Abstract
Purpose
To assess the diagnostic value of multiparametric magnetic resonance imaging (MRI) including dynamic Gd-EOB-DTPA-enhanced (DCE) and diffusion-weighted (DW) imaging for diagnosis and staging of hepatic fibrosis in primary sclerosing cholangitis (PSC) using transient elastography as a standard reference.
Material and methods
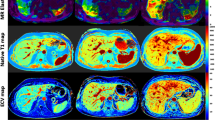
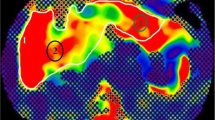
Multiparametric MRI was prospectively performed on a 3.0-Tesla scanner in 47 patients (age 43.9±14.3 years). Transient elastography derived liver stiffness measurements (LSM), DCE-MRI derived parameters (hepatocellular uptake rate (Ki), arterial (Fa), portal venous (Fv) and total (Ft) blood flow, mean transit time (MTT), and extracellular volume (Ve)) and the apparent diffusion coefficient (ADC) were calculated. Correlation and univariate analysis of variance with post hoc pairwise comparison were applied to test for differences between LSM derived fibrosis stages (F0/F1, F2/3, F4). ROC curve analysis was used as a performance measure.
Results
Both ADC and Ki correlated significantly with LSM (r= -0.614; p<0.001 and r= -0.368; p=0.01). The ADC significantly discriminated fibrosis stages F0/1 from F2/3 and F4 (p<0.001). Discrimination of F0/1 from F2/3 and F4 reached a sensitivity/specificity of 0.917/0.821 and 0.8/0.929, respectively. Despite significant inter-subject effect for classification of fibrosis stages, post hoc pairwise comparison was not significant for Ki (p>0.096 for F0/1 from F2/3 and F4). LSM, ADC and Ki were significantly associated with serum-based liver functional tests, disease duration and spleen volume.
Conclusion
DW-MRI provides a higher diagnostic performance for detection of hepatic fibrosis and cirrhosis in PSC patients in comparison to Gd-EOB-DTPA-enhanced DCE-MRI.
Key Points
• Both ADC and hepatocellular uptake rate (Ki) correlate significantly with liver stiffness (r= -0.614; p<0.001 and r= -0.368; p=0.01).
• The DCE-imaging derived quantitative parameter hepatocellular uptake rate (Ki) fails to discriminate pairwise intergroup differences of hepatic fibrosis (p>0.09).
• DWI is preferable to DCE-imaging for discrimination of fibrosis stages F0/1 to F2/3 (p<0.001) and F4 (p<0.001).






Similar content being viewed by others
Abbreviations
- ADC :
-
Apparent diffusion coefficient
- ALT:
-
Alanine amino transferase
- AP:
-
Alkaline phosphatase
- AST:
-
Aspartate amino transferase
- DCE :
-
Dynamic contrast-enhanced
- DWI :
-
Diffusion-weighted imaging
- EASL:
-
European Association for the Study of the Liver
- Fa:
-
Arterial flow
- Fi:
-
Hepatic uptake fraction
- FOV:
-
Field-of-view
- Fv:
-
Portal venous flow
- Gd-EOB-DTPA:
-
Gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid
- GFR:
-
Glomerular filtration rate
- GGT:
-
Gamma-glutamyl-transferase
- IgG:
-
Immunoglobulin G
- Ki :
-
Hepatocellular uptake rate
- LSM:
-
Liver stiffness measurements
- METAVIR :
-
Meta-analysis of histological data in viral hepatitis
- MRI :
-
Magnetic resonance imaging
- MTT:
-
Mean transit time
- NEX:
-
Number of excitations
- PSC :
-
Primary sclerosing cholangitis
- ROC :
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- SPIR:
-
Spectral inversion recovery
- TE:
-
Echo time
- TR:
-
Repetition time
- TSE:
-
Turbo spin echo
- Ve:
-
Extracellular volume
References
Portmann B, Zen Y (2012) Inflammatory disease of the bile ducts-cholangiopathies: liver biopsy challenge and clinicopathological correlation. Histopathology 60:236–248
Kovac JD, Weber MA (2016) Primary Biliary Cirrhosis and Primary Sclerosing Cholangitis: an Update on MR Imaging Findings with Recent Developments. J Gastrointestin Liver Dis 25:517–524
Ziol M, Handra-Luca A, Kettaneh A et al (2005) Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Hepatology 41:48–54
Castera L, Vergniol J, Foucher J et al (2005) Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology 128:343–350
Foucher J, Chanteloup E, Vergniol J et al (2006) Diagnosis of cirrhosis by transient elastography (FibroScan): a prospective study. Gut 55:403–408
Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24:289–293
Corpechot C, Gaouar F, El Naggar A et al (2014) Baseline values and changes in liver stiffness measured by transient elastography are associated with severity of fibrosis and outcomes of patients with primary sclerosing cholangitis. Gastroenterology 146:970–979 quiz e915-976
