Abstract
Magnetic resonance imaging (MRI) is increasingly used in the classification and evaluation of osteoarthritis (OA). Many studies have focused on knee OA, investigating the association between MRI-detected knee structural abnormalities and knee pain. Hip OA differs from knee OA in many aspects, but little is known about the role of hip structural abnormalities in hip pain. This study aimed to systematically evaluate the association of hip abnormalities on MRI, such as cartilage defects, bone marrow lesions (BMLs), osteophytes, paralabral cysts, effusion-synovitis, and subchondral cysts, with hip pain. We searched electronic databases from inception to February 2024, to identify publications that reported data on the association between MRI features in the hip joint and hip pain. The quality of the included studies was scored using the Newcastle-Ottawa Scale (NOS). The levels of evidence were evaluated according to the Cochrane Back Review Group Method Guidelines and classified into five levels: strong, moderate, limited, conflicting, and no evidence. A total of nine studies were included, comprising five cohort studies, three cross-sectional studies, and one case-control study. Moderate level of evidence suggested a positive association of the presence and change of BMLs with the severity and progress of hip pain, and evidence for the associations between other MRI features and hip pain were limited or even conflicting. Only a few studies with small to modest sample sizes evaluated the association between hip structural changes on MRI and hip pain. BMLs may contribute to the severity and progression of hip pain. Further studies are warranted to uncover the role of hip MRI abnormalities in hip pain. The protocol for the systematic review was registered with PROSPERO (https://www.crd.york.ac.uk/PROSPERO/, CRD42023401233).
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Intruduction
Osteoarthritis (OA) is a common musculoskeletal disease of the entire joint, characterized by pain and disability [1]. The hip joint is a frequently affected site of OA [2], affecting more than 240 million people in the world [3]. The pathophysiology of OA involves multiple tissues, including cartilage, bone, ligaments, synovium, and muscles [2, 4]. Understanding the involvement of these tissues in joint symptoms is crucial for developing effective treatment strategies. Although conventional x-rays are frequently used for the diagnosis and classification of OA, soft tissues cannot be adequately evaluated using this technique. Moreover, the available evidence does not show a consistent association between radiographic features and OA pain [5, 6]. More advanced imaging techniques, especially magnetic resonance imaging (MRI), offer much higher sensitivity in detecting early signs of joint damage, making it an invaluable tool for evaluating OA and its associated pain [7, 8].
In contrast to the extensive body of research examining factors associated with knee pain, there has been much fewer studies investigating the source of hip pain [9]. The xcharacteristics of hip OA differ significantly from knee OA in many aspects including epidemiology, prognosis, pathophysiology, anatomical and biomechanical factors, clinical presentation, and pain management [10]. Thus, the etiology and contributing factors for hip pain can differ from those of knee pain. It has been shown that knee pain is associated with several MRI features such as bone marrow lesions (BMLs) [11], effusion/synovitis [12, 13], meniscus tear, infrapatellar fat pad [14], osteophytes [15] and cartilage defects [16]. Clinical studies have gone further to explore the use of BMLs and effusion-synovitis as treatment targets for knee OA [17,18,19,20]. However, few studies have evaluated the role of MRI features in the hip in the assessment, prognosis, and treatment of hip OA. Therefore, this study aimed to systematically review studies evaluating the association between MRI abnormalities and hip pain.
Materials and methods
Protocol registration
The protocol for the systematic review was registered with PROSPERO (https://www.crd.york.ac.uk/PROSPERO/, CRD42023401233). This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [21]. The report of this study followed the Cochrane Handbook for Systematic Reviews of Interventions [22]. This study was a systematic review and ethics committee review was not applicable.
