bolus of 10 ml of contrast agent (Ultravist 370®, Bayer vital GmbH GB Pharma). For CT angiography, 50 ml of contrast agent at a flow rate of 5 ml/s, followed by a 50-ml saline chaser (20% contrast agent) at the same flow rate, was injected.
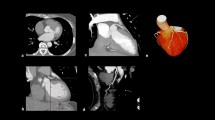
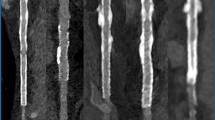
All image data sets were reconstructed with a slice thickness of 0.5 mm, increment of 0.3 mm, and a matrix of 512. Iterative reconstruction (Admire®, Siemens Healthineers) at a strength level of 2 was used for all data sets. Reconstructions were rendered using both a medium soft convolution kernel (Siemens Bv40) and a sharp convolution kernel (Siemens Bv49), with otherwise unchanged parameters (Fig. 1).
Calculation of FFR CT
FFRCT was calculated on-site using a PC-based prototype software (cFFR version 3.0, Siemens Healthineers). The program automatically renders the centerline and lumen of the vessels. Manual correction by a user blinded to invasive FFR was done where necessary. When completed, a 3D model of the coronary tree is generated with FFR values at any point on the vessel. After identifying the exact location of the FFR wire in the invasive coronary angiogram, the FFRCT value at the identical location of the simulated coronary tree was noted and compared to the invasive FFR value (Figs. 2 and 3).
Invasive FFR measurement
Invasive FFR was measured using PressureWire X Guidewire (St. Jude Medical/Abbott) after producing hyperemia with adenosine intracoronary. Coronary stenoses with invasively measured FFR ≤ 0.80 were classified as hemodynamically significant. Agreement between FFRCT using both reconstruction parameters was compared to invasive FFR.
Statistical analyses
All statistical analyses were done with IBM® SPSS® Statistics (version 24). Continuous variables are presented as mean ± standard deviation or median (interquartile range [IQR]). Wilcoxon test was used to compare groups. Results were deemed significant with a p value < 0.05. Receiver operating characteristic (ROC) curve analyses were performed and ROC curves and correlations compared with MedCalc Software Ltd.
Results
Out of 72 patients screened for inclusion in this analysis, 3 patients had to be excluded because of insufficient image quality of cCTA for the calculation of FFRCT and one patient due to technical reasons with FFRCT measurement. Sixty-nine patients (mean age 63 ± 10 years, 18 women) were included in this study. Baseline clinical characteristics are shown in Table 1.
Invasive coronary angiography was performed after a mean time of 8 days after cCTA. A total of 100 vessels were investigated both by invasive and CT-based FFR. The invasive angiographic lumen reduction of the target vessel ranged between 30 and 90% on visual analysis (mean 57%). Twenty-seven vessels had a degree of stenosis of 30– < 50%, 44 vessels showed a stenosis of 50– < 70%, while in 29 vessels a lumen reduction of 70–90% was found. In case of multiple stenoses, the pressure wire was placed after the most distal stenosis. The median invasive FFR value was 0.87 (IQR 0.14), and a total of 25 analyzed vessels (25% of all vessels) were classified as hemodynamically significantly stenosed due to an invasive FFR value of ≤ 0.8.
In most cases (57/100), the left anterior descending artery (LAD) with its side branches was the vessel of interest, followed by the circumflex coronary artery (CX, 27/100) and the right coronary artery (RCA, 16/100). The hemodynamic relevance of lesions according to invasive FFR was detected in the LAD territory in 20 cases (35% of all measured LAD), in the CX territory in 3 cases (11% of all measured CX), and in the RCA in 2 cases (13% of all measured RCA). There was a significant association between the vessel of interest and the severity of the stenosis (p = 0.027).
The median FFRCT using a medium smooth reconstruction kernel (Bv40) was 0.87 (IQR 0.11), and the median FFRCT using a sharp reconstruction kernel (Bv49) was 0.87 (IRQ 0.13). While FFRCT values simulated with Bv40 were not relevantly different compared with invasive FFR values (p = 0.26), this was the case when simulated with Bv49 (p = 0.017).
