Abstract
The objective of this study was to compare a newly developed fat-saturated intermediate-weighted (IM-w) 3D fast spin-echo (FSE) sequence with standard 2D IM-w FSE sequences regarding image quality and diagnostic performance in assessing abnormal findings of the knee. MR imaging was performed at 3.0 T in 50 patients. Images were assessed independently by three radiologists. Image quality was rated significantly higher (p < 0.05) for the 2D versus the 3D FSE sequences. Sensitivity for cartilage lesions was slightly higher for the 3D sequence, but specificity was lower. Low contrast objects were better visualized with 2D sequences, while high contrast objects were better shown with the 3D sequence. Confidence scores were higher for 2D than for 3D sequences, but differences were not significant. In conclusion, isotropic 3D FSE IM-w imaging may enhance standard knee MRI by increased visualization of high contrast lesions; however, 3D FSE image quality was lower.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Standard clinical MRI of the knee relies heavily on fat-saturated, two-dimensional T2- or intermediate-weighted fast spin-echo (2D T2- or IM-w FSE) sequences, performed in a reasonable data acquisition time. These sequences have demonstrated good performance in detecting joint abnormalities such as meniscal tears [1, 2], ligament injuries [3] or cartilage damage [4, 5]. Limitations of these sequences, however, have to be considered. These include: (1) relatively thick image sections with gaps and partial volume effects, (2) non-isotropic voxels and (3) acquisition of 2D sequences in all three planes, since reformations are not possible, thus increasing examination time. Using isotropic 3D T2- or IM-weighted techniques may solve these problems and potentially optimize visualization of knee abnormalities. Isotropic voxels would allow reformations with different slice thickness in any imaging plane, reducing imaging time, by eliminating the need to acquire sequences in multiple imaging planes. Three-dimensional imaging sequences of the knee have been tested and previously evaluated [6–11], but most of these were gradient echo sequences, and given different image contrast had limitations in replacing 2D T2- or IM FSE sequences for evaluating internal knee derangements.
In addition to 3D gradient echo sequences, 3D FSE techniques were developed; Mugler et al. described a 3D FSE sequence with variable flip angles and long echo trains first and established it for brain imaging [12, 13]. Subsequently, a new fast recovery 3D FSE sequence with a longer echo train acquisition (3D XETA, eXtended Echo Train Acquisition) was developed by Busse et al. [14] for knee imaging and evaluated by Gold et al. [7], optimizing echo time (TE) and echo train length (ETL), as well as improving scanning efficiency. This sequence allowed acquisition of T2- or IM-weighted 3D FSE images with isotropic resolution in an appropriate data acquisition time with minimal blurring for clinical knee MRI at 1.5 T. However, these investigators [7] limited their evaluation to healthy subjects and did not use this sequence to assess its performance in diagnosing knee abnormalities.
Therefore, the goals of this study were to compare the newly developed fat-saturated IM-weighted 3D FSE sequence to standard, established 2D IM-w FSE sequences, specifically regarding image quality and diagnostic performance in assessment of abnormal findings in the knee. Also we wanted to find out whether one 3D FSE sequence with multi-planar reformations could replace standard 2D FSE sequences obtained in multiple planes in a routine clinical knee examination.
Materials and methods
Patients
This Health Insurance Portability and Accountability Act-compliant (HIPAA) study had institutional review board approval, and informed consent was obtained from all patients. Over a period of 6 months, 50 consecutive patients were recruited and prospectively included in our study. Thirty female and 20 male patients were enrolled (mean age and standard deviation, 37 ± 18.7 years; age range, 15–82 years). Inclusion criteria were knee symptoms in all patients, such as pain or functional limitations; patients were referred by our sports medicine clinic with a history of acute or chronic trauma, suspected meniscal, cartilage or ligamentous injury as well intra-articular bodies and osteoarthritis. Exclusion criteria were previous surgery with implantation of metal hardware and standard contraindications for the use of MRI, including presence of a pace maker and claustrophobia.
