Abstract
The association between spondyloarthritis and cardiovascular (CV) diseases is complex with variable outcomes. This study aimed to assess the prevalence rates of CV diseases and to analyze the impact of CV risk factors on CV disease in patients with spondyloarthritis. A multi-center cross-sectional study using the BioSTAR (Biological and Targeted Synthetic Disease-Modifying Antirheumatic Drugs Registry) database was performed on patients with spondyloarthritis. Socio-demographic, laboratory, and clinical data were collected. Patients with and without major adverse cardiovascular events (MACE) were grouped as Group 1 and Group 2. The primary outcome was the overall group’s prevalence rates of CV disease and CV risk factors. The secondary outcome was the difference in socio-demographic and clinical characteristics between the groups and predictive risk factors for CV disease. There were 1457 patients with a mean age of 45.7 ± 10.9 years. The prevalence rate for CV disease was 3% (n = 44). The distribution of these diseases was coronary artery disease (n = 42), congestive heart failure (n = 4), peripheral vascular disorders (n = 6), and cerebrovascular events (n = 4). Patients in Group 1 were significantly male (p = 0.014) and older than those in Group 2 (p < 0.001). There were significantly more patients with hypertension, diabetes mellitus, chronic renal failure, dyslipidemia, and malignancy in Group 1 than in Group 2 (p < 0.05). Smoking (36.7%), obesity (24.4%), and hypertension (13.8%) were the most prevalent traditional CV risk factors. Hypertension (HR = 3.147, 95% CI 1.461–6.778, p = 0.003), dyslipidemia (HR = 3.476, 95% CI 1.631–7.406, p = 0.001), and cancer history (HR = 5.852, 95% CI 1.189–28.810, p = 0.030) were the independent predictors for CV disease. A multi-center cross-sectional study using the BioSTAR (Biological and Targeted Synthetic Disease-Modifying Antirheumatic Drugs Registry) database was performed on patients with spondyloarthritis. Socio-demographic, laboratory, and clinical data were collected. Patients with and without major adverse cardiovascular events (MACE) were grouped as Group 1 and Group 2. The primary outcome was the overall group’s prevalence rates of CV disease and CV risk factors. The secondary outcome was the difference in socio-demographic and clinical characteristics between the groups and predictive risk factors for CV disease. There were 1457 patients with a mean age of 45.7 ± 10.9 years. The prevalence rate for CV disease was 3% (n = 44). The distribution of these diseases was coronary artery disease (n = 42), congestive heart failure (n = 4), peripheral vascular disorders (n = 6), and cerebrovascular events (n = 4). Patients in Group 1 were significantly male (p = 0.014) and older than those in Group 2 (p < 0.001). There were significantly more patients with hypertension, diabetes mellitus, chronic renal failure, dyslipidemia, and malignancy in Group 1 than in Group 2 (p < 0.05). Smoking (36.7%), obesity (24.4%), and hypertension (13.8%) were the most prevalent traditional CV risk factors. Hypertension (HR = 3.147, 95% CI 1.461–6.778, p = 0.003), dyslipidemia (HR = 3.476, 95% CI 1.631–7.406, p = 0.001), and cancer history (HR = 5.852, 95% CI 1.189–28.810, p = 0.030) were the independent predictors for CV disease. The prevalence rate of CV disease was 3.0% in patients with spondyloarthritis. Hypertension, dyslipidemia, and cancer history were the independent CV risk factors for CV disease in patients with spondyloarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spondyloarthritis (SpA), recognized as a chronic inflammatory condition, encompasses various phenotypes, including ankylosing spondylitis [currently known as radiographic axial SpA (r-axSpA)], non-radiographic axial SpA (nr-axSpA), peripheral SpA, psoriatic arthritis, enteropathic SpA, reactive arthritis, and undifferentiated SpA [1,2,3,4]. While distinct disease characteristics define each SpA phenotype, typical clinical features and comorbidities are frequently observed in SpA patients, prompting the consideration of these diverse conditions as singular disease entities [3].
The association of SpA with cardiovascular (CV) risk factors and major adverse CV events (MACE), such as ischemic heart diseases and cerebrovascular events, has gained popularity for the last decades with conflicting findings [1, 2, 5,6,7]. In SpA patients, a 20–40% increase in CV mortality has been reported compared to the general population [8,9,10]. While certain CV risk factors like age, sex, and family history are non-modifiable, the five primary traditional and modifiable risk factors—hypertension, smoking, dyslipidemia, diabetes, and obesity—account for over 50% of all CV deaths in SpA patients [1, 2, 11, 12]. Therefore, identifying these factors and implementing control measures are crucial in managing the disease and averting morbidity and mortality in SpA patients [1, 13, 14].
Atherosclerosis-related CV events, such as ischemic heart disease, stroke, and myocardial infarction, are the prevalent disease conditions for SpA patients [5, 13,14,15,16]. Studies have indicated a positive correlation between the number of risk factors and the occurrence of CV disease (CVD) [2, 11, 17]. The complex relationship between CV risk factors, treatment approaches, disease-related features, and increased mortality in SpA patients warrants further exploration [1, 5, 11, 13]. Besides the considerable variations in the significance of such relationships for each country, the studies investigating these issues in the same patient groups, including all phenotypes of SpA, are limited in number [1, 9].
