Abstract
Objectives
To illuminate the prognostic value of ADC (apparent diffusion coefficient), an important quantitative parameter of diffusion-weighted MRI, for multiple myeloma (MM).
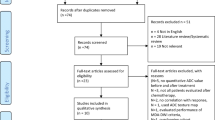
Methods
A prospective single-center study which enrolled 114 consecutive newly diagnosed MM patients with baseline whole-body diffusion-weighted MRI (WB DW-MRI) results was conducted. Baseline clinical and MRI parameters were analyzed with univariate and multivariate approaches to identify independent risk factors for progression-free survival (PFS) and overall survival (OS).
Results
Five different DW-MRI patterns were seen, and the mean ADC value of the representative background bone marrow was 0.4662 ± 0.1939 × 10−3 mm2/s. After a mean follow-up of 50.2 months (range, 15.7–75.8 months), twenty-four patients died and seven were lost to follow-up. The mean ADC value of the representative background bone marrow was showed to be an independent risk factor for both PFS (HR 4.664; 95% confidence interval (CI) 1.138–19.121; p = 0.032) and OS (HR 14.130; 95% CI 1.544–129.299; p = 0.019). Normal/salt-and-pepper pattern on DW-MRI was associated with PFS using univariate analysis (p = 0.035) but lost the significance with multivariate Cox regression.
Conclusions
Mean ADC value of the representative background bone marrow predicts both PFS and OS which suggests the role of baseline DW-MRI for risk stratification in newly diagnosed MM patients.
Key Points
• Whole-body diffusion-weighted MRI (WB DW-MRI) might be helpful to improve the current risk stratification systems for newly diagnosed multiple myeloma (MM).
• Morphological parameters as MRI pattern and focal lesion–associated parameters have been reported to be related to survival. However, important functional parameters such as apparent diffusion coefficient (ADC) values were not incorporated into the current risk stratification model.
• This study is one of the first endeavors to delineate the correlation of baseline ADC values and survival in MM patients. It is revealed that the mean ADC value of the representative background bone marrow (L3-S1 and iliac bone) was an independent risk factor for both PFS and OS.



Similar content being viewed by others
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- FISH:
-
Fluorescence in situ hybridization
- IMWG:
-
International Myeloma Working Group
- MGUS:
-
Monoclonal gammopathy of undetermined significance
- MM:
-
Multiple myeloma
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- WB DW-MRI:
-
Whole-body diffusion-weighted MRI
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66:7–30
D’Agostino M, Boccadoro M, Smith EL (2017) Novel immunotherapies for multiple myeloma. Curr Hematol Malig Rep 12:344–357
Durie BG, Salmon SE (1975) A clinical staging system for multiple myeloma. Correlation of measured myeloma cell mass with presenting clinical features, response to treatment, and survival. Cancer 36:842–854
Greipp PR, San Miguel J, Durie BG et al (2005) International staging system for multiple myeloma. J Clin Oncol 23:3412–3420
Palumbo A, Avet-Loiseau H, Oliva S et al (2015) Revised international staging system for multiple myeloma: a report from International Myeloma Working Group. J Clin Oncol 33:2863–2869
Pawlyn C, Morgan GJ (2017) Evolutionary biology of high-risk multiple myeloma. Nat Rev Cancer 17:543–556
Kyle RA, Gertz MA, Witzig TE et al (2003) Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 78:21–33
Rajkumar SV, Dimopoulos MA, Palumbo A et al (2014) International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 15:e538–e548
D’Sa S, Abildgaard N, Tighe J, Shaw P, Hall-Craggs M (2007) Guidelines for the use of imaging in the management of myeloma. Br J Haematol 137:49–63
Derlin T, Bannas P (2014) Imaging of multiple myeloma: current concepts. World J Orthop 5:272–282
Lecouvet FE, Boyadzhiev D, Collette L et al (2020) MRI versus (18)F-FDG-PET/CT for detecting bone marrow involvement in multiple myeloma: diagnostic performance and clinical relevance. Eur Radiol 30:1927–1937
Larbi A, Omoumi P, Pasoglou V et al (2019) Whole-body MRI to assess bone involvement in prostate cancer and multiple myeloma: comparison of the diagnostic accuracies of the T1, short tau inversion recovery (STIR), and high b-values diffusion-weighted imaging (DWI) sequences. Eur Radiol 29:4503–4513
Lai AYT, Riddell A, Barwick T et al (2020) Interobserver agreement of whole-body magnetic resonance imaging is superior to whole-body computed tomography for assessing disease burden in patients with multiple myeloma. Eur Radiol 30:320–327
Hillengass J, Fechtner K, Weber MA et al (2010) Prognostic significance of focal lesions in whole-body magnetic resonance imaging in patients with asymptomatic multiple myeloma. J Clin Oncol 28:1606–1610
Mai EK, Hielscher T, Kloth JK et al (2016) Association between magnetic resonance imaging patterns and baseline disease features in multiple myeloma: analyzing surrogates of tumour mass and biology. Eur Radiol 26:3939–3948
Ailawadhi S, Abdelhalim AN, Derby L et al (2010) Extent of disease burden determined with magnetic resonance imaging of the bone marrow is predictive of survival outcome in patients with multiple myeloma. Cancer 116:84–92