Data source and search strategy
We searched Medline (via Ovid), Web of science, Embase (via Ovid), and Cumulative Index to Nursing & Allied Health Literature (CINAHL) from inception to June 2024, for relevant studies evaluating the association of MRI abnormalities in the hip with hip pain. The following search terms were used: ‘hip’, ‘hip joint’, ‘pain’, ‘MRI’, ‘osteoarthritis’, detailed search strategies are provided in the Supplementary Methods. We also checked the citation lists of the included studies and relevant systematic reviews and gray literature (e.g. conference abstract) for additional studies.
Study selection
Two authors (HF and XZ) conducted an independent review of the titles and abstracts of all identified studies, followed by retrieving the full texts of relevant studies for further screening. The full-text reviews were performed in accordance with the selection criteria outlined in the registered protocol. Specifically, observational studies evaluating the association between MRI abnormalities (e.g. BMLs or cartilage defect) and pain in the hip joint were included. Animal studies or studies without data on MRI features and/or hip pain were excluded. There was no restriction on language.
Data extraction
Two authors (HF and XZ) independently extracted data from each included study. The extracted data included: (1) study characteristics (the first author, year of publication, place (country/territory), study design, and sample size); (2) characteristics of the study population (e.g. age, sex, OA patients or community-dwelling participants); (3) MRI features (e.g. subchondral cysts, paralabral cysts, cartilage defects, BMLs, osteophytes, and effusion/synovitis) (Table 1); (4) assessment of hip pain, (5) main findings for the association between MRI features and hip pain; and (6) adjusted covariates.
Assessment of study quality and credibility of evidence
Two authors (HF and XZ) independently assessed the methodological quality of the included studies using the Newcastle-Ottawa Scale (NOS) for cohort studies [23] and case-control studies [24], and an extension for cross-sectional studies [25]. Differences in scoring were resolved by discussion or by consulting the third author (GC). The possible scores of study quality ranged from 0 to 9 for cohort studies, 0–8 for cross-sectional and case-control studies, with higher scores indicating higher quality. A score of ≥ 7 was considered high study quality for cohort studies [26], cross-sectional studies [27] and case-control studies [28].
The same two authors independently evaluated the credibility of evidence for the association between each MRI feature and hip pain on the basis of the guidelines of the Cochrane Collaboration Back Review Group [29]. The credibility of evidence was categorized into five levels based on the following criteria: (1) Strong: multiple high-quality cohort studies show generally consistent findings, (2) Moderate: One high-quality cohort study and at least two high-quality cross-sectional studies or only at least three high-quality cross-sectional studies show generally consistent findings, (3) Limited: a single cohort study, or up to two cross-sectional studies show less consistent findings, (4) Conflicting: no consistent findings were reported, (5) No evidence: no studies were published.
Result
Literature search
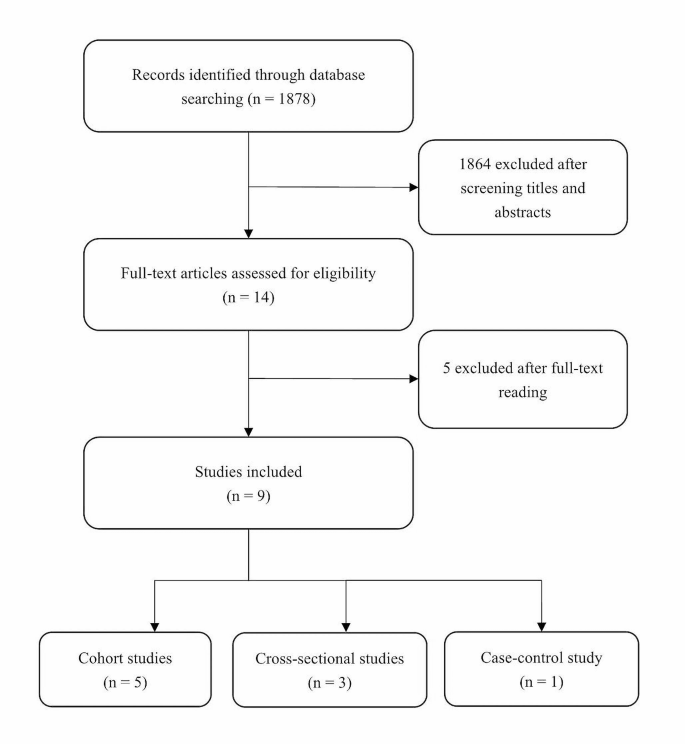
The flowchart of the study selection process is shown in Fig. 1. We identified a total of 1878 potentially relevant records from electronic search. After screening the titles and abstracts, 1864 were excluded. From the remaining 14 records, we further excluded 5 irrelevant studies, leaving 9 studies in this systematic review. Among the studies included, 5 were cohort studies [30,31,32,33,34], 3 were cross-sectional studies [35,36,37], and 1 was a case-control study [38].
