Abstract
Objective
To review the technical feasibility of resin microsphere (SIR-Spheres®) yttrium-90 radioembolization prescribed using the medical internal radiation dose (MIRD) model.
Methods
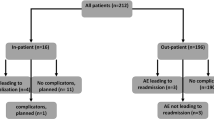
All radioembolization procedures for hepatic malignancies using resin microspheres with MIRD model between November 2015 and February 2019 were included in this IRB-approved study (n = 60). Student’s T test was used to compare prescribed activity based on MIRD and BSA models. Adverse events were assessed immediately, 30 days, and 6 months post-treatment.
Results
Sixty radioembolizations were performed in 54 patients (age 68 ± 9 years, 48–87 years, 35% female). Mean prescribed activity calculated by the MIRD model (target absorbed dose 120–200 Gy for primary and 80–200 Gy for metastatic liver cancers) was 1.7 GBq (0.3–6.4) compared with 0.6 GBq (0.12–2.1) if BSA had been used (p < 0.0001). The prescribed activity was successfully delivered in 93% (56/60) treatments. Prophylactic embolization and anti-reflux catheters were used in 20% (12/60) and 5% (3/60) treatments, respectively. No immediate post-procedural complications occurred. Abdominal pain was the most common clinical Grade 3 CTCAE in 30 days (10%) and 6 months (12%). Radiation pneumonitis occurred in 3 (5%) patients but no radiation-induced gastric ulcer or radiation-induced liver disease occurred.
Conclusion
MIRD dosimetry results in higher prescribed activity compared with BSA dosimetry with resin microspheres. MIRD prescribed activity with target absorbed doses up to 200 Gy can be successfully administered without prophylactic embolization in selected patients.
Key Points
•MIRD dosimetry results in higher prescribed activity compared with BSA dosimetry for radioembolization.
•MIRD dosimetry can be used for yttrium-90 resin microsphere radioembolization with acceptable safety profile.


Similar content being viewed by others
Abbreviations
- 3D:
-
3 Dimensional
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BSA:
-
Body surface area
- CT:
-
Computed tomography
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- ECOG:
-
Eastern Cooperative Oncology Group Performance Status
- HCC:
-
Hepatocellular carcinoma
- MIRD:
-
Medical Internal Radiation Dose
- TACE:
-
Transarterial chemoembolization
- TARE:
-
Transarterial radioembolization
- Tc-99m MAA:
-
Technetium 99m macroaggregated albumin
- Y-90:
-
Yttrium-90
References
Benson AB 3rd, D’Angelica MI, Abbott DE et al (2017) NCCN guidelines insights: hepatobiliary cancers, version 1.2017. J Natl Compr Canc Netw 15(5):563–573
Salem R, Padia SA, Lam M et al (2019 Jul) Clinical and dosimetric considerations for Y90: recommendations from an international multidisciplinary working group. Eur J Nucl Med Mol Imaging 46(8):1695–1704
SIR-Spheres® Y-90 resin microspheres. Package Insert [Internet]. [cited 2018 Jan 23]. Available from: https://www.sirtex.com/media/155126/ssl-us-13.pdf
Giammarile F, Bodei L, Chiesa C et al (2011) EANM procedure guideline for the treatment of liver cancer and liver metastases with intra-arterial radioactive compounds. Eur J Nucl Med Mol Imaging 38(7):1393–1406
Garin E (2015) Radioembolization with 90 Y-loaded microspheres: high clinical impact of treatment simulation with MAA-based dosimetry. Eur J Nucl Med Mol Imaging 42(8):1189–1191
Lassmann M, Chiesa C, Flux G, Bardiès M (2011) EANM Dosimetry Committee guidance document: good practice of clinical dosimetry reporting. Eur J Nucl Med Mol Imaging 38(1):192–200
Srinivas SM, Nasr EC, Kunam VK, Bullen JA, Purysko AS (2016) Administered activity and outcomes of glass versus resin 90Y microsphere radioembolization in patients with colorectal liver metastases. J Gastrointest Oncol 7(4):530–539
AbdelRazek M, Khalaf M, Abdelmaksoud M et al (2018) 3:27 PM Abstract No. 124 MIRD-based activity calculation may improve outcomes over body surface area for resin microsphere radioembolization of metastatic colorectal carcinoma. J Vasc Interv Radiol 29(4):S56