The inception of the BioSTAR (Biological and Targeted Synthetic Disease-Modifying Antirheumatic Drugs Registry) database by the Turkish League Against Rheumatism (TLAR) marks a groundbreaking initiative in Turkey, notably aimed at aggregating comprehensive real-life data about chronic conditions like SpA [18]. This nationwide registry stands as a pioneering effort, uniquely positioned to capture the intricate nuances of SpA's trajectory within the Turkish population, offering invaluable insights into its prevalence and prognostic determinants [19, 20]. Moreover, the intrinsic value of long-standing registries transcends mere data collection; they serve as indispensable tools for unraveling a disease's complex trajectory, assessing treatment outcomes, and discerning predictive factors for adverse events, efficacy, and safety of targeted therapeutic strategies [21]. Comprehensive analysis of registry-based cohorts, utilizing the extensive repository of real-world data, aims to uncover and elucidate the precise risk factors linked to CVD in patients with SpA.
This study aimed to assess the prevalence rate of CVD, analyze the demographic and clinical characteristics of SpA patients with and without documented MACEs, and investigate the impact of CV risk factors on the development of CVD in patients with all SpA phenotypes.
Materials and methods
Study
A multi-center cross-sectional study with follow-up data was conducted to investigate the prevalence rates of CVD and CV risk factors in patients with a diagnosis of SpA utilizing the database of the BioSTAR registry [18]. The local ethical committee approved the study (Turkey Medicines and Medical Devices Agency, 66,175,679–514.99–E.6366, and Ankara Numune Training and Research Hospital Ethics Committee, E-182413). Experienced physicians followed up with all patients at 6-month intervals and uploaded the updated clinical information to a predetermined electronic worksheet. All data in this database were evaluated in September 2022 for the current study). The study adhered to the Helsinki Declaration of 1964 principles and its subsequent amendments. All participants gave written informed consent before participating in the BioSTAR–SpA database.
Patients
We included all adult patients (≥ 18 years) with a diagnosis of SpA according to the Assessment of SpondyloArthritis International Society (ASAS) classification criteria [22]. Patients with missing socio-demographic or clinical data were excluded. Comprehensive medical history, physical examination, and laboratory tests were conducted for all patients.
Study variables
Socio-demographic data encompassed age, sex, body mass index (BMI), educational and marital status, smoking and alcohol status, comorbidities, and geographical regions of Turkey where the patients lived. The patients' BMI values were calculated as weight in kilograms divided by the square of height in meters (kg/m2). We categorized the patients with age (< 40 and ≥ 40 years) and BMI (≥ 30 kg/m2 and < 30 kg/m2). Laboratory investigations at the patients' last admission to attending centers were recorded.
The disease-related characteristics of the patients included the disease's duration, the SpA's phenotypes, and HLA B-27 status. The patients were grouped according to the phenotypes of SpA as r-axSpA, nr-axSpA, peripheral SpA, psoriatic arthritis, enteropathic SpA, reactive arthritis, and undifferentiated SpA [1]. The last measured results of the laboratory parameters, including C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), were recorded. The severity of the diseases was evaluated based on the scores of the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI; 1–10) and Ankylosing Spondylitis Disease Activity Score with CRP (ASDAS–CRP). The BASDAI consists of six 10 cm horizontal visual analog scales (VAS) to measure fatigue severity, spinal and peripheral joint pain, localized tenderness, and morning stiffness. The final score has a range of 0–10 [23]. The scores of ≥ 4.0 for BASDAI and ≥ 2.1 for ASDAS–CRP were regarded as high-disease activity [12, 18]. The disease activity indexes and the patient-reported outcomes at the time of the last visit, including ASDAS–ESR, Maastricht Enthesopathy Score (MASES; 1–10), the Bath Ankylosing Spondylitis Functional Index (BASFI; 1–10), the global VAS (1–100) for the patient, the physician, pain, and fatigue, the Disease Activity Index for Psoriatic Arthritis (DAPSA), the Psoriasis Area and Severity Score (PASI), the symptom severity score, fibromyalgia severity score, and tender, and swollen joint counts, were recorded [18, 20, 23,24,25,26,27,28,29].
The MASES score is calculated considering tenderness on 13 enthesis sites, graded from zero (no pain) to three (wince or withdraw). The range is between zero and 39 [18]. A self-assessment instrument with eight questions was used to calculate the BASFI score. The answer to each question corresponded to a 10 cm horizontal VAS with a mean score range from zero to ten [24]. The DAPSA is a composite score calculated with the number of painful and swollen joints, the global VAS for patients (1–10) and pain (1–10), and CRP. Higher scores indicate higher disease activity for psoriatic arthritis [25].
The PASI is a clinician-rated score for psoriasis severity in four anatomic locations (head, upper limbs, trunk, and lower limbs). Depending on the disease severity and surface area involvement, the adjusted total scores ranging from zero to 72 were calculated for each patient. Higher scores indicate more severe psoriatic conditions [26, 27].
The symptom severity score was determined considering fatigue, unrefreshing sleep, cognitive manifestations, and somatic symptoms, assigning from zero (no symptoms) to three (a great deal of symptoms) based on severity or amount. The total score was 12 [28].
The fibromyalgia severity score is calculated by summating the widespread pain index and the symptom severity scores. The range is between zero (no symptoms) and 31 (most severe symptoms). A higher score is regarded as an approximate measure of fibromyalgia severity [29].
The medication use and switching status were searched using the patient's medical files.
Traditional CV risk factors
The medical records of the patients were explicitly searched to ascertain the presence of CV risk factors: (1) dyslipidemia (physician diagnosis, or the use of lipid-lowering medication, or at least one factor: total cholesterol > 200 mg/dL, triglycerides > 150 mg/dL, HDL-cholesterol < 40 mg/dL in men or < 50 mg/dL in women, or LDL-cholesterol > 130 mg/dL), (2) hypertension (physician diagnosis and/or use of anti-hypertensive medications), (3) obesity (BMI ≥ 30 kg/m2), (4) currently active smoking, and (5) diabetes mellitus (physician diagnosis, or glycemia > 126 mg/dL, HbA1c > 6.5%, or glucose-lowering drugs or insulin therapy) [2, 30,31,32].
