Abstract
Objectives
The purpose of this study was to determine the efficacy and safety of contrast-enhanced ultrasound (CEUS)–guided celiac plexus neurolysis (CPN) in patients with upper abdominal cancer pain.
Methods
Thirty-five patients with upper abdominal cancers tortured by intractable upper abdominal pain underwent CEUS-guided CPN with ethanol. The pain alleviation and opioid intake were observed and evaluated during a 3-month follow-up after CPN. The dispersion of alcohol around the aorta was evaluated on 3D-CEUS. Complications were assessed during CPN and at follow-up.
Results
All of the 35 patients’ CPN was successfully achieved. Pain relief was observed in 28 (80%), 20 (57.1%), 27 (77.1%), 20 (57.1%), and 10 (29.4%) patients immediately, 1 day, 1 month, 2 months, and 3 months after CPN, respectively. The agent dispersion around the aorta on CEUS images of 28 patients who showed pain relief was at least 90° of the circumference around the aorta. The median duration of pain alleviation was 2.7 months (95% confidence interval [CI], 2.5–2.9). Less than half of the patients had minor complications including irritant pain at the puncture site (8 of 35; 22.9%), diarrhea (4 of 35; 11.4%), nausea and vomiting (3 of 35; 8.6%), and post-procedural hypotension (1 of 35; 2.9%).
Conclusions
CEUS-guided CPN is a safe and effective method to alleviate refractory upper abdominal pain in patients with upper abdominal cancers. CEUS image allows the visualization of puncture path and observation of drug dispersion. The pain relief is relevant to the dispersion of neurolytic agent around the aorta.
Key Points
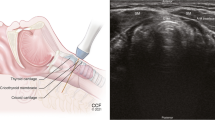
• CEUS-guided celiac plexus neurolysis (CPN) is feasible and easy.
• It allows direct visualization of the diffusion of the neurolytic agent in the retroperitoneal anatomic space.
• CEUS-guided CPN improves safety of CPN by clearly delineating the needle path.






Similar content being viewed by others
Abbreviations
- 2D:
-
Two dimensional
- 3D:
-
Three dimensional
- CEUS:
-
Contrast-enhanced ultrasound
- CPN:
-
Celiac plexus neurolysis
- CT:
-
Computed tomography
- EUS:
-
Endoscopic ultrasound
- iv:
-
Intravenous access
- MI:
-
Mechanical index
- MR:
-
Magnetic resonance
- ROI:
-
Region of interest
- US:
-
Ultrasound/ultrasonography
- VAS:
-
Visual analog scales
References
Cornman-Homonoff J, Holzwanger D, Lee K et al (2017) Celiac plexus block and neurolysis in the management of chronic upper abdominal pain[J]. Semin Interv Radiol 34(04):376–386
Scarborough BM, Smith CB (2018) Optimal pain management for patients with cancer in the modern era[J]. CA Cancer J Clin 68(suppl 2) 68(3):182–196
Wong GY, Schroeder DR, Carns PE et al (2004) Effect of neurolytic celiac plexus block on pain relief, quality of life, and survival in patients with unresectable pancreatic cancer: a randomized controlled trial[J]. Jama 291(9):1092–1099
Amr YM, Makharita MY (2014) Neurolytic sympathectomy in the management of cancer pain—time effect: a prospective, randomized multicenter study[J]. J Pain Symptom Manage 48(5):944–956.e2
Arcidiacono PG, Rossi M (2004) Celiac plexus neurolysis[J]. JOP: J Pancreas 5(4):315–321
Kambadakone A, Thabet A, Gervais DA et al (2011) CT-guided celiac plexus neurolysis: a review of anatomy, indications, technique, and tips for successful treatment[J]. Radiographics 31(6):1599–1621
Tempero MA, Malafa MP, Al-Hawary M et al (2017) Pancreatic adenocarcinoma, version 2.2017: clinical practice guidelines in Oncology[J]. J Natl Compr Canc Netw 15(8):1028–1061
Yasuda I, Wang HP (2017) Endoscopic ultrasound-guided celiac plexus block and neurolysis[J]. Dig Endosc 29(4):455–462
Seicean A (2014) Celiac plexus neurolysis in pancreatic cancer: the endoscopic ultrasound approach[J]. World J Gastroenterol 01:124–131
Gress F (2001) Endoscopic ultrasound-guided celiac plexus block for managing abdominal pain associated with chronic pancreatitis: a prospective single center experience[J]. Am J Gastroenterol 96(2):409–416
Obstein KL, Martins FP, Fernández-Esparrach G et al (2010) Endoscopic ultrasound-guided celiac plexus neurolysis using a reverse phase polymer[J]. World J Gastroenterol 16(6):728–731
Wang PJ, Shang MY, Qian Z et al (2006) CT-guided percutaneous neurolytic celiac plexus block technique[J]. Abdom Imaging 31(6):710–718
Bhatnagar S, Joshi S, Rana SPS et al (2014) Bedside ultrasound-guided celiac plexus neurolysis in upper abdominal cancer patients: a randomized, prospective study for comparison of percutaneous bilateral paramedian vs. unilateral paramedian needle-insertion technique[J]. Pain Pract 14(2):E63–E68
Huang DY, Yusuf GT, Daneshi M et al (2018) Contrast-enhanced ultrasound (CEUS) in abdominal intervention[J]. Abdom Radiol 43(4):960–976
Huang DY, Yusuf GT, Daneshi M et al (2016) Contrast-enhanced US-guided interventions: improving success rate and avoiding complications using US contrast agents[J]. Radiographics 37(2):160123
Luyao Z, Xiaoyan X, Huixiong X et al (2012) Percutaneous ultrasound-guided cholangiography using microbubbles to evaluate the dilated biliary tract: initial experience[J]. Eur Radiol 22(2):371–378