MR imaging
All examinations in the 50 patients were performed at 3 T (Signa, GE Healthcare, Waukesha, WI) with an eight-channel receiver element, one element transmit-receive coil (Invivo, Orlando, FL). The system was equipped with 50 mT/m gradients. The volunteers were placed supine in the magnet feet first, with the knee at the center of the coil, lined up with the inferior margin of the patella during imaging. A standard clinical MR examination was performed with the six following sequences: (1) a fat-saturated (fs) two-dimensional intermediate-weighted (IM-w) fast spin-echo (FSE) sequence in a sagittal orientation [repetition time, echo time, (TR/TE): 4,200/50 ms; field of view (FOV): 13 cm; slice thickness (ST): 3 mm; spacing: 0.5 mm; echo train length (ETL): 9; number of signals acquired: 2; matrix: 320 × 256 pixels; bandwidth (BW): 31.25 kHz; acquisition time (AT): 4:28 min]; (2) a fs 2D axial IM-w FSE sequence (TR/TE: 4,200/50 ms; FOV: 13 cm; ST: 4 mm; spacing: 0.5 mm; ETL: 9; number of signals acquired: 2; matrix: 320 × 256 pixels; BW: 31.25 kHz; AT: 4:23 min); (3) a coronal fs 2D IM-w FSE sequence (TR/TE: 4,200/51 ms; FOV: 13 cm; ST: 3 mm; spacing: 0; ETL: 9; number of signal acquired: 2; matrix: 320 × 256 pixels; BW: 31.25 kHz; AT: 4:14 min). Three non-fat saturated 2D sequences were also performed: (4) a sagittal proton-density (PD)-weighted FSE sequence, (5) an axial PD-w FSE sequence and (6) a coronal T1-w FSE sequence. Since these sequences were not included in the comparative analyses, we did not list sequence parameters.
In addition, a sagittal fs 3D XETA-FSE sequence was obtained with the following parameters: TR/TE: 2,500/38 ms; BW: 42 kHz; FOV: 16 cm; ST: 0.7 mm; ETL: 78; number of signal acquired: 0.5; matrix: 256 × 256 pixels; AT: 6:06 min and voxel size: 0.625 × 0.625 × 0.7 mm. Partial Fourier acquisition and ARC parallel imaging reduced imaging time by a factor of 3.4 compared to a standard sequence protocol. Each image dataset was reconstructed in an axial and coronal plane using the software implemented with the sequence and provided by the manufacturer.
Image analysis
All images were evaluated by three board-certified radiologists with expertise in musculoskeletal MRI ranging from 5 to 23 years (GS, LS, TML) on PACS workstations (Agfa, Ridgefield Park, NJ). At the time of analysis, the radiologists were blinded to the clinical history, previous reports and sequence parameters. One of the investigators (OR) brought up the images and recorded each of the readers’ findings. During the reading session, ambient light was kept at a minimum, and no time constraints were used.
Image analysis by the radiologists was performed in two steps. First, sagittal 3D FSE sequences and sagittal 2D FSE sequences were analyzed separately, in random order, not more than 25 sequences at one time. Time between reading sessions was at least 96 h in order to reduce a potential learning bias. Radiologists were asked to grade image quality, using the following criteria: edge sharpness, amount of blurring, artifacts, contrast between fluid and cartilage, contrast between fluid and soft tissue, delineation of small ligamentous structures, and amount of noise. A four-level scale was used, in which 1 indicated optimal image quality. If one or two criteria were not optimal, image quality was graded as 2. If the diagnosis was limited by the criteria listed above, image quality was graded as 3, and if diagnosis was substantially limited, image quality was graded as 4. In addition, presence and absence of an abnormality was graded focusing on cartilage, menisci, ligaments, patellar tendon, bone marrow, intra-articular bodies and joint effusion. A five-level scale was used to grade these abnormalities: grade 1 normal, grade 2 probable absence of disease, grade 3 indicated equivocal findings, grade 4 probable presence of a lesion and grade 5 definite presence of an abnormality.