Groups
The patients were grouped according to the MACE category's proven diagnoses of CV events (Group 1). We used a composite definition of MACE for myocardial infarction, ischemic heart disease, peripheral vascular disorders, congestive heart failure, ischemic stroke, and transient ischemic attack [33, 34]. All these diseases were included in the definition of CVD. Group 2 included patients without MACE.
Statistical analysis
The primary outcome was the prevalence rates of CVD and CV risk factors in patients with SpA. The secondary outcomes were the differences in socio-demographic and clinical characteristics between patients with and without CVD and the identification of the potential risk factors in predicting the development of CVD in the study group.
For descriptive statistics, mean ± standard deviation was used to present continuous data with normal distribution. Median with minimum–maximum values was applied for continuous variables without normal distribution. Numbers and percentages were used for categorical variables. The Shapiro–Wilk and Kolmogorov–Smirnov tests analyzed the normal distribution of the numerical variables.
The ındependent samples t test compared two independent groups where numerical variables had a normal distribution. The Mann–Whitney U test was applied for the variables without normal distribution in comparing two independent groups. The Pearson Chi-square and Fisher's exact tests were used to compare the differences between categorical variables in 2 × 2 tables.
The univariable and multivariable Cox proportional hazard regression models were used to estimate the crude hazard ratios (HRs) and 95% confidence interval (CI) values based on the demographic and clinical variables for the development of the composite MACEs during the duration of the diseases. In these analyses, we categorized for potential confounders: sex, age (< 40 and ≥ 40 years), BMI (< 30 kg/m2/ ≥ 30 kg/m2), smoking and alcohol, diagnosis (others/r-axSpA), BASDAI and ASDAS-CRP (non-high/high risk).
IBM SPSS statistics (version 22.0, IBM Corp., Armonk, NY, USA) was used for statistical analysis. The significance level (p value) was determined at 0.05 in all statistical analyses.
Results
There were 1457 patients with a mean age of 45.7 ± 10.9 years in the study. Most patients (70.1%) were 40 years of age or older. The male-to-female ratio was 2.1 in the study group. The socio-demographic characteristics are given in Table 1.
We found 44 patients (3%) with any MACE during the median disease duration of 126.8 months (Group 1). The distribution of these diseases was coronary artery disease (n = 42), congestive heart failure (n = 4), peripheral vascular disorders (n = 6), and cerebrovascular events (n = 4). The prevalence rates of CVD were 4.7%, 4.3%, 3.2%, and 0.6% in patients with PsA, peripheral SpA, R-axSpa, and Nr-axSpA, respectively. There were significant differences in the age of the patients, the age groups, sex, and alcohol status between the groups (p < 0.05) (Table 1). The patients in Group 1 were significantly older (p < 0.001). No patient was younger than 40 years in Group 1 (p < 0.001). The proportion of male patients was significantly higher in Group 1 than in Group 2 (0.014). There were more patients with current usage of alcohol in Group 1 than in Group 2 (p = 0.009). The other variables were similar in the groups (p > 0.05) (Table 1).
We detected significant differences in the frequencies of the comorbidities between the groups (p < 0.05) (Table 1). Hypertension (n = 201, 13.8%) and diabetes mellitus (n = 105, 7.2%) were the most frequent two diseases in the overall patients. In Group 1, there were significantly more patients with hypertension, diabetes mellitus, chronic renal failure, dyslipidemia, and malignancy than in Group 2 (p < 0.001, p = 0.001, p = 0.001, p < 0.001, and p = 0.018).
In the entire population, smoking (36.7%) and obesity (24.4%) were the most prevalent traditional CV risk factors, followed by hypertension (13.8%) (Table 1).
The disease-related characteristics of the study group are given in Table 2. The median duration of the diseases was significantly higher in Group 1 than in Group 2 (139 months vs. 126.8 months, p = 0.063). In the overall study group, r-axSpA was the most frequent phenotype of SpA seen in 1090 patients (74.8%), followed by nr-axSpA (11.6%). The distribution of the SpA phenotypes was similar in the groups (p = 0.328).
We found no significant differences in the laboratory investigations except triglyceride and glomerular filtration rate (Table 3). The patients in Group 1 had significantly higher triglyceride values and lower glomerular filtration rate values than those in Group 2 (p = 0.010 and p = 0.010). The values of ESR and CRP were similar in the groups (p = 0.532 and p = 0.618).
The disease activity scores are summarized in Table 4. The comparison of the disease severity based on the BASDAI and ASDAS–CRP revealed no significant differences between the groups (p = 0.908 and p = 0.303). The scores for the other scales were similar in the groups, except for DAPSA (p = 0.042).
The medications used to treat the patients are given in Table 5. There was no difference in the patients with drug switches between the groups (p = 0.662).
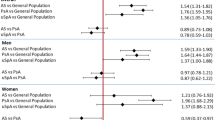
The univariate Cox proportional regression analysis revealed that age, hypertension, diabetes mellitus, dyslipidemia, and cancer history were the significant risk factors for the development of CVD. Nevertheless, the multivariate analysis showed that hypertension (HR = 3.147, 95% CI 1.461–6.778, p = 0.003), dyslipidemia (HR = 3.476, 95% CI 1.631–7.406, p = 0.001), and cancer history (HR = 5.852, 95% CI 1.189–28.810, p = 0.030) were the independent predictors for CVD in the study group (Table 6).