Characteristics of included studies
Table 2 shows the characteristics of included studies. Overall, the sample size of the studies were small to modest (n = 19 to 237), and the follow-up time of the 5 cohort studies ranged from 1 to 2.3 years. Among the 9 included studies, 4 examined multiple MRI features [32, 35, 37, 38] and 5 examined a single MRI feature [30, 31, 33, 34, 36]. Three studies were conducted in the same population [30, 33, 34]. Four studies used a 1.5T MRI [30, 33, 34, 36], four used a 3T scanners [31, 32, 35, 38], and the remaining one did not report the strength of MRI used [37]. Most of the studies used sagittal imaging [30, 32,33,34, 37, 38], with two studies using both sagittal, coronal and oblique axial imaging [32, 38], only one study used coronal and sagittal imaging [35], and one study used coronal imaging alone [36]. The patients investigated in the included studies were essentially middle-aged and older adults (mean age 46.5 to 66 years, 27.6-57.9% males), except for one study that examined high-impact athletes in their 20s and 30s [38].
Assessment of study quality
Five of the 9 studies (55.6%) were scored above the high-quality threshold (i.e. ≥7) according to the NOS assessment. For cross-sectional studies, only 1 of the 3 studies was scored high-quality, with the main issues being small sample size, sample representativeness, and the lack of comparison between respondents and non-respondents. Meanwhile, 4 of the 5 cohort studies were above the high-quality threshold, and only 1 study had issues with the representation and selection of exposed and non-exposed groups (Supplementary Tables 1–3).
Association between MRI features and hip pain
Subchondral cysts
One cross-sectional study [35], one case-control study [38] and one cohort study [32] evaluated the association between subchondral cysts and hip pain (Table 3). The credibility of the evidence was limited. The cross-sectional study showed a positive correlation between total subchondral cyst score (grade 0–2) and more severe hip pain score, assessed by the Harris Hip Score and Hip Disability and Osteoarthritis Outcome Score (HOOS) pain subscale (rank correlation coefficient = 0.37, P = 0.001) [35]. The case-control study did not observe a significant difference in subchondral cysts (grade 0–2) between symptomatic and control hips in athletes (8% vs. 7%, odds ratio (OR) = 1.29, 95% confidence interval (CI) 0.51 to 3.23) [38]. The cohort study showed a boardline significant association between baseline subchondral cyst score (grade 0–2) and change in hip pain (rank correlation coefficient = 0.30, p = 0.051) [32]. Moreover, the cohort study found a significant correlation between progression of subchondral cysts and change in HOOS symptoms other than pain (i.e. functional disability and stiffness) (rank correlation coefficient = 0.30, p = 0.03) but not hip pain score over 1.5 years (rank correlation coefficient = 0.18, p = 0.19) [32].
Paralabral cyst
One cross-sectional study [37] and one cohort study [32] evaluated the association between paralabral cyst and hip pain (Table 3). The credibility of the evidence was limited. The cross-sectional study found that paralabral cyst scores, based on the Hip Osteoarthritis MRI Scoring System (HOAMS), were similar in painless and painful hips (mean paralabral cyst score: 0.81 vs. 0.91, p = 0.39) [37]. Consistently, the cohort study found that neither baseline nor progression of paralabral cysts was associated with change in HOOS pain or other subscales, except that progression of paralabral cysts was associated with HOOS activity of daily living subscale (rank correlation coefficient = 0.30, p = 0.03) [32].