In a second step, the radiologists reviewed the 3D FSE sequences including axial and coronal reformations side by side with the three sagittal, axial and coronal 2D FSE sequences. They were asked to assess how the 3D FSE sequence compared in performance with the standard 2D FSE sequence by evaluating the three major abnormalities in each study. These abnormalities were selected by an experts’ panel prior to the study based on all sequences available, the report and clinical findings (OR, BM, TML). A three-level scale was used to score the images: 1= the 3D FSE sequence and reformations were better in visualizing lesions than the standard 2D FSE sequences, 2= 3D and 2D FSE images were similar in performance, and 3= 2D FSE sequences were better than 3D FSE sequence and reformations. Finally, radiologists were asked to decide (1) whether the 3D FSE sequence was better =1, same =2 or worse =3 than the standard 2D FSE sequences, (2) whether the 3D FSE sequence including axial and coronal reformations could replace the standard 2D FSE sequences in a routine clinical setting and (3) whether the 3D FSE sequence provided any additional information compared to standard 2D FSE sequences.
Quantitative analysis was also performed calculating effective signal-to-noise-ratios (SNR E ) for both the 3D and 2D FSE sequences with \(SNR_E = \frac{{\tfrac{{SI_{Tissue} }}{{SD_{Background} }}}}{{\sqrt {{\text{data aquisition time}}} }}\), where SI Tissue was the signal intensity of cartilage and SD Background was the standard deviation of the background. Effective contrast-to-noise ratios (CNRE) were calculated for cartilage (Tissue 2) versus fluid (Tissue 1) using the formula \(\begin{aligned} & CNR_E = \frac{{\frac{{SI_{Tissue1} - SI_{Tissue2} }}{{SD_{Background} }}}}{{\sqrt {{\text{data aquisition time}}} }} \\ & \\ \end{aligned} \). Effective SNR and CNR values were calculated to account for the differences in acquisition time between the individual sequences.
Standard of reference
The standard of reference for the MR abnormalities was based on arthroscopic findings in 25 subjects performed by an experienced orthopedic surgeon (BM); knee arthroscopies were performed within an average time interval of 59 ± 39 days to the MR studies. In 25 subjects the standard of reference was based on image analysis by two senior radiologists (TML and LS) in consensus, performed independently, after the study readings, with all available sequences as well clinical examinations, history of each patient and follow-up MR examinations.
Statistical analysis
Differences in image quality, SNRE and CNRE between 3D and 2D FSE sequences were assessed using an ANOVA analysis with a significance threshold of p < 0.05. Differences in specificity and sensitivity as well as in confidence scores in detecting knee abnormalities were assessed using the Wilcoxon signed rank test. Receiver-operator characteristic (ROC) analyses were performed based on the confidence of diagnosing the absence or presence knee abnormalities. Corresponding “area under the curve” (AZ) values were calculated to estimate the diagnostic performance of each cartilage protocol for detecting a lesion. Ninety-five percent confidence intervals were calculated for all AZ values to evaluate significant differences between the protocols [15, 16]. In addition, descriptive statistics were used to present results of direct comparisons. All of the statistical computations were processed using JMP 5.1 (SAS Institute Inc., Cary, NC) and SPSS 11.5 software (SPSS Inc., Chicago, IL).
Results
Image quality
Each of the radiologists scored image quality of the 3D FSE sequences significantly lower (p < 0.05) than that of the standard fs 2D FSE sequences for all anatomical structures except for joint fluid (Table 1). For all evaluated structures, an average score of 1.90 (±0.23) was calculated for the 3D FSE images while a corresponding score of 1.25 (±0.19) was calculated for the 2D FSE images. In particular, a higher amount of image blurring and indistinctness of the structural edges was noted on the 3D FSE images as shown in Figs. 1 and 2. This decreased visualization of low contrast objects in particular within the bone marrow (Fig. 1) and tears of the menisci (Fig. 2). Figure 1 shows images of a patient who underwent cartilage repair with mosaicplasty; the implanted osteochondral plug is not visualized on the 3D FSE image, while it is well shown on the 2D FSE image. The largest difference between individual scores was found for the bone marrow for all radiologists. Bone marrow on the 3D FSE images appeared noisy and indistinct, which limited visualization of bone marrow lesions.
