Abstract
Objectives
Invasive treatment of tumors adjacent to large hepatic vessels is a continuous clinical challenge. The primary aim of this study was to examine the feasibility of ablating liver tissue adjacent to large hepatic and portal veins with magnetic resonance imaging–guided high-intensity focused ultrasound (MRgHIFU). The secondary aim was to compare sonication data for ablations performed adjacent to hepatic veins (HV) versus portal veins (PV).
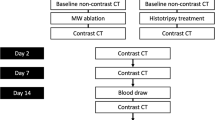
Materials and methods
MRgHIFU ablations were performed in six male land swine under general anesthesia. Ablation cells of either 4 or 8 mm diameter were planned in clusters (two/animal) adjacent either to HV (n = 6) or to PV (n = 6), with diameter ≥ 5 mm. Ablations were made using 200 W and 1.2 MHz. Post-procedure evaluation was made on contrast-enhanced MRI (T1w CE-MRI), histopathology, and ablation data from the HIFU system.
Results
A total of 153 ablations in 81 cells and 12 clusters were performed. There were visible lesions with non-perfused volumes in all animals on T1w CE-MRI images. Histopathology showed hemorrhage and necrosis in all 12 clusters, with a median shortest distance to vessel wall of 0.4 mm (range 0–2.7 mm). Edema and endothelial swelling were observed without vessel wall rupture. In 8-mm ablations (n = 125), heat sink was detected more often for HV (43%) than for PV (19%; p = 0.04).
Conclusions
Ablations yielding coagulative necrosis of liver tissue can be performed adjacent to large hepatic vessels while keeping the vessel walls intact. This indicates that perivascular tumor ablation in the liver is feasible using MRgHIFU.
Key Points
• High-intensity focused ultrasound ablation is a non-invasive treatment modality that can be used for treatment of liver tumors.
• This study shows that ablations of liver tissue can be performed adjacent to large hepatic vessels in an experimental setting.
• Liver tumors close to large vessels can potentially be treated using this modality.




Similar content being viewed by others
Abbreviations
- BW:
-
Bandwidth
- CEUS:
-
Contrast-enhanced ultrasound
- DT:
-
Dynamic scan time
- EM:
-
Equivalent minutes
- FA:
-
Flip angle
- FFE:
-
Fast field echo
- GRE-EPI:
-
Gradient echo sequence with echo-planar readout
- HCC:
-
Hepatocellular carcinoma
- HIFU:
-
High-intensity focused ultrasound
- MRgHIFU:
-
Magnetic resonance imaging–guided high-intensity focused ultrasound
- NPV:
-
Non-perfused volume
- PFS:
-
Proton frequency shift
- PS:
-
Pixel sum
- SENSE:
-
Sensitivity encoding
- SpO2%:
-
Oxygen saturation
- T1w:
-
T1 weighted
- T2w:
-
T2 weighted
- TE:
-
Echo time
- TFE:
-
Turbo field echo
- TR:
-
Repetition time
- USgHIFU:
-
Ultrasound-guided high-intensity focused ultrasound
- VS:
-
Voxel size
References
Frankel TL, D'Angelica MI (2014) Hepatic resection for colorectal metastases. J Surg Oncol 109:2–7
European Association For The Study Of The Liver; European Organisation For Research And Treatment Of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56:908–943
Van Cutsem E, Cervantes A, Nordlinger B, Arnold D, ESMO Guidelines Working Group (2014) Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 25(Suppl 3):iii1–iii9
Xiao Y, Li W, Wan H, Tan Y, Wu H (2018) Central hepatectomy versus major hepatectomy for patients with centrally located hepatocellular carcinoma: a meta-analysis. Int J Surg 52:297–302
Yu WB, Rao A, Vu V, Xu L, Rao JY, Wu JX (2017) Management of centrally located hepatocellular carcinoma: update 2016. World J Hepatol 9:627–634
Azoulay D, Pascal G, Salloum C, Adam R, Castaing D, Tranecol N (2013) Vascular reconstruction combined with liver resection for malignant tumours. Br J Surg 100:1764–1775
Abitabile P, Hartl U, Lange J, Maurer CA (2007) Radiofrequency ablation permits an effective treatment for colorectal liver metastasis. Eur J Surg Oncol 33:67–71
Martin RC, Scoggins CR, McMasters KM (2010) Safety and efficacy of microwave ablation of hepatic tumors: a prospective review of a 5-year experience. Ann Surg Oncol 17:171–178
Lu DS, Raman SS, Limanond P et al (2003) Influence of large peritumoral vessels on outcome of radiofrequency ablation of liver tumors. J Vasc Interv Radiol 14:1267–1274
Lu DS, Raman SS, Vodopich DJ, Wang M, Sayre J, Lassman C (2002) Effect of vessel size on creation of hepatic radiofrequency lesions in pigs: assessment of the “heat sink” effect. AJR Am J Roentgenol 178:47–51
Courivaud F, Kazaryan AM, Lund A et al (2014) Thermal fixation of swine liver tissue after magnetic resonance-guided high-intensity focused ultrasound ablation. Ultrasound Med Biol 40:1564–1577