Discussion
This nationwide registry-based study using the BioSTAR database showed that the CVD prevalence rate in SpA patients was 3% within the median disease duration of 126.8 months. Notably, hypertension, dyslipidemia, and a history of cancer emerged as significant risk factors for CVD in this cohort. This research represents one of the pioneering studies analyzing CVD prevalence across all SpA phenotypes within the Turkish population.
The prevalence rates for CVD in patients with inflammatory joint diseases show considerable variances across studies. Yagensky et al. [34] reported prevalence rates of 8.7% and 12.8% for SpA and PsA. Similar rates were reported by the other studies [32, 33, 35, 36]. Interestingly, the prevalence rates in López-Medina’s and Kao's studies were relatively lower than the previously documented rates [1, 6]. In the ASAS–COMOSPA study, the patients from the Mediterranean area had lower CVD rates (1.8% and 1.3% for ischemic heart disease and stroke) than those in Northern European countries (6.2% and 2.5% for ischemic heart disease and stroke), indicating potential regional disparities [1]. Kao et al. [6] highlighted a 2.9% CVD prevalence in newly diagnosed AS patients, suggesting a potential link between increased prevalence and older age or prolonged disease duration [6]. In the current study, the overall prevalence rate for CVD in patients with SpA was 3.0%. The variations in the distribution of SpA phenotypes, geographical areas, and disease activity might be the reasons for such differences. Although older people are more prone to CVD, the possible association of increased disease duration or severity with a higher prevalence of CVD in patients with SpA warrants clarification through prospective studies.
The association between traditional CV risk factors and SpA has been investigated for decades [5, 6]. It is generally believed that SpA patients present with an atherogenic metabolic profile, with chronic systemic inflammation potentially exacerbating both past and future CV events. Notably, indicators of systemic inflammation such as uveitis or elevated CRP levels have been linked to increased CVD in ankylosing spondylitis patients [8, 37, 38]. In that way, these patients might see atherosclerotic events more frequently [6]. However, conflicting outcomes in some studies [39,40,41] underscore methodological differences and patient characteristics, contributing to varied results.
Previous studies have had different prevalence rates of the traditional CV risk factors. In our study, smoking and obesity emerged as prominent risk factors, while other CV risk factors were less prevalent. Similar rates have been reported in the Moroccan population, albeit in a smaller SpA patient cohort [3]. Nevertheless, hypercholesterolemia was the most frequent risk factor seen in more than half of SpA patients [34]. Hypertension was the most common risk factor in almost half of the Norwegian patients with inflammatory joint diseases [35]. In varying prevalence rates from 19.2% to 33.8%, hypertension was seen in patients with different SpA phenotypes in the ASAS–COMOSPA study [1]. Although the prevalence rates of each risk factor have shown considerable variations in each study, socio-demographic, environmental, behavioral, and clinical characteristics might be used to explain such differences [1, 5]. Consequently, assessing data separately within each country or population becomes crucial when evaluating CV risk in SpA patients.
Several authors investigated the reasons for mortality in inflammatory joint diseases, including rheumatoid arthritis, PsA, and axSpA. The authors reported cardiovascular and respiratory diseases as the two leading causes of death in patients with axSpA in the Norwegian Cardio-Rheuma Register [9, 32]. Nevertheless, CARdiovascular in rheuMAtology (CARMA) prospective study showed that patients with SpA were more likely to have an increased risk for CVE. In contrast, the corresponding CV mortality was lower than the estimated rates [32, 33]. The length of follow-up is also a vital factor for detecting more accurate data about mortality. As the duration of follow-up increases, it is expected to see more deaths in aging patients with variable severity of chronic inflammatory joint diseases.
Disease activity has been proposed as a potential risk factor for major adverse CV events (MACEs) in SpA patients, with higher disease activity potentially linked to an increased number of traditional CV risk factors [2, 6]. While our study did not specifically analyze the correlation between the number of CV risk factors and disease characteristics, no significant association was found between disease activity based on BASDAI and ASDAS–CRP groups and CVD development.
The association between drugs and MACEs in SpA patients is another speculative issue [6, 42]. Despite the cardiac toxicities, the antiinflammatory action mechanisms of these medications might attenuate the underlying atherogenic potential and serve the cardioprotection via reducing the disease activity and controlling systemic inflammation for SpA patients with different phenotypes [5, 43, 44]. Nevertheless, the association between the risk of CV mortality and nonsteroidal antiinflammatory drug usage in SpA patients remains controversial [45]. The highly selective COX-2 inhibitors and steroids were the other speculative drugs leading to a higher CVD risk [44]. Kao et al. [6] reported the negative impact of selective COX-2 inhibitors and corticosteroids on developing MACEs in AS patients. However, the results conflicted because of methodological insufficiencies [6]. TNF inhibitors were associated with a reduced risk of CVD according to the retrospective follow-up analysis of 5046 SpA patients [5]. Secukinumab and ixekizumab were the selective IL-17A inhibitors that improved the degree of systemic inflammation without negatively impacting traditional CV risk factors [5, 46, 47]. There were questionable relationships between the targeted synthetic DMARDs and MACE risk in SpA patients [45, 48,49,50]. Based on the systematic reviews and meta-analyses, the evidence that specific types of medications were associated with a higher risk of CVD is still being determined due to methodological problems [41, 44]. We did not analyze the impact of the patient's past and current medication history on the development of CVD, considering the difficulty in collecting data about the quantity of the drugs [2]. The uncertainty regarding the possible interconnections between the disease activity, comorbidities, and the indications for the drugs might influence the results of the previous studies [9, 47]. Although medication adherence was obtained using the patients' medical files or the patient-reported outcomes retrospectively, prospective large-scale studies might be more beneficial for robust conclusions.