Using the sharp reconstruction kernel, a significantly closer correlation of FFRCT with invasive FFR was observed in comparison to medium smooth reconstruction kernel (r = 0.74, p < 0.0001 vs r = 0.58, p < 0.0001; direct comparison of correlation coefficients p = 0.04; scatterplots Figs. 4 and 5). ROC curve analysis showed an area under the ROC curve (AUC) of 0.92 (p < 0.001) for FFRCT using a sharp reconstruction kernel to correctly identify or exclude hemodynamically significant stenosis compared to invasive FFR, whereas a smaller AUC of 0.82 (p < 0.001) was observed for a medium smooth reconstruction kernel. This difference of AUC between Bv49 and Bv40 FFRCT was statistically significant (p = 0.02). A FFRCT value of ≤ 0.8 using sharp reconstruction kernel data sets showed a sensitivity of 88% and a specificity of 92% to detect diseased vessels causing ischemia compared to the invasive gold standard, resulting in an accuracy of 91%. The medium smooth kernel data sets performed significantly worse, having a sensitivity of 60% and specificity of 89%, resulting in an accuracy of 82% when using the same FFRCT cut-off value of ≤ 0.8. Statistical analysis [10] demonstrated the superiority of sharp kernel reconstructions regarding diagnostic accuracy when compared to medium smooth kernel reconstructions (p = 0.02).
In 46 patients, only one vessel was assessed for FFR whereas in 23 patients, more than one vessel was assessed. On a per-patient basis with one pathologic invasive FFR value indicating the presence of relevant stenoses, FFRCT with a Bv49 reconstruction kernel was able to correctly classify 61 patients. In 5 patients, the severity of stenosis was overestimated, and in 3 patients, relevant stenoses were not detected (sensitivity 88%, specificity 89%, diagnostic accuracy 88%). Using a Bv40 reconstruction kernel, only 57 patients could be correctly classified with 5 patients overestimating and 7 patients underestimating the degree of stenosis severity (sensitivity 71%, specificity 89%, diagnostic accuracy 83%). The numerically higher diagnostic accuracy of a sharp reconstruction kernel was not significantly superior to a medium smooth reconstruction kernel on a per-patient basis (p = 0.14).
Discussion
To the best of our knowledge, this is the first study to evaluate the influence of the image reconstruction kernel on FFRCT values. We could show that FFRCT using a sharper reconstruction kernel had a significantly better correlation with invasive FFR compared to a medium smooth reconstruction kernel. These results are of clinical relevance as patient-related decision-making concerning further diagnostic workup or invasive assessment critically depends on the accuracy of the FFRCT values. The higher spatial resolution of CT data sets generated by a sharper reconstruction kernel outweighs the disadvantage of increased noise, and therefore, the preferred kernel should render high-spatial-resolution data sets (often termed “sharp”). High image quality and high spatial resolution are key factors for obtaining accurate FFRCT results since the hemodynamic significance of a lesion is partly affected by the depicted degree of stenosis length and vessel diameter. Presumably, the enhanced spatial resolution offered by sharper reconstruction kernels improves automatic delineation of coronary centerlines with better lumen depiction and subsequent manual corrections can be done more confidently when needed.
Baumann and Renker et al compared invasive FFR with FFRCT by a prior version of the software used in our study. They showed a correlation similar to ours between FFRCT and invasively measured FFR (r = 0.74, p < 0.0001) in a cohort of 28 patients/36 vessels [11]. In another trial with 53 patients and 67 lesions, the results with on-site FFRCT calculation were similar: a reasonable correlation of FFRCT with invasive FFR (r = 0.66, p < 0.001) and increased diagnostic performance of FFRCT over cCTA alone for the detection of hemodynamically relevant stenosis defined by an invasive FFR < 0.8 [12]. The image reconstruction kernel was not specified in the first trial, but in the second publication, image reconstruction was performed using a vascular kernel, B26f, which corresponds to a medium smooth reconstruction kernel. A study with 71 patients/91 vessels performed in our department could demonstrate a higher correlation (r = 0.85) and high diagnostic accuracy for FFRCT compared to invasive FFR by using the sharp Bv49 kernel [13].