Ehlken H, Wroblewski R, Corpechot C et al (2016) Validation of Transient Elastography and Comparison with Spleen Length Measurement for Staging of Fibrosis and Clinical Prognosis in Primary Sclerosing Cholangitis. PLoS One 11:e0164224
Taouli B, Tolia AJ, Losada M et al (2007) Diffusion-weighted MRI for quantification of liver fibrosis: preliminary experience. AJR Am J Roentgenol 189:799–806
Taouli B, Chouli M, Martin AJ, Qayyum A, Coakley FV, Vilgrain V (2008) Chronic hepatitis: role of diffusion-weighted imaging and diffusion tensor imaging for the diagnosis of liver fibrosis and inflammation. J Magn Reson Imaging 28:89–95
Lewin M, Poujol-Robert A, Boelle PY et al (2007) Diffusion-weighted magnetic resonance imaging for the assessment of fibrosis in chronic hepatitis C. Hepatology 46:658–665
Faria SC, Ganesan K, Mwangi I et al (2009) MR imaging of liver fibrosis: current state of the art. Radiographics 29:1615–1635
Li Z, Sun J, Chen L et al (2016) Assessment of liver fibrosis using pharmacokinetic parameters of dynamic contrast-enhanced magnetic resonance imaging. J Magn Reson Imaging 44:98–104
Patel J, Sigmund EE, Rusinek H, Oei M, Babb JS, Taouli B (2010) Diagnosis of cirrhosis with intravoxel incoherent motion diffusion MRI and dynamic contrast-enhanced MRI alone and in combination: preliminary experience. J Magn Reson Imaging 31:589–600
Dyvorne HA, Jajamovich GH, Bane O et al (2016) Prospective comparison of magnetic resonance imaging to transient elastography and serum markers for liver fibrosis detection. Liver Int 36:659–666
Nilsson H, Blomqvist L, Douglas L et al (2013) Gd-EOB-DTPA-enhanced MRI for the assessment of liver function and volume in liver cirrhosis. Br J Radiol 86:20120653
Juluru K, Talal AH, Yantiss RK et al (2016) Diagnostic accuracy of intracellular uptake rates calculated using dynamic Gd-EOB-DTPA-enhanced MRI for hepatic fibrosis stage. J Magn Reson Imaging. https://doi.org/10.1002/jmri.25431
Zhang W, Kong X, Wang ZJ, Luo S, Huang W, Zhang LJ (2015) Dynamic Contrast-Enhanced Magnetic Resonance Imaging with Gd-EOB-DTPA for the Evaluation of Liver Fibrosis Induced by Carbon Tetrachloride in Rats. PLoS One 10:e0129621
Sourbron S, Sommer WH, Reiser MF, Zech CJ (2012) Combined quantification of liver perfusion and function with dynamic gadoxetic acid-enhanced MR imaging. Radiology 263:874–883
Sandrin L, Fourquet B, Hasquenoph JM et al (2003) Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol 29:1705–1713
Portney L, Watkins M (1999) Foundations of clinical research: application to practice. Prentice Hall, Upper Saddle River
Juluru K, Talal AH, Yantiss RK et al (2017) Diagnostic accuracy of intracellular uptake rates calculated using dynamic Gd-EOB-DTPA-enhanced MRI for hepatic fibrosis stage. J Magn Reson Imaging 45:1177–1185
Ning J, Yang Z, Xie S, Sun Y, Yuan C, Chen H (2017) Hepatic function imaging using dynamic Gd-EOB-DTPA enhanced MRI and pharmacokinetic modeling. Magn Reson Med 78:1488–1495
Bollow M, Taupitz M, Hamm B, Staks T, Wolf KJ, Weinmann HJ (1997) Gadolinium-ethoxybenzyl-DTPA as a hepatobiliary contrast agent for use in MR cholangiography: results of an in vivo phase-I clinical evaluation. Eur Radiol 7:126–132
Tschirch FT, Struwe A, Petrowsky H, Kakales I, Marincek B, Weishaupt D (2008) Contrast-enhanced MR cholangiography with Gd-EOB-DTPA in patients with liver cirrhosis: visualization of the biliary ducts in comparison with patients with normal liver parenchyma. Eur Radiol 18:1577–1586
Rohrer M, Bauer H, Mintorovitch J, Requardt M, Weinmann HJ (2005) Comparison of magnetic properties of MRI contrast media solutions at different magnetic field strengths. Invest Radiol 40:715–724
Hennedige TP, Wang G, Leung FP et al (2017) Magnetic Resonance Elastography and Diffusion Weighted Imaging in the Evaluation of Hepatic Fibrosis in Chronic Hepatitis B. Gut Liver 11:401–408
Feier D, Balassy C, Bastati N, Fragner R, Wrba F, Ba-Ssalamah A (2015) The diagnostic efficacy of quantitative liver MR imaging with diffusion-weighted, SWI, and hepato-specific contrast-enhanced sequences in staging liver fibrosis-a multiparametric approach. Eur Radiol. https://doi.org/10.1007/s00330-015-3830-0
Kovac JD, Dakovic M, Stanisavljevic D et al (2012) Diffusion-weighted MRI versus transient elastography in quantification of liver fibrosis in patients with chronic cholestatic liver diseases. Eur J Radiol 81:2500–2506
