Abstract
Objective
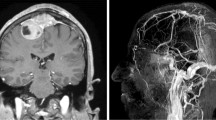
Meningiomas are highly vascularized tumors which may recruit pial blood supply. Pial supply complicates tumor treatment in numerous ways. The objective of this study was to establish a reliable MRI-based diagnostic score to predict the existence of pial blood supply in supratentorial intracranial meningiomas and then correlate the score with clinical and surgical outcomes and histopathological findings.
Methods
We performed a retrospective analysis of supratentorial histologically proven meningiomas in our institution from 2010 to 2018. A score was built based on MRI criteria and correlated with digital subtraction angiography (DSA) pial vascularization assessment. The score was then validated on a second independent population recruited with the same modalities.
Results
Logistic regression identified four parameters related to pial blood supply which were used to build the score: skull base location, tumor size > 45 mm, peritumoral flow voids, and incomplete cerebrospinal fluid rim. The overall diagnostic performance in predicting pial blood supply was as follows: sensitivity 97.8%, specificity 76.9%, predictive positive value 88.2%, negative predictive value 95.2%, and accuracy 90.3%. Inter-reader agreement and Cohen’s kappa were good, respectively, of 90.7% and 0.69. A high score was associated with aggressive meningioma (World Health Organization II–III) (p = 0.04) and with greater importance of pial supply relative to dural supply.
Conclusions
We have identified a reliable way to use MRI to predict the existence of pial blood supply in supratentorial intracranial meningiomas. A higher score also predicted higher grade meningioma.
Key Points
• Accurate and reproducible MRI score composed of four items to predict the existence of pial blood supply in supratentorial meningioma.
• High score is associated with high-grade meningioma (WHO II–III) but also with greater importance of pial supply relative to dural supply.



Similar content being viewed by others
Abbreviations
- DSA:
-
Digital subtraction angiography
- ECA:
-
External carotid artery
- PTBE:
-
Peritumoral brain edema
- WHO:
-
World Health Organization
References
Shah A, Choudhri O, Jung H, Li G (2015) Preoperative endovascular embolization of meningiomas: update on therapeutic options. Neurosurg Focus 38:E7. https://doi.org/10.3171/2014.12.FOCUS14728
Dubel GJ, Ahn SH, Soares GM (2013) Contemporary endovascular embolotherapy for meningioma. Semin Intervent Radiol 30:263–277. https://doi.org/10.1055/s-0033-1353479
Aihara M, Naito I, Shimizu T et al (2015) Preoperative embolization of intracranial meningiomas using n-butyl cyanoacrylate. Neuroradiology 57:713–719. https://doi.org/10.1007/s00234-015-1521-9
Takeguchi T, Miki H, Shimizu T et al (2003) Prediction of tumor-brain adhesion in intracranial meningiomas by MR imaging and DSA. Magn Reson Med Sci 2:171–179
Alvernia JE, Sindou MP (2004) Preoperative neuroimaging findings as a predictor of the surgical plane of cleavage: prospective study of 100 consecutive cases of intracranial meningioma. J Neurosurg 100:422–430. https://doi.org/10.3171/jns.2004.100.3.0422
Ildan F, Erman T, Göçer AI et al (2007) Predicting the probability of meningioma recurrence in the preoperative and early postoperative period: a multivariate analysis in the midterm follow-up. Skull Base 17:157–171. https://doi.org/10.1055/s-2007-970554
Nowak A, Dziedzic T, Krych P et al (2015) Benign versus atypical meningiomas: risk factors predicting recurrence. Neurol Neurochir Pol 49:1–10. https://doi.org/10.1016/j.pjnns.2014.11.003
Pistolesi S, Fontanini G, Camacci T et al (2002) Meningioma-associated brain oedema: the role of angiogenic factors and pial blood supply. J Neurooncol 60:159–164
Nakasu S, Fukami T, Jito J, Matsuda M (2005) Microscopic anatomy of the brain-meningioma interface. Brain Tumor Pathol 22:53–57. https://doi.org/10.1007/s10014-005-0187-0
Bitzer M, Wöckel L, Luft AR et al (1997) The importance of pial blood supply to the development of peritumoral brain edema in meningiomas. J Neurosurg 87:368–373. https://doi.org/10.3171/jns.1997.87.3.0368
Sindou MP, Alaywan M (1998) Most intracranial meningiomas are not cleavable tumors: anatomic-surgical evidence and angiographic predictibility. Neurosurgery 42:476–480
Sato M, Nakai Y, Tsurushima H, Shiigai M, Masumoto T, Matsumura A (2013) Risk factors of ischemic lesions related to cerebral angiography and neuro-interventional procedures. Neurol Med Chir (Tokyo) 53:381–387
Enokizono M, Morikawa M, Matsuo T et al (2014) The rim pattern of meningioma on 3D FLAIR imaging: correlation with tumor-brain adhesion and histological grading. Magn Reson Med Sci 13:251–260. https://doi.org/10.2463/mrms.2013-0132
Tsutsumi S, Izumi H, Yasumoto Y, Ito M (2013) Convexity en plaque meningioma manifesting as subcutaneous mass: case report. Neurol Med Chir (Tokyo) 53:727–729. https://doi.org/10.2176/nmc.cr2012-0324
Lagman C, Ong V, Nguyen T et al (2018) The Meningioma Vascularity Index: a volumetric analysis of flow voids to predict intraoperative blood loss in nonembolized meningiomas. J Neurosurg 1–6. https://doi.org/10.3171/2018.1.JNS172724
El Sanharawi M, Naudet F (2013) Understanding logistic regression. J Fr Ophtalmol 36:710–715. https://doi.org/10.1016/j.jfo.2013.05.008
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Aymeric Rouchaud.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Diagnostic or prognostic study/observational
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 23 kb)
Rights and permissions
About this article
Cite this article
Friconnet, G., Espíndola Ala, V.H., Janot, K. et al. MRI predictive score of pial vascularization of supratentorial intracranial meningioma. Eur Radiol 29, 3516–3522 (2019). https://doi.org/10.1007/s00330-019-06197-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06197-6