The mean diameter reduction in the target lesion was 57% in our study. Invasive FFR is especially suitable to evaluate lesions with intermediate stenosis, as stenosis as low as 30–50% can already have hemodynamic relevance [1] [14], while no additional benefit has been shown for lesions showing > 90% stenosis [15]. Thus, our study investigated the effect of image reconstruction kernels in a study population, which represents the daily life challenge of evaluating the usefulness of performing a percutaneous coronary intervention.
Coronary CT angiography is recommended by the guidelines of the European Society of Cardiology to clarify whether CAD causes chest pain when clinical assessment alone cannot exclude CAD [16]. However, the low specificity of cCTA to rule out hemodynamic CAD sets patients at risk of unnecessary non-invasive testing or invasive coronary angiography [17, 18]. The initial SCOT-HEART trial roused suspicion of increased invasive testing of patients presenting with chest pain who received coronary CT angiography as a first-line diagnostic tool for evaluation of chest pain [19]. However, the 5-year results of the SCOT-HEART trial could not only show a decrease in the primary endpoint, but also that the higher rate of invasive coronary angiography could only be observed in the first few months, while later no difference could be found [20]. Potentially using non-invasive FFR measurement for evaluating coronary stenoses in coronary CT angiography could have helped to reduce the number of early coronary angiographies while maintaining the positive long-term effect of increased use of antithrombotic and cholesterol-lowering agents in this cohort. Curzen et al could show that the availability of FFRCT values changes the treatment plan in about one-third of patients when added to standard coronary CT angiography [21]. The PLATFORM study also demonstrated that off-site FFRCT can safely reduce the number of invasive coronary angiographies without prognostic disadvantages in the group of patients with canceled invasive diagnostic in 1 year follow-up [22].
We could show that FFRCT performed with data reconstructed with a sharp kernel shows better results when compared to invasive FFR than a medium smooth kernel. The use of a sharp reconstruction kernel thus can help to achieve better diagnostic accuracy of non-invasive FFRCT algorithms.
Several limitations need to be acknowledged in this study. The number of patients and FFR-measured vessels are relatively small. Particularly, the number of pathologic invasive FFR values was low with 25 vessels. However, this is no sign of the low specificity of cCTA, as severely stenosed vessels were frequently not FFR-measured but directly intervened and only the intermediate stenoses were evaluated by FFR. With a mean angiographic degree of stenosis of 57%, it was to be expected that the number of pathologic FFR is rather low, owing that even in vessels with 50 to 70% stenosis, hemodynamic significance of the lesion is present only in about one-third of cases [15]. The predominance of left anterior descending artery lesions is reflecting the wider use of FFR in this vessel as a larger retrospective trial has already observed [23]. An inherent referral bias cannot be excluded as only patients with lesions deemed to be significant in cCTA were further sent for clinical invasive clarification. FFRCT measurements for both kernels were done by the same operator, so bias cannot be excluded totally, although the operator was strictly blinded for the invasive FFR value. Moreover, we analyzed the influence of the reconstruction kernel on FFRCT values within the same data set. The potential influence of other acquisition parameters on CT-derived FFR including tube current and output, and collimation and contrast opacification of the coronary arteries, was not analyzed in this cohort. Furthermore, this is a single-vendor study, and further research is needed to generalize the results to other software simulating FFRCT.
In conclusion, we could demonstrate that image reconstruction parameters have a significant impact on the diagnostic performance of FFRCT. A sharper reconstruction kernel provides a higher correlation with invasive FFR, potentially changing clinical decision-making.