Nationwide data about SpA patients with different phenotypes was the main strength of this study. Although the inclusion of all different phenotypes might be regarded as the study's heterogeneity, variability in SpA phenotypes and disease characteristics within the studied population could influence the applicability of our findings to diverse SpA subgroups to understand the overall risk of CVD in this patient group. We also aimed to compare the differences in the prevalence rates of each phenotype. The insufficient number of patients in some phenotypes prevented such comparisons. Besides, due to the study's cross-sectional design, we could not discriminate whether CVD was present before or after the diagnosis of SpA.
The cross-sectional nature of our study restricted our ability to establish the temporal sequence between the onset of CVD and the diagnosis of SpA, which is the study's major limitation. In that way, CVD occurrences predated or followed the diagnosis of SpA, the complex interplay between disease-specific factors, limitations inherent in the dataset, and the potential influence of unmeasured confounders or variables not included or analyzed in the study.
Another limitation might be the potential underestimation of CVD prevalence due to the likelihood of subclinical cases and unregistered hospital admissions.
In conclusion, this nationwide, cross-sectional registry study revealed that CVD risk in patients with SpA was relatively low compared to the previous rates. Among the traditional CV risk factors, hypertension and dyslipidemia were the independent predictive factors for the development of CVD. Besides, cancer history was another independent risk factor for CVD. Large-scale, prospective studies are needed to clarify the controversial issues in predicting CVD risk.
References
López-Medina C, Jiménez-Gómez Y, Moltó A, Schiotis RE, Marzo-Ortega H, van Gaalen FA, Ozgocmen S, Dougados M, Calvo-Gutiérrez J, Castro-Villegas MC, Collantes-Estévez E, Font-Ugalde P, ASAS-COMOSPA Task Force (2018) Cardiovascular risk factors in patients with spondyloarthritis from Northern European and Mediterranean countries: an ancillary study of the ASAS-COMOSPA project. Jt Bone Spine 85(4):447–453. https://doi.org/10.1016/j.jbspin.2017.07.006
Ferraz-Amaro I, Rueda-Gotor J, Genre F, Corrales A, Blanco R, Portilla V, González Mazón I, Llorca J, Expósito R, Vicente EF, Quevedo-Abeledo JC, Rodríguez-Lozano C, Ortega-Castro R, Ladehesa-Pineda ML, Fernández-Carballido C, Martínez-Vidal MP, Castro-Corredor D, Anino-Fernández J, García Vivar ML, Galíndez-Agirregoikoa E, Peiteado D, Plasencia-Rodríguez C, Montes Perez E, Fernández Díaz C, Castañeda S, González-Gay MÁ (2021) Potential relation of cardiovascular risk factors to disease activity in patients with axial spondyloarthritis. Ther Adv Musculoskelet Dis. https://doi.org/10.1177/1759720X211033755
Eddarami J, Azzouzi H, Ichchou L (2021) Heart ınvolvement in a moroccan population with spondyloarthritis: a cross-sectional study. J Saudi Heart Assoc 33(2):191–197. https://doi.org/10.37616/2212-5043.1258
Ladehesa-Pineda ML, Arias de la Rosa I, López Medina C, Castro-Villegas MDC, Ábalos-Aguilera MDC, Ortega-Castro R, Gómez-García I, Seguí-Azpilcueta P, Jiménez-Gómez Y, Escudero-Contreras A, López Pedrera C, Barbarroja N, Collantes-Estévez E, CASTRO Working Group (2020) Assessment of the relationship between estimated cardiovascular risk and structural damage in patients with axial spondyloarthritis. Ther Adv Musculoskelet Dis. https://doi.org/10.1177/1759720X20982837
Chan SCW, Teo CK, Li PH, Lau KK, Lau CS, Chung HY (2021) Cardiovascular risk in patients with spondyloarthritis and association with anti-TNF drugs. Ther Adv Musculoskelet Dis. https://doi.org/10.1177/1759720X211032444
Kao CM, Wang JS, Ho WL, Ko TM, Chen HM, Lin CH, Huang WN, Chen YH, Chen HH (2022) Factors associated with the risk of major adverse cardiovascular events in patients with ankylosing spondylitis: a nationwide, population-based case-control study. Int J Environ Res Public Health 19(7):4098. https://doi.org/10.3390/ijerph19074098
Atzeni F, Popa CD, Nucera V, Nurmohamed MT (2022) Safety of JAK inhibitors: focus on cardiovascular and thromboembolic events. Expert Rev Clin Immunol 18(3):233–244. https://doi.org/10.1080/1744666X.2022.2039630
Kelty E, Ognjenovic M, Raymond WD, Inderjeeth CA, Keen HI, Preen DB, Nossent JC (2022) Mortality rates in patients with ankylosing spondylitis with and without extraarticular manifestations and comorbidities: a retrospective cohort study. J Rheumatol 49(7):688–693. https://doi.org/10.3899/jrheum.210909
Kerola AM, Kazemi A, Rollefstad S, Lillegraven S, Sexton J, Wibetoe G, Haavardsholm EA, Kvien TK, Semb AG (2022) All-cause and cause-specific mortality in rheumatoid arthritis, psoriatic arthritis and axial spondyloarthritis: a nationwide registry study. Rheumatology (Oxford) 4:keac210. https://doi.org/10.1093/rheumatology/keac210