Effusion-synovitis
One cross-sectional study [37], one case-control study [38] and one cohort study [34] showed inconsistent findings for the association between hip effusion-synovitis and hip pain (Table 3). The credibility of the evidence was conflicting. The cohort study observed a significant positive correlation between presence of hip effusion-synovitis at two/three sites and presence of hip pain (PR (95% CI): 1.42 (1.05, 1.93)), although there was no significant correlation between change in effusion-synovitis size and change in hip pain [34]. By contrast, the case-control study showed an inverse correlation between effusion-synovitis and the presence of hip symptoms (OR (95% CI) 0.46 (0.26, 0.81)), before and after adjusting for age, sex, and BMI [38]. The remaining cross-sectional study reported no significant associations between joint effusion/synovitis and hip pain [37].
Cartilage defects
One cohort study [33], one case-control study [38] and two cross-sectional studies [35, 37] examined the association between cartilage defects and hip pain (Table 3). The credibility of the evidence was limited. The cohort study reported higher levels of Western Ontario and McMaster Universities Arthritis Index (WOMAC) hip pain in individuals with any type of hip cartilage defects (PR (95% CI): 1.20 (1.02, 1.35)) and secondary cartilage defects (PR (95% CI): 1.40 (1.09, 1.80)) [33]. One cross-sectional study reported a significant linear correlation between cartilage defects score and Visual Analogue Scale (VAS) hip pain (r = 0.46, P < 0.001), although cartilage defects score was not statistically significantly different between individuals with and those without hip pain (mean cartilage defects score: 1.23 vs. 0.75, p = 0.18) [37], another cross-sectional study found a significant correlation between acetabular cartilage score and HOOS pain (r = 0.25, p = 0.026), but there’s no correlation between femoral cartilage score and HOOS pain (rs=0.17, p = 0.146) [35].
Osteophytes
One cross-sectional study [37] examined the relationship between MRI-detected osteophytes and hip pain (Table 3), showing a positive correlation between osteophyte score and VAS pain (r = 0.5811, p < 0.0001), and there was a higher osteophyte score in the inferomedial compartment in individuals with hip pain than those without (3.0 vs. 2.0, p = 0.03) [37]. The credibility of evidence was limited.
BMLs
Three cohort studies [30,31,32], three cross-sectional studies [35,36,37], and one case-control study [38] evaluated the association between BMLs and hip pain (Table 3). The credibility of evidence was moderate. All three cohort studies consistently reported a significant association between BMLs and hip pain, with one showing that change in BML size was significantly associated with change in hip pain (regression coefficient [β] (95% CI): 0.85 (0.00, 1.71)), and the severity of hip pain was associated with a per square centimeter increase in the size of acetabular BML (regression coefficient [β] (95% CI): 4.18 (1.54, 6.88)) [30]. The second cohort study found that Modified Harris Hip Score (MHHS) pain score was significantly lower in individuals with BMLs than those without, regardless of the size of BMLs (p < 0.05) [31], and the third cohort study indicated that baseline BML size was significantly associated with worsening of HOOS pain subscale (regression coefficient [β] (95% CI): 0.690 (0.464, 0.913)) [32]. All three cross-sectional studies reported positive correlations between BML scores and hip pain (r = 0.29 to 0.51, p < 0.05) [35,36,37], and the remaining case-control study did not observe a significant differences in BML scores between symptomatic and control hips [38].