A 24-year-old female patient, who underwent cartilage repair with mosaicplasty. Sagittal MR images obtained with 2D (a) and 3D FSE sequences (b) at 3 T. Note the differences in image quality between sequences, with a substantially lower amount of noise in (a). The implanted osteochondral plug is well visualized on the 2D FSE sequence (arrow in a), but not on the 3D FSE sequence (arrow in b)
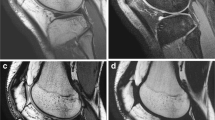
A 45-year-old male patient with an oblique tear of the medial meniscus posterior horn. Sagittal images obtained with 2D (a) and 3D FSE sequences (b) at 3 T. Finding was classified as probably no meniscal lesion by all radiologists in the 3D FSE sequence (arrow in b), whereas the tear is well visualized on the 2D FSE sequence and was diagnosed as a definite tear (arrow in a). This also correlated to the arthroscopic findings
However, high contrast objects, such as small fissures within the cartilage surrounded by joint fluid (Figs. 3, 4, 5) or intra-articular bodies surrounded by fluid (Fig. 6), were better visualized with the 3D FSE sequence due to the thin slice thickness with reduced partial volume effects. For each of the radiologists the smallest difference in image quality between 3D FSE and 2D FSE sequences was found for joint fluid (p > 0.05). Visualization of small structures within the joint fluid, such as synovial debris and synovial bands (Fig. 7), in addition to bodies, was improved.
A 16-year-old male patient with a cartilage defect at the patella. Sagittal 2D (a) and 3D FSE sequences (b). Images show a less than 50% depth cartilage fissure at the patella (arrows). This lesion was missed on the 2D FSE images (a) and diagnosed as a definite lesion on the 3D FSE sequence (b), highlighted by the surrounding joint fluid
A 17-year-old female patient with osteochondritis dissecans. Sagittal 2D (a) and 3D FSE sequences (b). The full thickness cartilage lesion at the medial femoral condyle is not well shown on the 2D FSE sequence (arrow in a), but clearly visualized on the 3D FSE sequence (arrow in b). In particular, the grade of the cartilage defect is more precisely illustrated with the 3D FSE sequence. Joint fluid within the lesion delineates the exact borders of the lesion with the 3D FSE sequence
SNR measurements
Effective SNR and CNR values with standard deviations were calculated for the sagittal 2D and 3D FSE images as well as for the reconstructed 3D FSE sequences. Higher SNR values were found for the 2D FSE sequence (22.7 ± 11.6) than for the 3D FSE sequence (8.9 ± 4.4), which was expected given differences in slice thickness and image quality documented by the above-presented scores. The corresponding effective CNR values with standard deviations were 58.6 (±20.7) for the 2D FSE and 17.4 (±7.7) for the 3D FSE sequence, indicating higher contrast between cartilage and fluid for the 2D FSE sequence. To better control for voxel size, we also measured the effective SNR and CNR values in the reconstructed 2-mm images and obtained similar values as in the 2D sequences (22.3 ± 10.2 and 57.2 ± 33.1, respectively), indicating that reconstruction with larger slice thickness improved SNR and CNR.
Confidence scores
Reviewing the radiologists’ confidence scores in diagnosing knee joint abnormalities revealed that fewer lesions were classified as definite with the 3D FSE sequence than with the 2D FSE sequence. With the 3D FSE sequence, 527 definite diagnoses were made and 573 with the 2D FSE sequence. With the 3D FSE sequence, 208 abnormalities were classified as probable, whereas only 177 were classified as probable with the 2D FSE sequence. Classification varied according to the anatomic site: while for meniscal, ligament and cartilage abnormalities confidence scores were similar, for bone marrow abnormalities performance of the 2D FSE sequences was substantially better. Presence or absence of bodies, however, was graded with higher confidence on the 3D FSE images.
Diagnostic performance
Abnormal findings covered a wide spectrum of mild to severe cartilage, meniscus and ligamentous lesions. Thirty-three cartilage lesions were diagnosed using the available standard of reference. Seven lesions were located at the medial and three at the lateral femoral condyle; three lesions each were located at the medial and lateral tibial plateau. At the trochlea, 4 lesions were found, while 13 defects were located at the patella. Twelve full thickness lesions (grade 4) were diagnosed, nine more than 50% thickness lesions (grade 3) and 7 less than 50% thickness lesions (grade 2). Five lesions were grade 1 lesions, consistent with softening of the cartilage arthroscopically and signal changes and/or swelling on MR images. Thirty-six meniscal abnormalities were diagnosed; 25 were located at the medial meniscus and 11 at the lateral meniscus. Seven were graded as intrasubstance degeneration (grade 1), 12 as simple tears (horizontal or vertical) without deformation (grade 2), 7 as complex tears without deformation (grade 3) and 10 as meniscal tears with deformation (grade 4). Twenty-one ligamentous abnormalities were diagnosed. Six were graded as grade 1 sprain with signal change, nine as partial tear (grade 2 sprain) and six as a complete tear (grade 3 sprain). In addition, other abnormalities were diagnosed, such as bone marrow abnormalities, loose bodies and joint effusions, adding up to a total of 131 abnormalities.