Kim YS, Rhim H, Choi MJ, Lim HK, Choi D (2008) High-intensity focused ultrasound therapy: an overview for radiologists. Korean J Radiol 9:291–302
Holland GA, Mironov O, Aubry J-F, Hananel A, Duda JB (2013) High-intensity focused ultrasound. Ultrasound Clinics 8:213–226
Li S, Wu PH (2013) Magnetic resonance image-guided versus ultrasound-guided high-intensity focused ultrasound in the treatment of breast cancer. Chin J Cancer 32:441–452
de Senneville BD, Mougenot C, Quesson B, Dragonu I, Grenier N, Moonen CT (2007) MR thermometry for monitoring tumor ablation. Eur Radiol 17:2401–2410
Zhang L, Zhu H, Jin C et al (2009) High-intensity focused ultrasound (HIFU): effective and safe therapy for hepatocellular carcinoma adjacent to major hepatic veins. Eur Radiol 19:437–445
Jiang F, He M, Liu YJ, Wang ZB, Zhang L, Bai J (2013) High intensity focused ultrasound ablation of goat liver in vivo: pathologic changes of portal vein and the “heat-sink” effect. Ultrasonics 53:77–83
Kopelman D, Inbar Y, Hanannel A et al (2006) Magnetic resonance-guided focused ultrasound surgery (MRgFUS): ablation of liver tissue in a porcine model. Eur J Radiol 59:157–162
Sapareto SA, Dewey WC (1984) Thermal dose determination in cancer therapy. Int J Radiat Oncol Biol Phys 10:787–800
Chiang J, Willey BJ, Del Rio AM, Hinshaw JL, Lee FT, Brace CL (2014) Predictors of thrombosis in hepatic vasculature during microwave tumor ablation of an in vivo porcine model. J Vasc Interv Radiol 25:1965–1971 e1962
Chiang J, Cristescu M, Lee MH et al (2016) Effects of microwave ablation on arterial and venous vasculature after treatment of hepatocellular carcinoma. Radiology 281:617–624
Ishii T, Numata K, Hao Y et al (2017) Evaluation of hepatocellular carcinoma tumor vascularity using contrast-enhanced ultrasonography as a predictor for local recurrence following radiofrequency ablation. Eur J Radiol 89:234–241
Wijlemans JW, de Greef M, Schubert G et al (2015) A clinically feasible treatment protocol for magnetic resonance-guided high-intensity focused ultrasound ablation in the liver. Invest Radiol 50:24–31
Ramaekers P, de Greef M, van Breugel JM, Moonen CT, Ries M (2016) Increasing the HIFU ablation rate through an MRI-guided sonication strategy using shock waves: feasibility in the in vivo porcine liver. Phys Med Biol 61:1057–1077
Zhao LY, Liu S, Chen ZG, Zou JZ, Wu F (2016) Cavitation enhances coagulated size during pulsed high-intensity focussed ultrasound ablation in an isolated liver perfusion system. Int J Hyperthermia. https://doi.org/10.1080/02656736.2016.1255918:1-11
Ringe KI, Lutat C, Rieder C, Schenk A, Wacker F, Raatschen HJ (2015) Experimental evaluation of the heat sink effect in hepatic microwave ablation. PLoS One 10:e0134301
Chiang J, Hynes K, Brace CL (2012) Flow-dependent vascular heat transfer during microwave thermal ablation. Conf Proc IEEE Eng Med Biol Soc 2012:5582–5585
Wachsberg RH, Angyal EA, Klein KM, Kuo HR, Lambert WC (1997) Echogenicity of hepatic versus portal vein walls revisited with histologic correlation. J Ultrasound Med 16:807–810 quiz 811-802
Bangard C, Gossmann A, Kasper HU et al (2006) Experimental radiofrequency ablation near the portal and the hepatic veins in pigs: differences in efficacy of a monopolar ablation system. J Surg Res 135:113–119
Frericks BB, Ritz JP, Albrecht T et al (2008) Influence of intrahepatic vessels on volume and shape of percutaneous thermal ablation zones: in vivo evaluation in a porcine model. Invest Radiol 43:211–218
Funding
This study has received funding by The Norwegian Cancer Society (Kreftforeningen).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Per Kristian Hol Prof. M.D., The Intervention Center, Oslo University Hospital and Institute of Clinical Medicine, University of Oslo.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Manuela Zucknick, Oslo Centre for Biostatistics and Epidemiology, Faculty of Medicine, Oslo University, kindly provided statistical advice for this manuscript.
Ethical approval
Approval from the Institutional Animal Care Committee was obtained.
Methodology
• experimental
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Carling, U., Barkhatov, L., Reims, H.M. et al. Can we ablate liver lesions close to large portal and hepatic veins with MR-guided HIFU? An experimental study in a porcine model. Eur Radiol 29, 5013–5021 (2019). https://doi.org/10.1007/s00330-018-5996-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5996-8