Wang QB, Zhu H, Liu HL, Zhang B (2012) Performance of magnetic resonance elastography and diffusion-weighted imaging for the staging of hepatic fibrosis: A meta-analysis. Hepatology 56:239–247
Wang Y, Ganger DR, Levitsky J et al (2011) Assessment of chronic hepatitis and fibrosis: comparison of MR elastography and diffusion-weighted imaging. AJR Am J Roentgenol 196:553–561
Taouli B, Koh DM (2010) Diffusion-weighted MR imaging of the liver. Radiology 254:47–66
Luciani A, Vignaud A, Cavet M et al (2008) Liver cirrhosis: intravoxel incoherent motion MR imaging--pilot study. Radiology 249:891–899
Williamson KD, Chapman RW (2015) Editorial: further evidence for the role of serum alkaline phosphatase as a useful surrogate marker of prognosis in PSC. Aliment Pharmacol Ther 41:149–151
Al Mamari S, Djordjevic J, Halliday JS, Chapman RW (2013) Improvement of serum alkaline phosphatase to <1.5 upper limit of normal predicts better outcome and reduced risk of cholangiocarcinoma in primary sclerosing cholangitis. J Hepatol 58:329–334
Ponsioen CY, Chapman RW, Chazouilleres O et al (2016) Surrogate endpoints for clinical trials in primary sclerosing cholangitis: Review and results from an International PSC Study Group consensus process. Hepatology 63:1357–1367
Ehlken H, Wroblewski R, Corpechot C et al (2016) Spleen size for the prediction of clinical outcome in patients with primary sclerosing cholangitis. Gut 65:1230–1232
European Association for the Study of the L (2009) EASL Clinical Practice Guidelines: management of cholestatic liver diseases. J Hepatol 51:237–267
Huwart L, Sempoux C, Vicaut E et al (2008) Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology 135:32–40
Lu PX, Huang H, Yuan J et al (2014) Decreases in molecular diffusion, perfusion fraction and perfusion-related diffusion in fibrotic livers: a prospective clinical intravoxel incoherent motion MR imaging study. PLoS One 9:e113846
Yoon JH, Lee JM, Baek JH et al (2014) Evaluation of hepatic fibrosis using intravoxel incoherent motion in diffusion-weighted liver MRI. J Comput Assist Tomogr 38:110–116
Haimerl M, Verloh N, Zeman F et al (2013) Assessment of clinical signs of liver cirrhosis using T1 mapping on Gd-EOB-DTPA-enhanced 3T MRI. PLoS One 8:e85658
Heye T, Yang SR, Bock M et al (2012) MR relaxometry of the liver: significant elevation of T1 relaxation time in patients with liver cirrhosis. Eur Radiol 22:1224–1232
Cassinotto C, Feldis M, Vergniol J et al (2015) MR relaxometry in chronic liver diseases: Comparison of T1 mapping, T2 mapping, and diffusion-weighted imaging for assessing cirrhosis diagnosis and severity. Eur J Radiol 84:1459–1465
Li Z, Sun J, Hu X et al (2016) Assessment of liver fibrosis by variable flip angle T1 mapping at 3.0T. J Magn Reson Imaging 43:698–703
Hinrichs H, Hinrichs JB, Gutberlet M et al (2016) Functional gadoxetate disodium-enhanced MRI in patients with primary sclerosing cholangitis (PSC). Eur Radiol 26:1116–1124
Keller S, Aigner A, Zenouzi R et al (2018) Association of gadolinium-enhanced magnetic resonance imaging with hepatic fibrosis and inflammation in primary sclerosing cholangitis. PLoS One 13:e0193929
Martin DR, Lauenstein T, Kalb B et al (2012) Liver MRI and histological correlates in chronic liver disease on multiphase gadolinium-enhanced 3D gradient echo imaging. J Magn Reson Imaging 36:422–429
Saito H, Tada S, Nakamoto N et al (2004) Efficacy of non-invasive elastometry on staging of hepatic fibrosis. Hepatol Res 29:97–103
Funding
A.W. Lohse and C. Schramm were funded by the Deutsche Forschungsgemeinschaft (DFG) (SFB841 and KFO306).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is J. Yamamura.
Conflict of interest
The authors of this manuscript declare relationships with the following companies: Philips Healthcare (H. Kooijman).
Statistics and biometry
One of the authors has significant statistical expertise (R. Buchert).
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• experimental study
• performed at one institution
Electronic supplementary material
ESM 1
(DOCX 103 kb)
Rights and permissions
About this article
Cite this article
Keller, S., Sedlacik, J., Schuler, T. et al. Prospective comparison of diffusion-weighted MRI and dynamic Gd-EOB-DTPA-enhanced MRI for detection and staging of hepatic fibrosis in primary sclerosing cholangitis. Eur Radiol 29, 818–828 (2019). https://doi.org/10.1007/s00330-018-5614-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5614-9