Discussion
This systematic review screened and evaluated studies that described the association between MRI-detected hip abnormalities and hip pain, and several MRI features were identified, such as osteophytes, subchondral cysts, paralabral cysts, effusion-synovitis, BMLs and cartilage defects. Overall, the number, sample size, and quality of included studies were inferior to studies focusing on the knee, and current evidence suggests that BMLs, cartilage defects, and osteophytes may be associated with the presence and severity of hip pain, while subchondral and paralabral cysts may not. Moreover, the association between effusion-synovitis and hip pain was conflicting. Considering the paucity of studies examining their association, a robust conclusion cannot be reached [39]. Thus, more studies are required to validate whether these MRI features contribute to the presence and severity of hip pain.
The credibility of evidence for the association between each of the hip MRI features and hip pain was limited or even conflicting, except that there was a moderate level of evidence for the association between BMLs and hip pain. This can be attributed to various reasons. Firstly, the limited number of included studies may have restricted the breadth and depth of the analysis, potentially leading to less robust conclusions. Secondly, some of the included studies might have exhibited lower overall quality of evidence due to factors such as small sample sizes and inadequate representativeness, impacting the reliability and validity of the findings. Moreover, our research methodology, which involved aggregating study results and applying uniform criteria, while simple, may have hindered the effective synthesis and interpretation of the data, potentially resulting in less accurate or comprehensive outcomes.
We found moderate evidence of a positive association between BMLs and hip pain. These findings are similar to other studies showing a significant association between BMLs and knee pain [11, 40], suggesting that BMLs could be a potential cause or indicator of both knee and hip OA. This could contribute to the management of hip OA, as effectively managing the progression of BMLs may reduce knee pain in knee OA with BMLs [18]. The additional MRI features in this study, despite showing limited or conflicting evidence, play a role in semi-quantitative evaluation of hip OA [41]. These features, awaiting further study, hold promise for distinguishing hip OA subtypes and informing its diagnosis and treatment.
The strength of this study is that we systematically screened studies that evaluated the association between hip MRI abnormalities and hip pain and employed a pre-specified assessment system to qualitatively evaluate the credibility of evidence. There are several limitations in this study. First, we categorized the results of the included studies as either negative or positive based solely on statistical significance, without considering the influence of sample size on the outcomes, and this may have overlooked false negative findings. However, the limited number of studies disabled us from conducting a meta-analysis to pool these results. Second, we scored the methodological quality of the included studies with different designs. The subjective awareness of the evaluator can have an impact on the results of the assessment, leading to biases, although the scores were rated by different authors to reach a consensus.
In conclusion, only a few studies with small to modest sample sizes evaluated the association between hip structural changes on MRI and hip pain. BMLs may contribute to the severity and progression of hip pain. Further studies are warranted to uncover the role of hip MRI abnormalities in hip pain.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Hutton CW (1987) Generalised osteoarthritis: an evolutionary problem? Lancet. (London England) 1(8548):1463–1465. https://doi.org/10.1016/s0140-6736(87)92209-4
