Abstract
Objectives
To assess patterns of parenchymal tissue on mammography in women with dense breasts and to determine how this varies with age and affects recall to assessment and cancer diagnosis.
Method
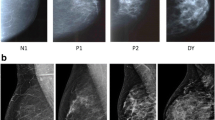
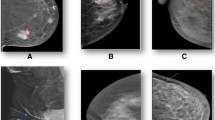
Breast density data was obtained in women attending routine mammographic screening from April 2013 to March 2015 using automated breast density assessment software. Women with the densest breasts were selected for visual interpretation of parenchymal pattern (PP). One hundred non-assessed women, aged 50, 55, 60, 65 and 69-71 years (total = 500), provided controls. Cases included women recalled for assessment (mastectomy or implants excluded) (total = 280). Mammograms reviewed by ten readers and PP classified as: (1) very smooth; (2) mainly smooth; (3) mixed; (4) mainly nodular; (5) very nodular. The ratio of women in each category at each age and screening outcomes were compared by Pearson’s chi-squared test.
Results
Reader agreement for scoring PP was good (intraclass correlation = 0.6302). Proportions of women in each PP category were similar at all ages for controls (p = 0.147) and cases (p = 0.657). The ratio of PP categories did not vary significantly with age in those who underwent biopsy (p = 0.484). Thirty-four cancers were diagnosed. There was a significant correlation between a diagnosis of cancer and nodular PP compared to not nodular PP (p = 0.043).
Conclusions
The ratio of smooth to nodular pattern in women with the densest breasts did not vary with age. The PP of the breast tissue did not affect likelihood of recall to assessment or biopsy. There was a significant relationship between a nodular parenchymal pattern and diagnosis of cancer.
Key Points
• This paper shows that there is good agreement between mammogram readers when classifying mammographic PP on a five-point scale from very smooth to very nodular.
• In non-assessed women with the densest breasts, there is no significant change in the proportions of smooth to nodular patterns with increasing age.
• The likelihood of recall for further assessment or biopsy at assessment is not related to PP in women with highest breast density.
• When recalled for further assessment, significantly more women are diagnosed with cancer in the group with nodular PP on mammography when compared with smooth and mixed patterns.




Similar content being viewed by others
Abbreviations
- ICC:
-
Interclass correlation
- NBSS:
-
National Breast Screening System
- PP:
-
Parenchymal pattern
- VGd:
-
Volpara Grade d
References
Boyd F, Martin LJ, Yaffe MJ et al (2011) Mammographic density and breast cancer risk: current understanding and future prospects. Breast Cancer Res 13:223
van Gils CH, Hendriks JH, Otten JD, Holland R, Verbeek AL (2000) Parity and mammographic breast density in relation to breast cancer risk: indication of interaction. Eur J Cancer Prev 9:105–111
Boyd NF, Byng JW, Jong RA et al (1995) Quantitative classification of mammographic densities and breast cancer risk: results from the Canadian National Breast Screening Study. J Natl Cancer Inst 87:670–675
Chiu SYH, Duffy S, Yen AMF, Tabár L, Smith RA, Chen HH (2010) Effect of baseline breast density on breast cancer incidence, stage, mortality, and screening parameters: 25-year follow-up of a Swedish mammographic screening. Cancer Epidemiol Biomarkers Prev 19:1219–1228
Gierach GL, Ichikawa L, Kerlikowske K et al (2012) Relationship between mammographic density and breast cancer death in the Breast Cancer Surveillance Consortium. J Natl Cancer Inst 104:1218–1227
Wolfe JN (1976) Breast patterns as an index of risk for developing breast cancer. AJR Am J Roentgenol 126:1130–1137
Winkel RR, von Euler-Chelpin M, Nielsen M et al (2015) Inter-observer agreement according to three methods of evaluating mammographic density and parenchymal pattern in a case control study: impact on relative risk of breast cancer. BMC Cancer 15:274
Gram IT, Funkhouser E, Tabár L (1997) The Tabár classification of mammographic parenchymal patterns. Eur J Radiol 24:131–136
Jakes RW, Duffy SW, Ng FC, Gao F, Ng EH (2000) Mammographic parenchymal patterns and risk of breast cancer at and after a prevalence screen in Singaporean women. Int J Epidemiol 29:11–19
Cicchetti DV (1994) Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assessment 6:284–290
R Core Team (2015) A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria Available at: http://www.R-project.org/
Heller SL, Hudson S, Wilkinson LS (2015) Breast density across a regional screening population: effects of age, ethnicity and deprivation. Br J Radiol 88(1055):20150242
Nayak L, Miyake KK, Leung JWT et al (2016) Impact of breast density legislation on breast cancer risk assessment and supplemental screening: a survey of 110 radiology facilities. Breast J 22:493–500
Bernardi D, Macaskill P, Pellegrini M et al (2016) Breast cancer screening with tomosynthesis (3D mammography) with acquired or synthetic 2D mammography compared with 2D mammography alone (STORM-2): a population-based prospective study. Lancet Oncol 17:1105–1116
Skaane P, Bandos AI, Gullien R et al (2013) Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology 267:47–56
McCormack VA, dos Santos Silva I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev 15:1159–1169
Acknowledgements
These findings were presented at ECR 2016.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr Louise Wilkinson.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because local governance approval was obtained from the research and development office as the observations were of routinely collected data.
Ethical approval
Institutional Review Board approval was not required because local governance approval was obtained from the research and development office as the observations of routinely collected data without the need for ethics approval.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in Heller et al. [12].
Methodology
• retrospective
• observational
• performed at one institution
Rights and permissions
About this article
Cite this article
Ward, L., Heller, S., Hudson, S. et al. Parenchymal pattern in women with dense breasts. Variation with age and impact on screening outcomes: observations from a UK screening programme. Eur Radiol 28, 4717–4724 (2018). https://doi.org/10.1007/s00330-018-5420-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5420-4