Södergren A, Askling J, Bengtsson K, Forsblad-d’Elia H, Jernberg T, Lindström U, Ljung L, Mantel Ä, Jacobsson LTH (2021) Characteristics and outcome of a first acute myocardial infarction in patients with ankylosing spondylitis. Clin Rheumatol 40(4):1321–1329. https://doi.org/10.1007/s10067-020-05354-3
Ferraz-Amaro I, Prieto-Peña D, Palmou-Fontana N, Martínez-López D, de Armas-Rillo L, García-Dorta A, Atienza-Mateo B, Blanco R, Armesto S, González-Gay MÁ (2020) The number of traditional cardiovascular risk factors ıs ındependently correlated with disease activity in patients with psoriatic arthritis. Medicina (Kaunas) 56(8):415. https://doi.org/10.3390/medicina56080415
Chen CH, Chen HA, Liu CH, Liao HT, Chou CT, Chen CH (2020) Association of obesity with inflammation, disease severity and cardiovascular risk factors among patients with ankylosing spondylitis. Int J Rheum Dis 23(9):1165–1174. https://doi.org/10.1111/1756-185X.13912
Rueda-Gotor J, Ferraz-Amaro I, Genre F, González-Mazón I, Corrales A, Calvo-Rio V, Portilla V, Llorca J, Expósito R, Hernández-Hernández V, Quevedo-Abeledo JC, Rodríguez-Lozano C, Lopez-Medina C, Ladehesa-Pineda ML, Castañeda S, Vicente EF, Fernández-Carballido C, Martínez-Vidal MP, Castro-Corredor D, Anino-Fernández J, Peiteado D, Plasencia-Rodríguez C, García-Vivar ML, Galíndez-Agirregoikoa E, Montes-Perez E, Fernández-Díaz C, Blanco R, González-Gay MÁ (2022) Factors associated with atherosclerosis in radiographic and non-radiographic axial spondyloarthritis. A multicenter study on 838 patients. Semin Arthritis Rheum 55:152037. https://doi.org/10.1016/j.semarthrit.2022.152037
González Mazón I, Rueda-Gotor J, Ferraz-Amaro I, Genre F, Corrales A, Calvo Rio V, Palmou Fontana N, Portilla V, Llorca J, Mata C, Hernández-Hernández V, Quevedo-Abeledo JC, Rodríguez-Lozano C, Lopez Medina C, Ladehesa-Pineda ML, Castañeda S, Vicente EF, Fernández-Carballido C, Martínez-Vidal MP, Castro-Corredor D, Anino-Fernández J, Peiteado D, Plasencia-Rodríguez C, García-Vivar ML, Galíndez-Agirregoikoa E, Montes Perez E, Fernández Díaz C, Blanco R, González-Gay MA (2021) Subclinical atherosclerotic disease in ankylosing spondylitis and non-radiographic axial spondyloarthritis. A multicenter study on 806 patients. Semin Arthritis Rheum 51(2):395–403. https://doi.org/10.1016/j.semarthrit.2021.02.003
Kim JH, Choi IA (2021) Cardiovascular morbidity and mortality in patients with spondyloarthritis: a meta-analysis. Int J Rheum Dis 24(4):477–486. https://doi.org/10.1111/1756-185X.13970
Mathieu S, Soubrier M (2019) Cardiovascular events in ankylosing spondylitis: a 2018 meta-analysis. Ann Rheum Dis 78(6):e57. https://doi.org/10.1136/annrheumdis-2018-213317
Yang ZJ, Liu J, Ge JP, Chen L, Zhao ZG, Yang WY, China National Diabetes and Metabolic Disorders Study Group (2012) Prevalence of cardiovascular disease risk factor in the Chinese population: the 2007–2008 China National Diabetes and Metabolic Disorders Study. Eur Heart J 33(2):213–220. https://doi.org/10.1093/eurheartj/ehr205
Bodur H, Yurdakul FG, Ataman S, Cay HF, Gurer G, Capkin E, Sezer İ, Duruoz MT, Melikoglu MA, Rezvani A, Yagci I, Gogus F, Kamanli A, Akgul O, Cevik R (2022) Where we are in treat to target era? Predictive factors for remission and drug switching in patients with axial spondyloarthritis: a real-life evidence from BioStaR nationwide registry. Clin Rheumatol 41(7):2053–2063. https://doi.org/10.1007/s10067-022-06145-8
Fitzgerald G, Gallagher P, O’Shea FD (2020) multimorbidity in axial spondyloarthropathy and its association with disease outcomes: results from the Ankylosing Spondylitis Registry of Ireland Cohort. J Rheumatol 47(2):218–226. https://doi.org/10.3899/jrheum.181415
Akgul O, Bodur H, Ataman S, Yurdakul FG, Capkin E, Gurer G, Sezer I, Duruoz MT, Melikoglu MA, Cay HF, Rezvani A, Yagci I, Gogus F, Kamanli A, Cevik R (2020) Clinical performance of ASAS Health Index in patients with ankylosing spondylitis and non-radiographic axial spondyloarthritis: real-world evidence from Multicenter Nationwide Registry. Rheumatol Int 40(11):1793–1801. https://doi.org/10.1007/s00296-020-04680-8
Önen F, Can G, Çapar S, Dalkılıç E, Pehlivan Y, Şenel S, Akar S, Koca SS, Tufan A, Yazıcı A, Yılmaz S, İnanç N, Sarı İ, Birlik M, Solmaz D, Cefle A, Öztürk MA, Yolbaş S, Krogh NS, Yılmaz N, Erten Ş, Bes C, Gündüz ÖS, Göker B, Haznedaroğlu S, Yavuz Ş, Yildirim Çetin G, Yıldız F, Direskeneli H, Akkoç N (2022) A real-life analysis of patients with rheumatologic diseases on biological treatments: data from TURKBIO Registry. Eur J Rheumatol 9(2):82–87. https://doi.org/10.5152/eurjrheum.2022.21060
Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J, Braun J, Chou CT, Collantes-Estevez E, Dougados M, Huang F, Gu J, Khan MA, Kirazli Y, Maksymowych WP, Mielants H, Sørensen IJ, Ozgocmen S, Roussou E, Valle-Oñate R, Weber U, Wei J, Sieper J (2009) The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 68(6):777–783. https://doi.org/10.1136/ard.2009.108233. (Erratum in: Ann Rheum Dis. 2019 Jun; 78(6): e59)
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A (1994) A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 21(12):2286–2291
Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P, Jenkinson T (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 21(12):2281–2285
Gonçalves RSG, de Almeida Martins LM, de Ataide MH, Dantas AT, Duarte ALBP (2020) DAPSA versus cDAPSA: do we need to use CRP? Ann Rheum Dis 79(11):e142. https://doi.org/10.1136/annrheumdis-2019-215960
Matza LS, Brazier JE, Stewart KD, Pinto L, Bender RH, Kircik L, Jordan J, Kim KJ, Mutebi A, Viswanathan HN, Menter A (2019) Developing a preference-based utility scoring algorithm for the psoriasis area severity index (PASI). J Med Econ 22(9):936–944. https://doi.org/10.1080/13696998.2019.1627362
Keskin Y, Nas K, Kiliç E, Sargin B, Acer Kasman S, Alkan H, Şahin N, Cengiz G, Cuzdan N, Albayrak Gezer İ, Keskin D, Mülkoğlu C, Resorlu H, Ataman Ş, Bal A, Duruoz MT, Küçükakkas O, Yurdakul OV, Alkan Melikoğlu M, Aydin Y, Ayhan FF, Bodur H, Çaliş M, Çapkin E, Devrimsel G, Gök K, Hizmetli S, Kamanli A, Ecesoy H, Kutluk Ö, Şen N, Şendur ÖF, Tekeoğlu İ, Tolu S, Toprak M, Tuncer T (2020) Clinical characteristics, disease activity, functional status, and quality of life results of patients with psoriatic arthritis using biological and conventional synthetic disease-modifying antirheumatic drugs. Arch Rheumatol 36(1):1–9. https://doi.org/10.46497/ArchRheumatol.2021.7874
Moyano S, Kilstein JG, Alegre de Miguel C (2015) New diagnostic criteria for fibromyalgia: here to stay? Reumatol Clin 11(4):210–214. https://doi.org/10.1016/j.reuma.2014.07.008
Latifoglou E, Çınar E, Tanıgör G, On AY (2023) Coexistence of fibromyalgia and post-polio syndrome in persons with prior poliomyelitis in Turkey: the relations with symptoms, polio-related impairments, and quality of life. Disabil Rehabil 45(21):3511–3518. https://doi.org/10.1080/09638288.2022.2127931
Schwartz DM, Parel P, Li H, Sorokin AV, Berg AR, Chen M, Dey A, Hong CG, Playford M, Sylvester M, Teague H, Siegel E, Mehta NN (2022) PET/CT-based characterization of 18F-FDG uptake in various tissues reveals novel potential contributions to coronary artery disease in psoriatic arthritis. Front Immunol 13:909760. https://doi.org/10.3389/fimmu.2022.909760
Landgren AJ, Dehlin M, Jacobsson L, Bergsten U, Klingberg E (2021) Cardiovascular risk factors in gout, psoriatic arthritis, rheumatoid arthritis and ankylosing spondylitis: a cross-sectional survey of patients in Western Sweden. RMD Open 7(2):e001568. https://doi.org/10.1136/rmdopen-2021-001568
Martín-Martínez MA, Castañeda S, Sánchez-Alonso F, García-Gómez C, González-Juanatey C, Sánchez-Costa JT, Belmonte-López MA, Tornero-Molina J, Santos-Rey J, Sánchez González CO, Quesada E, Moreno-Gil MP, Cobo-Ibáñez T, Pinto-Tasnde JA, Babío-Herráez J, Bonilla G, Juan-Mas A, Manero-Ruiz FJ, Romera-Baurés M, Bachiller-Corral J, Chamizo-Carmona E, Uriarte-Ecenarro M, Barbadillo C, Fernández-Carballido C, Aurrecoechea E, Möller-Parrera I, Llorca J, González-Gay MA, CARMA Project Collaborative Group (2021) Cardiovascular mortality and cardiovascular event rates in patients with inflammatory rheumatic diseases in the CARdiovascular in rheuMAtology (CARMA) prospective study-results at 5 years of follow-up. Rheumatology (Oxford) 60(6):2906–2915. https://doi.org/10.1093/rheumatology/keaa737
Shi LH, Lam SH, So H, Li EK, Li TK, Szeto CC, Tam LS (2022) High inflammatory burden predicts cardiovascular events in patients with axial spondyloarthritis: a long-term follow-up study. Ther Adv Musculoskelet Dis. https://doi.org/10.1177/1759720X221122401
Yagensky V, Schirmer M (2022) Cardiovascular risks and risk stratification in inflammatory joint diseases: a cross-sectional study. Front Med (Lausanne) 9:786776. https://doi.org/10.3389/fmed.2022.786776
Wibetoe G, Ikdahl E, Rollefstad S, Olsen IC, Bergsmark K, Kvien TK, Salberg A, Soldal DM, Bakland G, Lexberg Å, Fevang BT, Gulseth HC, Haugeberg G, Semb AG (2017) Cardiovascular disease risk profiles in inflammatory joint disease entities. Arthritis Res Ther 19(1):153. https://doi.org/10.1186/s13075-017-1358-1
Castañeda S, Martín-Martínez MA, González-Juanatey C, Llorca J, García-Yébenes MJ, Pérez-Vicente S, Sánchez-Costa JT, Díaz-Gonzalez F, González-Gay MA (2015) Cardiovascular morbidity and associated risk factors in Spanish patients with chronic inflammatory rheumatic diseases attending rheumatology clinics: baseline data of the CARMA Project. Semin Arthritis Rheum 44(6):618–626. https://doi.org/10.1016/j.semarthrit.2014.12.002. (Erratum in: Semin Arthritis Rheum. 2015 Oct; 45(2):e7–8)