Exacoustos C, Zupi E, Szabolcs B et al (2009) Contrast-tuned imaging and second-generation contrast agent SonoVue: a new ultrasound approach to evaluation of tubal patency[J]. J Minim Invasive Gynecol 16(4):437–444
Cheng XQ, Zhang ZQ, Guo XY et al (2017) Adhesive capsulitis of the shoulder: evaluation with US-arthrography using a sonographic contrast agent[J]. Sci Rep 7(1):7–17
Cheng XQ, Lu M, Yang X et al (2015) The effect of percutaneous ultrasound-guided subacromial bursography using microbubbles in the assessment of subacromial impingement syndrome: initial experience[J]. Eur Radiol 25(8):2412–2418
Maruyama, Hitoshi, Kamezaki et al (2013) The application of transabdominal 3D ultrasound for the diagnosis of gastric varices: a preliminary study[J]. Eur J Radiol 82(9):E400–E404
Wong P, Muanza T, Reynard E et al (2011) Use of 3D-ultrasound in the detection of breast tumor bed displacement during radiotherapy[J]. Int J Radiat Oncol Biol Phys 75(3):S196–S197
Moiyadi AV, Shetty P (2016) Direct navigated 3D ultrasound for resection of brain tumors: a useful tool for intraoperative image guidance[J]. Neurosurg Focus 40(3):E5
Bartolotta TV, Taibbi A, Matranga D et al (2015) 3D versus 2D contrast-enhanced sonography in the evaluation of therapeutic response of hepatocellular carcinoma after locoregional therapies: preliminary findings[J]. Radiol Med 120(8):695–704
Arlt F, Chalopin C, Müns A et al (2016) Intraoperative 3D contrast-enhanced ultrasound (CEUS): a prospective study of 50 patients with brain tumours[J]. Acta Neurochir 158(4):685–694
Kiyokawa K, Masuda H, Fuyuki T et al (2000) Three-dimensional hysterosalpingo-contrast sonography (3D-HyCoSy) as an outpatient procedure to assess infertile women: a pilot study[J]. Ultrasound Obstet Gynecol 16(7):648–654
Song ZZ (2008) Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma[J]. Hepatology 47(6):2145–2146
Hawker GA, Mian S, Kendzerska T et al (2011) Measures of adult pain: visual analog scale for pain (VAS pain), Numeric Rating Scale for pain (NRS pain), McGill Pain Questionnaire (MPQ), short-form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), short form-36 bodily pain scale (SF)[J]. Arthritis Care Res 63(S11):S240–S252
Cohen SP, Christo PJ, Wang S et al (2008) The effect of opioid dose and treatment duration on the perception of a painful standardized clinical stimulus[J]. Reg Anesth Pain Med 33(3):199–206
Cardella JF, Kundu S, Miller DL et al (2009) Society of Interventional Radiology Clinical Practice Guidelines[J]. J Vasc Interv Radiol 20(7):S189–S191
Liu S, Fu W, Liu Z et al (2016) MRI-guided celiac plexus neurolysis for pancreatic cancer pain: efficacy and safety[J]. J Magn Reson Imaging 44(4):923–928
Lou S (2019) Endoscopic ultrasound-guided celiac plexus neurolysis to alleviate intractable pain caused by advanced pancreatic cancer. Surg Laparosc Endosc Percutan Tech 29(6):472–475
Edelstein MR, Gabriel RT et al (2017) Pain outcomes in patients undergoing CT-guided celiac plexus neurolysis for intractable abdominal visceral pain. Am J Hosp Palliat Med 34(2):111–114
Iwata K, Yasuda I, Enya M et al (2011) Predictive factors for pain relief after endoscopic ultrasound-guided celiac plexus neurolysis[J]. Dig Endosc 23(2):140–145
Lee JM (2000) CT-guided celiac plexus block for intractable abdominal pain[J]. J Korean Med Sci 15(2):173–178
Mohamed RE, Amin MA, Omar HM (2017) Computed tomography-guided celiac plexus neurolysis for intractable pain of unresectable pancreatic cancer[J]. Egypt J Radiol Nucl Med 48(3):627–637
Ishiwatari H, Hayashi T, Yoshida M et al (2015) EUS-guided celiac plexus neurolysis by using highly viscous phenol-glycerol as a neurolytic agent (with video)[J]. Gastrointest Endosc 81(2):479–483
Sakamoto H, Kitano M (2010) Kamata K, et al EUS-guided broad plexus neurolysis over the superior mesenteric artery using a 25-gauge needle[J]. Am J Gastroenterol 105(12):2599–2606
Xu HX, Lu MD, Xie XH et al (2008) Three-dimensional contrast-enhanced ultrasound of the liver: experience of 92 cases[J]. Ultrasonics 49(3):377–385
Arif M, Moelker A, Vanwalsum TW (2018) Needle tip visibility in 3D ultrasound images[J]. Cardiovasc Intervent Radiol 41(1):145–152
Sushma, Bhatnagar, Sanjay et al (2017) Evaluation of outcomes of ultrasound guided celiac plexus neurolysis using immediate post procedure computed tomography: an observational study.[J]. Indian J Gastroenterol 2017(Suppl 11):282–288
Funding
This study has received funding from the Sichuan Province Science and Technology Support Program (grant number SCCHEC-03-2018-002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Man Lu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Prospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lu Wang and Man Lu are co-first authors.
Rights and permissions
About this article
Cite this article
Wang, L., Lu, M., Wu, X. et al. Contrast-enhanced ultrasound–guided celiac plexus neurolysis in patients with upper abdominal cancer pain: initial experience. Eur Radiol 30, 4514–4523 (2020). https://doi.org/10.1007/s00330-020-06705-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06705-z