The diagnostic performance in detecting knee abnormalities was evaluated based on the confidence scores used by the radiologists and the previously described standard of reference. The number and percentage of correctly detected abnormalities for definite scores as well as a combination of definite and probable scores were determined and are shown in Table 2. Using definite scores and data from all radiologists, there was only a 6% overall difference in correct detection for all knee joint abnormalities between the 3D FSE and 2D FSE sequences; in 50 patients with a total of 393 abnormalities (131 assessed by 3 radiologists), 230 (59%) abnormalities were correctly diagnosed with high certainty (definite) using the 3D FSE sequence and 254 (65%) with the 2D FSE sequence.
Analyzing the results according to different abnormalities, sequence-specific variations were demonstrated. For meniscal, ligamentous and cartilaginous lesions, the detection rate showed no significant (p > 0.05) differences between the 3D FSE and the 2D FSE sequence. Yet trends were shown with a mildly better detection rate for the 2D FSE sequence for all three lesions and were most evident for ligament lesions. Detection rates, however, were significantly higher for the 2D FSE sequence regarding bone marrow (p < 0.05) abnormalities; 15% more lesions were detected with the 2D FSE sequence than with the 3D FSE sequence. Although the number of detected bodies with the two sequences differed substantially, a significant difference could not be calculated due to the small number evaluated; 71% of intra-articular bodies were detected with the 3D FSE sequence, while only 38% were detected with the 2D FSE sequence, constituting a difference of 33%.
Sensitivity and specificity values were also calculated. While average sensitivity and specificity values for all structures were similar, with only 1% difference for the sensitivity (3D FSE 77% versus 2D FSE 78%) and 3% difference for the specificity (3D FSE 88% versus 2D FSE 91%), more pronounced differences were found for cartilage abnormalities (specificity 24% higher for 2D FSE) and diagnosis of bodies (sensitivity 31% higher for 3D FSE). Sensitivity for cartilage lesions was mildly higher for the 3D FSE (94%) than the 2D FSE sequence (90%). Results were consistent among all three radiologists for all of the different abnormalities.
Results of the ROC analysis are presented in Table 3. Average A Z values calculated from pooled radiologist data for all abnormalities were similar for the 3D and 2D FSE sequences \(\left( {A_Z {\text{ = 0}}{\text{.80}} \pm {\text{0}}{\text{.09 versus }}A_Z {\text{ = 0}}{\text{.83 $ \pm $ 0}}{\text{.12, p $>$ 0}}{\text{.05}}} \right)\). Again, results were consistent among all three radiologists. A Z values for bodies were not calculated since their number was relatively small.
Using data from all radiologists cartilage abnormalities were evaluated with the 3D versus the 2D sequence as follows: detection rate, 76% versus 79% and AZ value, 0.78 versus 0.84 for all lesions. Decreased diagnostic performance was found for lower grade lesions. For meniscal lesions the detection rate for all radiologists was 56% for the 3D versus 60% for the 2D sequence, while the AZ value was 0.86 versus 0.87.
Direct comparison
Assessment of the three major lesions was made in every patient. By comparing the three available planes side by side, diagnostic performance in visualizing the lesions was scored as identical for both sequences in 53%, as better in 11% and as worse in 36% for the 3D FSE sequence by all radiologists. Results were consistent for all three imaging planes and radiologists (Table 4). In 75% of the studies radiologists found that the 3D FSE sequence could replace the sagittal, coronal and axial 2D FSE sequences. Radiologists also found the 3D FSE sequence to provide additional information in 14% of all evaluated images.