Lai YF, Lin TY, Chien WC, Sun CA, Chung CH, Chen YH, Chen JT, Chen CL (2022) Uveitis as a risk factor for developing acute myocardial infarction in ankylosing spondylitis: a national population-based longitudinal cohort study. Front Immunol 11(12):811664. https://doi.org/10.3389/fimmu.2021.811664
Feng KM, Chien WC, Chen YH, Sun CA, Chung CH, Chen JT, Chen CL (2022) Increased risk of acute coronary syndrome in ankylosing spondylitis patients with uveitis: a population-based cohort study. Front Immunol 10(13):890543. https://doi.org/10.3389/fimmu.2022.890543
Liew JW, Reveille JD, Castillo M, Sawhney H, Naovarat BS, Heckbert SR, Gensler LS (2021) Cardiovascular risk scores in axial spondyloarthritis versus the general population: a cross-sectional study. J Rheumatol 48(3):361–366. https://doi.org/10.3899/jrheum.200188
Brophy S, Cooksey R, Atkinson M, Zhou SM, Husain MJ, Macey S, Rahman MA, Siebert S (2012) No increased rate of acute myocardial infarction or stroke among patients with ankylosing spondylitis—a retrospective cohort study using routine data. Semin Arthritis Rheum 42(2):140–145. https://doi.org/10.1016/j.semarthrit.2012.02.008
Schieir O, Tosevski C, Glazier RH, Hogg-Johnson S, Badley EM (2017) Incident myocardial infarction associated with major types of arthritis in the general population: a systematic review and meta-analysis. Ann Rheum Dis 76(8):1396–1404. https://doi.org/10.1136/annrheumdis-2016-210275
Karmacharya P, Shahukhal R, Crowson CS, Murad MH, Davis JM 3rd, Shrestha P, Bekele D, Wright K, Chakradhar R, Dubreuil M (2020) Effects of therapies on cardiovascular events in ankylosing spondylitis: a systematic review and meta-analysis. Rheumatol Ther 7(4):993–1009. https://doi.org/10.1007/s40744-020-00248-x
Persson R, Hagberg KW, Qian Y, Vasilakis-Scaramozza C, Jick S (2021) The risks of major cardiac events among patients with psoriatic arthritis treated with apremilast, biologics, DMARDs or corticosteroids. Rheumatology (Oxford) 60(4):1926–1931. https://doi.org/10.1093/rheumatology/keaa683
Bodur H (2023) Cardiovascular comorbidities in spondyloarthritis. Clin Rheumatol 42(10):2611–2620. https://doi.org/10.1007/s10067-022-06473-9
Toussirot E (2021) The risk of cardiovascular diseases in axial spondyloarthritis. Current insights. Front Med (Lausanne) 8:782150. https://doi.org/10.3389/fmed.2021.782150
Merola JF, McInnes IB, Deodhar AA, Dey AK, Adamstein NH, Quebe-Fehling E, Aassi M, Peine M, Mehta NN (2022) Effect of secukinumab on traditional cardiovascular risk factors and inflammatory biomarkers: post hoc analyses of pooled data across three indications. Rheumatol Ther 9(3):935–955. https://doi.org/10.1007/s40744-022-00434-z
Kwon OC, Park MC (2022) Effect of tumor necrosis factor inhibitors on risk of cardiovascular disease in patients with axial spondyloarthritis. Arthritis Res Ther 24(1):141. https://doi.org/10.1186/s13075-022-02836-4
van der Heijde D, Song IH, Pangan AL, Deodhar A, van den Bosch F, Maksymowych WP, Kim TH, Kishimoto M, Everding A, Sui Y, Wang X, Chu AD, Sieper J (2019) Efficacy and safety of upadacitinib in patients with active ankylosing spondylitis (SELECT-AXIS 1): a multicentre, randomised, double-blind, placebo-controlled, phase 2/3 trial. Lancet 394(10214):2108–2117. https://doi.org/10.1016/S0140-6736(19)32534-6
McInnes IB, Kato K, Magrey M, Merola JF, Kishimoto M, Pacheco-Tena C, Haaland D, Chen L, Duan Y, Zueger P, Liu J, Lippe R, Pangan AL, Behrens F (2021) Upadacitinib in patients with psoriatic arthritis and an inadequate response to non-biological therapy: 56-week data from the phase 3 SELECT-PsA 1 study. RMD Open 7(3):e001838. https://doi.org/10.1136/rmdopen-2021-001838. (Erratum in: RMD Open. 2021 Nov; 7(3))
Deodhar A, Van den Bosch F, Poddubnyy D, Maksymowych WP, van der Heijde D, Kim TH, Kishimoto M, Blanco R, Duan Y, Li Y, Pangan AL, Wung P, Song IH (2022) Upadacitinib for the treatment of active non-radiographic axial spondyloarthritis (SELECT-AXIS 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 400(10349):369–379. https://doi.org/10.1016/S0140-6736(22)01212-0
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK). This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Consent to participate
Informed consent was obtained from all subjects before enrollment.
Consent for publication
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duruöz, M.T., Bodur, H., Ataman, Ş. et al. Cross-sectional analysis of cardiovascular disease and risk factors in patients with spondyloarthritis: a real-life evidence from biostar nationwide registry. Rheumatol Int 44, 631–642 (2024). https://doi.org/10.1007/s00296-023-05523-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-023-05523-y