Shah JL, Zendejas-Ruiz IR, Thornton LM et al (2017) Neoadjuvant transarterial radiation lobectomy for colorectal hepatic metastases: a small cohort analysis on safety, efficacy, and radiopathologic correlation. J Gastrointest Oncol 8(3):E43–E51
Vouche M, Habib A, Ward TJ et al (2014) Unresectable solitary hepatocellular carcinoma not amenable to radiofrequency ablation: multicenter radiology-pathology correlation and survival of radiation segmentectomy. Hepatology. 60(1):192–201
Kallini JR, Gabr A, Thorlund K et al (2017) Comparison of the adverse event profile of TheraSphere® with SIR-spheres® for the treatment of unresectable hepatocellular carcinoma: a systematic review. Cardiovasc Intervent Radiol 40(7):1033–1043
Borggreve AS, Landman AJEMC, Vissers CMJ et al (2016) Radioembolization: is prophylactic embolization of hepaticoenteric arteries necessary? A systematic review. Cardiovasc Intervent Radiol 39(5)
Common Terminology Criteria for Adverse Events (CTCAE). 2017;155
Ward TJ, Louie JD, Sze DY (2017) Yttrium-90 radioembolization with resin microspheres without routine embolization of the gastroduodenal artery. J Vasc Interv Radiol 28(2):246–253
Wright CL, Werner JD, Tran JM et al (2012) Radiation pneumonitis following yttrium-90 radioembolization: case report and literature review. J Vasc Interv Radiol 23(5):669–674
Dobrocky T, Fuerstner M, Klaeser B, Lopez-Benitez R, Wälti YB, Kara L (2015) Regional radiation pneumonitis after SIRT of a subcapsular liver metastasis: what is the effect of direct beta irradiation? Cardiovasc Intervent Radiol 38(4):1025–1030
Ward TJ, Tamrazi A, Lam MGEH et al (2015) Management of High hepatopulmonary shunting in patients undergoing hepatic radioembolization. J Vasc Interv Radiol 26(12):1751–1760
Edeline J, Touchefeu Y, Guiu B et al (2019) Radioembolization plus chemotherapy for first-line treatment of locally advanced intrahepatic cholangiocarcinoma: a phase 2 clinical trial. JAMA Oncol 6(1):51–59
Chow PKH, Gandhi M, Tan S-B et al (2018) SIRveNIB: selective internal radiation therapy versus sorafenib in Asia-Pacific patients with hepatocellular carcinoma. J Clin Oncol 2:JCO2017760892
Vilgrain V, Pereira H, Assenat E et al (2017) Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): an open-label randomised controlled phase 3 trial. Lancet Oncol 18(12):1624–1636
Wasan HS, Gibbs P, Sharma NK et al (2017) First-line selective internal radiotherapy plus chemotherapy versus chemotherapy alone in patients with liver metastases from colorectal cancer (FOXFIRE, SIRFLOX, and FOXFIRE-Global): a combined analysis of three multicentre, randomised, phase 3 trials. Lancet Oncol 18(9):1159–1171
Yang H, Seon J, Sung PS et al (2017) Dexamethasone prophylaxis to alleviate postembolization syndrome after transarterial chemoembolization for hepatocellular carcinoma: a randomized, double-blinded, placebo-controlled study. J Vasc Interv Radiol 28(11):1503–1511.e2
Acknowledgments
This study was funded by Sirtex Medical Inc.
Funding
This study was funded by Sirtex Medical Inc. Woburn MA. The funding supported research personnel performing data collection and data analysis for this project. The funding source had no role in the design of the study and no personnel from the funding source had involvement in data collection, analysis, interpretation of the data, or writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ammar Sarwar (Author).
Conflict of interest
Ammar Sarwar (Author) has received research grants from Sirtex Medical Inc. and is a consultant for the company. None of the other authors have a conflict of interest relevant to this publication.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sarwar, A., Kudla, A., Weinstein, J.L. et al. Yttrium-90 radioembolization using MIRD dosimetry with resin microspheres. Eur Radiol 31, 1316–1324 (2021). https://doi.org/10.1007/s00330-020-07231-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07231-8