Mai EK, Hielscher T, Kloth JK et al (2015) A magnetic resonance imaging-based prognostic scoring system to predict outcome in transplant-eligible patients with multiple myeloma. Haematologica 100:818–825
Lee SY, Kim HJ, Shin YR, Park HJ, Lee YG, Oh SJ (2017) Prognostic significance of focal lesions and diffuse infiltration on MRI for multiple myeloma: a meta-analysis. Eur Radiol 27:2333–2347
Hillengass J, Bäuerle T, Bartl R et al (2011) Diffusion-weighted imaging for non-invasive and quantitative monitoring of bone marrow infiltration in patients with monoclonal plasma cell disease: a comparative study with histology. Br J Haematol 153:721–728
Rasche L, Angtuaco EJ, Alpe TL et al (2017) The presence of large focal lesions is a strong independent prognostic factor in multiple myeloma. Blood 132:59–66
Lacognata C, Crimì F, Guolo A et al (2017) Diffusion-weighted whole-body MRI for evaluation of early response in multiple myeloma. Clin Radiol 72:850–857
Ye ZM, Dai SJ, Yan FQ et al (2018) DCE-MRI-derived volume transfer constant (Ktrans) and DWI apparent diffusion coefficient as predictive markers of short- and long-term efficacy of chemoradiotherapy in patients with esophageal cancer. Technol Cancer Res Treat 17:1533034618765254
Xie H, Sun T, Chen M et al (2015) Effectiveness of the apparent diffusion coefficient for predicting the response to chemoradiation therapy in locally advanced rectal cancer: a systematic review and meta-analysis. Medicine (Baltimore) 94:e517
Rajkumar SV (2012) Multiple myeloma: 2012 update on diagnosis, risk-stratification, and management. Am J Hematol 87:78–88
Fonseca R, Blood E, Rue M et al (2003) Clinical and biologic implications of recurrent genomic aberrations in myeloma. Blood 101:4569–4575
Hebraud B, Magrangeas F, Cleynen A et al (2015) Role of additional chromosomal changes in the prognostic value of t(4;14) and del(17p) in multiple myeloma: the IFM experience. Blood 125:2095–2100
Zhang H, Xue H, Alto S et al (2016) Integrated shimming improves lesion detection in whole-body diffusion-weighted examinations of patients with plasma disorder at 3 T. Invest Radiol 51:297–305
Messiou C, Giles S, Collins DJ et al (2012) Assessing response of myeloma bone disease with diffusion-weighted MRI. Br J Radiol 85:e1198–e1203
Giles SL, Messiou C, Collins DJ et al (2014) Whole-body diffusion-weighted MR imaging for assessment of treatment response in myeloma. Radiology 271:785–794
Dimopoulos MA, Hillengass J, Usmani S et al (2015) Role of magnetic resonance imaging in the management of patients with multiple myeloma: a consensus statement. J Clin Oncol 33:657–664
Durie BG, Harousseau JL, Miguel JS et al (2006) International uniform response criteria for multiple myeloma. Leukemia 20:1467–1473
Messiou C, Kaiser M (2015) Whole body diffusion weighted MRI--a new view of myeloma. Br J Haematol 171:29–37
Koutoulidis V, Fontara S, Terpos E et al (2017) Quantitative diffusion-weighted imaging of the bone marrow: an adjunct tool for the diagnosis of a diffuse MR imaging pattern in patients with multiple myeloma. Radiology 282:484–493
Andrulis M, Bauerle T, Goldschmidt H et al (2014) Infiltration patterns in monoclonal plasma cell disorders: correlation of magnetic resonance imaging with matched bone marrow histology. Eur J Radiol 83:970–974
Messiou C, Collins DJ, Morgan VA et al (2011) Optimising diffusion weighted MRI for imaging metastatic and myeloma bone disease and assessing reproducibility. Eur Radiol 21:1713–1718
Jawed I, Lee CM, Tward JD et al (2007) Survival outcomes for multiple myeloma over three decades: a surveillance, epidemiology, and end results (SEER) analysis. J Clin Oncol 25(18_suppl):8019. Available via. https://doi.org/10.1200/jco.2007.25.18_suppl.8019
Funding
Institutional research funding was provided by the National Natural Science Foundation of China (81900202, for L.Z.), the Fundamental Research Funds for the Central Universities (3332018036, for L.Z.), National Public Welfare Basic Scientific Research Program of Chinese Academy of Medical Sciences (2018PT32003 and 2017PT32004, for H.-d.X), and Youth Science Foundation of Peking Union Medical College Hospital (pumch201911423, for Q.W.).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jian Li, MD, Deputy Director of the Department of Hematology, Peking Union Medical College Hospital.
Conflict of interest
The authors have no conflicts of interest.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all patients in this study.
Ethical approval
Peking Union Medical College Hospital Ethics Committee approval was obtained.
Methodology
• prospective
• diagnostic or prognostic
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 1390 kb)
Rights and permissions
About this article
Cite this article
Zhang, L., Wang, Q., Wu, X. et al. Baseline bone marrow ADC value of diffusion-weighted MRI: a potential independent predictor for progression and death in patients with newly diagnosed multiple myeloma. Eur Radiol 31, 1843–1852 (2021). https://doi.org/10.1007/s00330-020-07295-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07295-6