Abbreviations
- AUC:
-
Area under the ROC curve
- bpm:
-
Beats per minute
- CAD:
-
Coronary artery disease
- cCTA:
-
Coronary computed tomography angiography
- CT:
-
Computed tomography
- CX:
-
Circumflex coronary artery
- FFR:
-
Fractional flow reserve
- FFRCT :
-
CT-derived FFR
- i.v.:
-
Intravenous
- IQR:
-
Interquartile range
- LAD:
-
Left anterior descending artery
- p.o.:
-
Per os
- RCA:
-
Right coronary artery
- ROC:
-
Receiver operating characteristic
References
Bech GJ, De Bruyne B, Pijls NH et al (2001) Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation 103:2928–2934
Zimmermann FM, Ferrara A, Johnson NP et al (2015) Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur Heart J 36:3182–3188
Tonino PA, De Bruyne B, Pijls NH et al (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360:213–224
Pijls NH, Fearon WF, Tonino PA et al (2010) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol 56:177–184
Authors/Task Force members, Windecker S, Kolh P et al (2014) 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 35:2541–2619
Min JK, Taylor CA, Achenbach S et al (2015) Noninvasive fractional flow reserve derived from coronary CT angiography: clinical data and scientific principles. JACC Cardiovasc Imaging 8:1209–1222
Nakazato R, Park HB, Berman DS et al (2013) Noninvasive fractional flow reserve derived from computed tomography angiography for coronary lesions of intermediate stenosis severity: results from the DeFACTO study. Circ Cardiovasc Imaging 6:881–889
Norgaard BL, Leipsic J, Gaur S et al (2014) Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 63:1145–1155
Leipsic J, Yang TH, Thompson A et al (2014) CT angiography (CTA) and diagnostic performance of noninvasive fractional flow reserve: results from the Determination of Fractional Flow Reserve by Anatomic CTA (DeFACTO) study. AJR Am J Roentgenol 202:989–994
Hawass NE (1997) Comparing the sensitivities and specificities of two diagnostic procedures performed on the same group of patients. Br J Radiol 70:360–366
Baumann S, Wang R, Schoepf UJ et al (2015) Coronary CT angiography-derived fractional flow reserve correlated with invasive fractional flow reserve measurements–initial experience with a novel physician-driven algorithm. Eur Radiol 25:1201–1207
Renker M, Schoepf UJ, Wang R et al (2014) Comparison of diagnostic value of a novel noninvasive coronary computed tomography angiography method versus standard coronary angiography for assessing fractional flow reserve. Am J Cardiol 114:1303–1308
Rother J, Moshage M, Dey D et al (2018) Comparison of invasively measured FFR with FFR derived from coronary CT angiography for detection of lesion-specific ischemia: results from a PC-based prototype algorithm. J Cardiovasc Comput Tomogr 12:101–107
Pijls NH, De Bruyne B, Peels K et al (1996) Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 334:1703–1708
Tonino PA, Fearon WF, De Bruyne B et al (2010) Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol 55:2816–2821
Knuuti J, Wijns W, Saraste A et al (2020) 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41:407–477
Meijboom WB, Meijs MF, Schuijf JD et al (2008) Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol 52:2135–2144
Douglas PS, Hoffmann U, Patel MR et al (2015) Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 372:1291–1300
The SCOT-HEART investigators (2015) CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet 385:2383–2391
SCOT-HEART Investigators, Newby DE, Adamson PD et al (2018) Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med 379:924–933
Curzen NP, Nolan J, Zaman AG, Norgaard BL, Rajani R (2016) Does the routine availability of CT-derived FFR influence management of patients with stable chest pain compared to CT angiography alone?: the FFRCT RIPCORD Study. JACC Cardiovasc Imaging 9:1188–1194
Douglas PS, De Bruyne B, Pontone G et al (2016) 1-year outcomes of FFRCT-guided care in patients with suspected coronary disease: the PLATFORM Study. J Am Coll Cardiol 68:435–445
Biasco L, Pedersen F, Lonborg J et al (2015) Angiographic characteristics of intermediate stenosis of the left anterior descending artery for determination of lesion significance as identified by fractional flow reserve. Am J Cardiol 115:1475–1480
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Fabian Ammon.
Conflict of interest
Fabian Ammon received speaker honoraria from Edwards Lifescience. Mohamed Marwan received speaker honoraria from Siemens Healthineers and Edwards Lifescience. The other authors have nothing to disclose.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because of the retrospective design of only clinically available data.
Ethical approval
Institutional Review Board approval was not required because of the retrospective design of only clinically available data
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ammon, F., Moshage, M., Smolka, S. et al. Influence of reconstruction kernels on the accuracy of CT-derived fractional flow reserve. Eur Radiol 32, 2604–2610 (2022). https://doi.org/10.1007/s00330-021-08348-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08348-0