Lespasio MJ, Sultan AA, Piuzzi NS, Khlopas A, Husni ME, Muschler GF, Mont MA (2018) Hip osteoarthritis: a primer. Permanente J 22:17–084. https://doi.org/10.7812/tpp/17-084
Katz JN, Arant KR, Loeser RF (2021) Diagnosis and treatment of hip and knee osteoarthritis: a review. JAMA 325(6):568–578. https://doi.org/10.1001/jama.2020.22171
Loeser RF, Goldring SR, Scanzello CR, Goldring MB (2012) Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum 64(6):1697–1707. https://doi.org/10.1002/art.34453
Neogi T, Felson D, Niu J, Nevitt M, Lewis CE, Aliabadi P, Sack B, Torner J, Bradley L, Zhang Y (2009) Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. BMJ (Clinical Res ed) 339:b2844. https://doi.org/10.1136/bmj.b2844
Kim C, Nevitt MC, Niu J, Clancy MM, Lane NE, Link TM, Vlad S, Tolstykh I, Jungmann PM, Felson DT, Guermazi A (2015) Association of hip pain with radiographic evidence of hip osteoarthritis: diagnostic test study. BMJ (Clinical Res ed) 351:h5983. https://doi.org/10.1136/bmj.h5983
Guermazi A, Roemer FW, Haugen IK, Crema MD, Hayashi D (2013) MRI-based semiquantitative scoring of joint pathology in osteoarthritis. Nat Rev Rheumatol 9(4):236–251. https://doi.org/10.1038/nrrheum.2012.223
Roemer FW, Guermazi A, Demehri S, Wirth W, Kijowski R (2022) Imaging in Osteoarthritis. Osteoarthr Cartil 30(7):913–934. https://doi.org/10.1016/j.joca.2021.04.018
Sandhar S, Smith TO, Toor K, Howe F, Sofat N (2020) Risk factors for pain and functional impairment in people with knee and hip osteoarthritis: a systematic review and meta-analysis. BMJ open 10(8):e038720. https://doi.org/10.1136/bmjopen-2020-038720
van der Hall M, Hinman RS, Peat G, de Zwart A, Quicke JG, Runhaar J, van der Knoop J, de Rooij M, Meulenbelt I, Vliet Vlieland T, Lems WF, Holden MA, Foster NE, Bennell KL (2022) How does hip osteoarthritis differ from knee osteoarthritis? Osteoarthr Cartil 30(1):32–41. https://doi.org/10.1016/j.joca.2021.09.010
Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, Kazis L, Gale DR (2001) The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med 134(7):541–549. https://doi.org/10.7326/0003-4819-134-7-200104030-00007
Hill CL, Hunter DJ, Niu J, Clancy M, Guermazi A, Genant H, Gale D, Grainger A, Conaghan P, Felson DT (2007) Synovitis detected on magnetic resonance imaging and its relation to pain and cartilage loss in knee osteoarthritis. Ann Rheum Dis 66(12):1599–1603. https://doi.org/10.1136/ard.2006.067470
Wang X, Jin X, Han W, Cao Y, Halliday A, Blizzard L, Pan F, Antony B, Cicuttini F, Jones G, Ding C (2016) Cross-sectional and longitudinal associations between knee joint effusion synovitis and knee Pain in older adults. J Rhuematol 43(1):121–130. https://doi.org/10.3899/jrheum.150355
Pan F, Han W, Wang X, Liu Z, Jin X, Antony B, Cicuttini F, Jones G, Ding C (2015) A longitudinal study of the association between infrapatellar fat pad maximal area and changes in knee symptoms and structure in older adults. Ann Rheum Dis 74(10):1818–1824. https://doi.org/10.1136/annrheumdis-2013-205108
Zhu Z, Laslett LL, Jin X, Han W, Antony B, Wang X, Lu M, Cicuttini F, Jones G, Ding C (2017) Association between MRI-detected osteophytes and changes in knee structures and pain in older adults: a cohort study. Osteoarthr Cartil 25(7):1084–1092. https://doi.org/10.1016/j.joca.2017.01.007
Everhart JS, Abouljoud MM, Flanigan DC (2019) Role of full-thickness cartilage defects in knee osteoarthritis (OA) incidence and progression: data from the OA Initiative. J Orthop Res 37(1):77–83. https://doi.org/10.1002/jor.24140