Discussion
The results of this study show that isotropic 3D FSE sequences have promise in assessing lesions of the articular cartilage and intraarticular bodies, while they appear limited in the detection of meniscal, ligament and bone marrow abnormalities. While image quality consistently scored lower with the 3D compared with the 2D FSE sequences, the diagnostic performance was similar, though radiologists felt more confident diagnosing abnormalities with the 2D sequences. Interestingly, low contrast objects were not well evaluated with the 3D FSE sequences, but visualization of high contrast objects was enhanced.
The standard sequences for knee joint imaging are fat-saturated IM- or T2-w FSE sequences. These sequences allow excellent visualization of the hyaline cartilage, menisci, tendons and ligaments as well as the capsular structures of the joint and the bone marrow [1–5, 17]. A potential disadvantage of these sequences is the relatively large slice thickness (2–4 mm) with an interslice gap; thus, partial volume effects limit visualization of small structures, and 3D reformations are not possible. In addition, acquisition has to be performed in two or three imaging planes with 2D sequences to fully assess the anatomy of complex joints such as the knee.
With the new 3D FSE sequence available for this study, imaging of the joints could potentially be accelerated by only obtaining one sequence with isotropic voxels that could be reformatted in any imaging plane. This could in particular improve imaging performed under economic constraints; however, SNR and CNR efficiencies are critical to achieve this goal. Diagnostic performance could be potentially improved by the small slice thickness (0.7 mm), better directly visualizing critical structures with more detail, for example, bodies or intra-articular bands such as scar, synovitis or plicae. However, in-plane spatial resolution has to be sacrificed to achieve a reasonable acquisition time and signal-to-noise ratio with isotropic voxels.
A small number of studies have been performed showing the potential of 3D FSE sequences with isotropic voxels [7, 18–20]. In addition to knee imaging, 3D FSE sequences have also been applied for the examination of the biliary tree and the pancreatic duct on MR cholangiopancreatographic (MRCP) images.
Gold et al. [7] compared a similar isotropic 3D fast spin-echo (FSE) sequence at 1.5 T with extended echo-train acquisition (XETA) as in our study with a 2D FSE and a 2D fast recovery FSE (FRFSE) sequence at the knee in healthy volunteers. These investigators concluded that the 3D FSE sequence enables rapid isotropic imaging of the knee with volumetric data for the diagnosis of any relevant derangement while improving clinical efficiency by saving acquisition time through reformations. They also showed signal variations in tissues for the 2D and 3D FSE sequences: while SNR of cartilage and muscle was higher for the 3D FSE sequence (TR/TE, 2,500/38 ms), the 2D FSE sequence (TR/TE, 4,000/38) had higher SNR for fluid and higher CNR between cartilage and fluid. In that study, imaging was performed at 1.5 T, while we used 3.0 T, which can potentially enhance the performance by increasing SNR.
Some investigators also used 3D gradient echo sequences to better study knee abnormalities [10, 11, 21–23]. Ruehm et al. [11] investigated an optimized 3D dual echo steady state (3D DESS) sequence. These investigators found that fewer surface cartilage lesions were depicted with the 3D DESS than with the standard 2D T2-weighted FSE sequences (sensitivity: 43%, 60%; specificity: 92%, 92%) and a moderately higher sensitivity in detecting cartilage softening with the 3D DESS sequence (73%) compared to the 2D FSE sequence (53%). The results of our study were more favorable for the 3D FSE sequence; the 3D DESS sequence therefore may not be suited to replace FSE sequences.
Duc et al. [21] used a 3D isovoxel true fast imaging with steady-state precession (FISP) sequence with water excitation and secondary multiplanar reformations (acquisition time, 3 min) and examined 29 patients concerning the accuracy in detecting meniscal, cartilage and anterior cruciate ligament (ACL) abnormalities. Using arthroscopy as their standard of reference, a diagnostic performance of the 3D FISP sequence was found that was comparable to the 2D FSE standard sequence.