Eriksen EF (2015) Treatment of bone marrow lesions (bone marrow edema). BoneKEy Rep 4:755. https://doi.org/10.1038/bonekey.2015.124
Callaghan MJ, Parkes MJ, Hutchinson CE, Gait AD, Forsythe LM, Marjanovic EJ, Lunt M, Felson DT (2015) A randomised trial of a brace for patellofemoral osteoarthritis targeting knee pain and bone marrow lesions. Ann Rheum Dis 74(6):1164–1170. https://doi.org/10.1136/annrheumdis-2014-206376
Cai G, Aitken D, Laslett LL, Pelletier JP, Martel-Pelletier J, Hill C, March L, Wluka AE, Wang Y, Antony B, Blizzard L, Winzenberg T, Cicuttini F, Jones G (2020) Effect of Intravenous Zoledronic Acid on Tibiofemoral cartilage volume among patients with knee osteoarthritis with bone marrow lesions: a Randomized Clinical Trial. JAMA 323(15):1456–1466. https://doi.org/10.1001/jama.2020.2938
Wang Z, Jones G, Winzenberg T, Cai G, Laslett LL, Aitken D, Hopper I, Singh A, Jones R, Fripp J, Ding C, Antony B (2020) Effectiveness of Curcuma longa Extract for the treatment of symptoms and effusion-synovitis of knee osteoarthritis : a Randomized Trial. Ann Intern Med 173(11):861–869. https://doi.org/10.7326/m20-0990
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2023) Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). www.training.cochrane.org/handbook
Wells GA, Wells G, Shea B, Shea B, O’Connell D, Peterson J, Welch, Losos M, Tugwell P, Ga SW, Zello GA, Petersen JA (2014) The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. In
Burfield M, Sayers M, Buhmann R (2023) The association between running volume and knee osteoarthritis prevalence: a systematic review and meta-analysis. Phys Therapy Sport : Official J Association Chart Physiotherapists Sports Med 61:1–10. https://doi.org/10.1016/j.ptsp.2023.02.003
Moskalewicz A, Oremus M (2020) No clear choice between Newcastle-Ottawa Scale and Appraisal Tool for cross-sectional studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J Clin Epidemiol 120:94–103. https://doi.org/10.1016/j.jclinepi.2019.12.013
Mahdi SS, Allana R, Battineni G, Khalid T, Agha D, Khawaja M, Amenta F (2022) The promise of telemedicine in Pakistan: a systematic review. Health Sci Rep 5(1):e438. https://doi.org/10.1002/hsr2.438
Neal BS, Lack SD, Lankhorst NE, Raye A, Morrissey D, van Middelkoop M (2019) Risk factors for patellofemoral pain: a systematic review and meta-analysis. Br J Sports Med 53(5):270–281. https://doi.org/10.1136/bjsports-2017-098890
Su B, Qin W, Xue F, Wei X, Guan Q, Jiang W, Wang S, Xu M, Yu S (2018) The relation of passive smoking with cervical cancer: a systematic review and meta-analysis. Medicine 97(46):e13061. https://doi.org/10.1097/md.0000000000013061
van Tulder M, Furlan A, Bombardier C, Bouter L (2003) Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 28(12):1290–1299. https://doi.org/10.1097/01.Brs.0000065484.95996.Af
Ahedi H, Aitken D, Blizzard L, Cicuttini F, Jones G (2014) A population-based study of the association between hip bone marrow lesions, high cartilage signal, and hip and knee pain. Clin Rheumatol 33(3):369–376. https://doi.org/10.1007/s10067-013-2394-0
Koyama T, Fukushima K, Uchida K, Ohashi Y, Uchiyama K, Takahira N, Takaso M (2022) Is bone marrow oedema in patients with labral tear an indicator of hip pain? J Orthop Surg Res 17(1):420. https://doi.org/10.1186/s13018-022-03243-w
Schwaiger BJ, Gersing AS, Lee S, Nardo L, Samaan MA, Souza RB, Link TM, Majumdar S (2016) Longitudinal assessment of MRI in hip osteoarthritis using SHOMRI and correlation with clinical progression. Semin Arthritis Rheum 45(6):648–655. https://doi.org/10.1016/j.semarthrit.2016.04.001
Ahedi HG, Aitken DA, Blizzard LC, Ding CH, Cicuttini FM, Jones G (2016) Correlates of hip cartilage defects: a cross-sectional study in older adults. J Rhuematol 43(7):1406–1412. https://doi.org/10.3899/jrheum.151001