But to the best of our knowledge, clinical studies using 3D FSE sequences for imaging of knee joint lesions at 3 T and comparing it standard clinical sequences have not yet been performed. The results of our study show that the new 3D FSE sequence, despite its clear deficit in image quality, only has relatively minor limitations in diagnostic performance compared to the standard 2D FSE sequences. Interestingly, visualization of low and high contrast objects was substantially different. Lesions of bone marrow and menisci, for example, were not well demonstrated with the 3D FSE sequence, and anatomical detail appeared indistinct and blurry. This made the diagnosis of subtle lesions and fissures within those low contrast structures difficult. This finding of decreased visualization is reflected in the results of the image quality and confidence scores, as well as the detection rates and ROC analysis for low contrast structures such as bone marrow and menisci. However, high contrast objects, including anatomical structures adjacent to joint fluid, such as cartilage, were better visualized with the new 3D FSE sequence than with the 2D FSE sequence. This better visualization of high contrast objects made it easier to depict small objects, including bodies, linear intra-articular bands, plicae or synovial debris within joint fluid and also better depicted small fissures in cartilage that were highlighted by fluid.
However, a substantial difference between the 3D FSE sequence and the standard 2D FSE sequence was also seen in the confidence scores of the radiologists in rendering a diagnosis. Due to the overall limited image quality with the 3D FSE sequence, radiologists gave less definite but more probable diagnoses with the 3D FSE images than with the 2D FSE images.
The results of the side-by-side comparison showed that the radiologists diagnosed in 53% of all evaluated images the performance of 2D and 3D FSE sequences as equally good. This reflects the overall impression of the other results in our study. Still in 36% of all images radiologists considered the diagnostic performance of 3D FSE sequence as worse than the performance of the standard 2D FSE sequence. This was mainly due to the low image quality of the reformations, which decreased visualization of anatomical structures substantially though a 2-mm slice thickness for the reformations was chosen. Interestingly, however, in 75% of cases, the radiologists found that that one 3D FSE sequence with reformations could replace three 2D FSE sequences in a clinical routine examination.
A limitation of our study was that we compared sequences with different slice thicknesses and spatial resolutions. However, we wanted to compare the new sequence with routinely used clinical sequences. Also we did not want to reconstruct the sagittal 3D FSE sequences with a larger slice thickness, as we wanted to assess the full potential of the small slice thickness. An additional limitation is the fact that we had an arthroscopic standard of reference in only 25 of our 50 patients. However, great care was taken to obtain the best possible standard of reference in the other cases using all available sequences, consensus readings, clinical information as well as follow-up MR studies. Although all radiologists were blinded to sequence parameters, the fact that the individual sequences have specific morphological features and the 3D FSE has more slices than the 2D FSE sequence may have made the sequences easily identifiable and thus may have introduced a bias. Additional criticism may be raised by the fact that 96 h between the two reading sessions may not be enough time to prevent a learning bias. Also, please note that the relatively limited number of lesions at each anatomic site is a potential limitation of the study.
In conclusion, this study showed that though image quality with the new 3D FSE sequence is clearly limited compared to standard 2D FSE sequences, diagnostic performance was similar, and in a high percentage the radiologists felt that the 3D FSE sequence with reformations could replace three standard 2D FSE sequences. Though we currently would not recommend using this sequence as a substitute for standard 2D sequences, we found it to be useful in better assessing high contrast structures, such as superficial cartilage lesions, synovial structures and intra-articular bodies surrounded by joint fluid. With further optimization, however, we believe that one 3D FSE sequence reformatted in multiple planes may eventually be substituted for separately acquired 2D sequences, substantially reducing knee MR examination time.
References
Escobedo EM, Hunter JC, Zink-Brody GC, Wilson AJ, Harrison SD, Fisher DJ (1996) Usefulness of turbo spin-echo MR imaging in the evaluation of meniscal tears: comparison with a conventional spin-echo sequence. AJR Am J Roentgenol 167:1223–1227
Jee WH, McCauley TR, Kim JM et al (2003) Meniscal tear configurations: categorization with MR imaging. AJR Am J Roentgenol 180:93–97
Schaefer FK, Schaefer PJ, Brossmann J et al (2006) Value of fat-suppressed PD-weighted TSE-sequences for detection of anterior and posterior cruciate ligament lesions-comparison to arthroscopy. Eur J Radiol 58:411–415
Bredella MA, Tirman PF, Peterfy CG et al (1999) Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol 172:1073–1080
Sonin AH, Pensy RA, Mulligan ME, Hatem S (2002) Grading articular cartilage of the knee using fast spin-echo proton density-weighted MR imaging without fat suppression. AJR Am J Roentgenol 179:1159–1166
Gold GE, Burstein D, Dardzinski B, Lang P, Boada F, Mosher T (2006) MRI of articular cartilage in OA: novel pulse sequences and compositional/functional markers. Osteoarthritis Cartilage 14(Suppl A):A76–86
Gold GE, Busse RF, Beehler C et al (2007) Isotropic MRI of the knee with 3D fast spin-echo extended echo-train acquisition (XETA): initial experience. AJR Am J Roentgenol 188:1287–1293
Gold GE, Fuller SE, Hargreaves BA, Stevens KJ, Beaulieu CF (2005) Driven equilibrium magnetic resonance imaging of articular cartilage: initial clinical experience. J Magn Reson Imaging 21:476–481
Duc SR, Mengiardi B, Pfirrmann CW, Hodler J, Zanetti M (2007) Improved visualization of collateral ligaments of the ankle: multiplanar reconstructions based on standard 2D turbo spin-echo MR images. Eur Radiol 17:1162–1171
Fischbach F, Bruhn H, Unterhauser F et al (2005) Magnetic resonance imaging of hyaline cartilage defects at 1.5T and 3.0T: comparison of medium T2-weighted fast spin echo, T1-weighted two-dimensional and three-dimensional gradient echo pulse sequences. Acta Radiol 46:67–73
Ruehm S, Zanetti M, Romero J, Hodler J (1998) MRI of patellar articular cartilage: evaluation of an optimized gradient echo sequence (3D-DESS). J Magn Reson Imaging 8:1246–1251
Mugler JP 3rd (1999) Overview of MR imaging pulse sequences. Magn Reson Imaging Clin N Am 7:661–697
Park J, Mugler JP 3rd, Horger W, Kiefer B (2007) Optimized T1-weighted contrast for single-slab 3D turbo spin-echo imaging with long echo trains: application to whole-brain imaging. Magn Reson Med 58:982–992
Busse RF, Hariharan H, Vu A, Brittain JH (2006) Fast spin echo sequences with very long echo trains: design of variable refocusing flip angle schedules and generation of clinical T2 contrast. Magn Reson Med 55:1030–1037
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–843
Link TM, Stahl R, Woertler K (2007) Cartilage imaging: motivation, techniques, current and future significance. Eur Radiol 17:1135–1146
Rodegerdts EA, Boss A, Riemarzik K et al (2006) 3D imaging of the whole spine at 3 T compared to 1.5 T: initial experiences. Acta Radiol 47:488–493
Sodickson A, Mortele KJ, Barish MA, Zou KH, Thibodeau S, Tempany CM (2006) Three-dimensional fast-recovery fast spin-echo MRCP: comparison with two-dimensional single-shot fast spin-echo techniques. Radiology 238:549–559
Zhang J, Israel GM, Hecht EM, Krinsky GA, Babb JS, Lee VS (2006) Isotropic 3D T2-weighted MR cholangiopancreatography with parallel imaging: feasibility study. AJR Am J Roentgenol 187:1564–1570
Duc SR, Pfirrmann CW, Koch PP, Zanetti M, Hodler J (2008) Internal knee derangement assessed with 3-minute three-dimensional isovoxel true FISP MR sequence: preliminary study. Radiology 246:526–535
Duc SR, Koch P, Schmid MR, Horger W, Hodler J, Pfirrmann CW (2007) Diagnosis of articular cartilage abnormalities of the knee: prospective clinical evaluation of a 3D water-excitation true FISP sequence. Radiology 243:475–482
Siepmann DB, McGovern J, Brittain JH, Reeder SB (2007) High-resolution 3D cartilage imaging with IDEAL SPGR at 3 T. AJR Am J Roentgenol 189:1510–1515
Acknowledgments
We would like to thank Troy A. Lewein, MSK Clinical Development, GE Healthcare, and Eric Han, GE Healthcare, for their important contributions in setting up the protocols and giving technical advice.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Ristow, O., Steinbach, L., Sabo, G. et al. Isotropic 3D fast spin-echo imaging versus standard 2D imaging at 3.0 T of the knee—image quality and diagnostic performance. Eur Radiol 19, 1263–1272 (2009). https://doi.org/10.1007/s00330-008-1260-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-008-1260-y