Ahedi H, Aitken D, Blizzard L, Cicuttini F, Jones G (2020) Quantification of hip effusion-synovitis and its cross-sectional and longitudinal associations with hip pain, MRI findings and early radiographic hip OA. BMC Musculoskelet Disord 21(1):533. https://doi.org/10.1186/s12891-020-03532-7
Kumar D, Wyatt CR, Lee S, Nardo L, Link TM, Majumdar S, Souza RB (2013) Association of cartilage defects, and other MRI findings with pain and function in individuals with mild-moderate radiographic hip osteoarthritis and controls. Osteoarthr Cartil 21(11):1685–1692. https://doi.org/10.1016/j.joca.2013.08.009
Taljanovic MS, Graham AR, Benjamin JB, Gmitro AF, Krupinski EA, Schwartz SA, Hunter TB, Resnick DL (2008) Bone marrow edema pattern in advanced hip osteoarthritis: quantitative assessment with magnetic resonance imaging and correlation with clinical examination, radiographic findings, and histopathology. Skeletal Radiol 37(5):423–431. https://doi.org/10.1007/s00256-008-0446-3
Kijima H, Yamada S, Konishi N, Kubota H, Tazawa H, Tani T, Suzuki N, Kamo K, Okudera Y, Fujii M, Sasaki K, Kawano T, Iwamoto Y, Nagahata I, Miura T, Miyakoshi N, Shimada Y (2020) The differences in imaging findings between painless and painful osteoarthritis of the hip. Clin Med Insights Arthritis Musculoskelet Disorders 13:1179544120946747. https://doi.org/10.1177/1179544120946747
Heerey JJ, Srinivasan R, Agricola R, Smith A, Kemp JL, Pizzari T, King MG, Lawrenson PR, Scholes MJ, Souza RB, Link T, Majumdar S, Crossley KM (2021) Prevalence of early hip OA features on MRI in high-impact athletes. The femoroacetabular impingement and hip osteoarthritis cohort (FORCe) study. Osteoarthr Cartil 29(3):323–334. https://doi.org/10.1016/j.joca.2020.12.013
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O’Connell D, Oxman AD, Phillips B, Schünemann HJ, Edejer T, Varonen H, Vist GE, Williams JW Jr., Zaza S (2004) Grading quality of evidence and strength of recommendations. BMJ (Clinical Res ed) 328(7454):1490. https://doi.org/10.1136/bmj.328.7454.1490
Yusuf E, Kortekaas MC, Watt I, Huizinga TW, Kloppenburg M (2011) Do knee abnormalities visualised on MRI explain knee pain in knee osteoarthritis? A systematic review. Ann Rheum Dis 70(1):60–67. https://doi.org/10.1136/ard.2010.131904
Jaremko JL, Lambert RG, Zubler V, Weber U, Loeuille D, Roemer FW, Cibere J, Pianta M, Gracey D, Conaghan P, Ostergaard M, Maksymowych WP (2014) Methodologies for semiquantitative evaluation of hip osteoarthritis by magnetic resonance imaging: approaches based on the whole organ and focused on active lesions. J Rhuematol 41(2):359–369. https://doi.org/10.3899/jrheum.131082
Acknowledgements
No AI or editing software was employed for writing and editing this manuscript.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This work is supported by the National Natural Science Foundation of China (NSFC, 82103933) and the Scientific Research Level Upgrading Project of Anhui Medical University (2021xkjT006).
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
The guarantor (GC) had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. GC conceived, initiated, and supervised the project. CG, HF and XZ cleaned and analyzed the data. HF, XZ, JW, XX, ZY and GC contributed to the interpretation of the results and writing and revision of the manuscript. All authors gave final approval of the version submitted. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Ethics approval
Inapplicable.
Conflict of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fang, H., Zhang, X., Wang, J. et al. The relationship between MRI-detected hip abnormalities and hip pain in hip osteoarthritis: a systematic review. Rheumatol Int (2024). https://doi.org/10.1007/s00296-024-05678-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00296-024-05678-2