Abstract
To investigate factors associated with fulfilment of expectations towards paid employment after total hip/knee arthroplasty (THA/TKA). Cohort study including preoperatively employed patients aged 18–64 scheduled for THA/TKA. Expectations were collected preoperatively, and 6 and 12 months postoperatively with the paid employment item of the Hospital-for-Special-Surgery Expectations Surveys (back-to-normal = 1; large improvement = 2; moderate improvement = 3; slight improvement = 4; not applicable = 5). Patients scoring not applicable were excluded. Fulfilment was calculated by subtracting preoperative from postoperative scores (< 0: unfulfilled; ≥ 0: fulfilled). Multivariable logistic regression analyses were conducted separately for THA/TKA at 6 and 12 months postoperatively. Six months postoperatively, 75% of THA patients (n = 237/n = 316) and 72% of TKA patients (n = 211/n = 294) had fulfilled expectations. Older age (TKA:OR 1.08, 95% CI 1.01–1.15) and better postoperative physical functioning (THA:OR 1.10, 95% CI 1.06–1.14; TKA:OR 1.03, 95% CI 1.01–1.06) increased the likelihood of fulfilment. Physical work tasks (THA:OR 0.12, 95% CI 0.03–0.44), preoperative sick leave (TKA:OR 0.33, 95% CI 0.17–0.65), and difficulties at work (THA:OR 0.10, 95% CI 0.03–0.35; TKA:OR 0.41, 95% CI 0.17–0.98) decreased the likelihood of fulfilment. Twelve months postoperatively similar risk factors were found. Three out of four working-age THA/TKA patients had fulfilled expectations towards paid employment at 6 months postoperatively. Preoperative factors associated with fulfilment were older age, mental work tasks, no sick leave, postoperative factors were better physical functioning, and no perceived difficulties at work.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Work is a key element of participation and an important determinant of general health, well-being, and quality of life [1]. Studies measuring work-related outcomes have mainly examined first-time return to work (RTW) [2,3,4], and found that RTW rates varied between 25 and 122% after total hip arthroplasty (THA) and 40–98% after total knee arthroplasty (TKA) within 1–2 years postoperatively [2, 3]. RTW is an important treatment goal for an expanding group of patients undergoing a THA or TKA [2, 3, 5], as 45% of THA and 49% of TKA patients in the Netherlands are of working age [6]. Similar trends are seen in other Western countries [7, 8]. Patients are also confident in reaching this goal, as patients of working-age tend to have high expectations about (returning to) work [5, 9].
Although patient expectations towards paid employment after THA or TKA are high, 11–43% of patients have unfulfilled expectations [9,10,11,12]. The few studies investigating fulfilment of expectations among THA or TKA patients suggest that expectations towards paid employment are among the least fulfilled [10, 11]. However, as these studies did not focus on working-age patients [10,11,12], uncertainties remain about such expectation fulfilment. Moreover, research investigating factors solely associated with fulfilment towards paid employment is so far lacking. The existing studies only incorporate fulfilment towards paid employment as one of multiple factors in their total fulfilment scores [10, 11]. Investigating which factors influence fulfilment of expectations towards paid employment will aid in the design of future target strategies to appropriately address those prone to unfulfillment.
Looking beyond the first time of RTW and focussing on fulfilment of patient expectations towards paid employment is important to gain better understanding of preoperative and postoperative factors associated with a successful RTW process. Therefore, the aim of this study was to identify factors associated with fulfilment of patient expectations towards paid employment for THA or TKA patients at both 6 and 12 months postoperatively. Potential factors include sociodemographic and preoperative/postoperative health- and work-related factors that have previously been linked to RTW [2, 3, 13]. We focussed on fulfilment of expectations towards paid employment at both 6 and 12 months postoperatively, as previous studies indicated that general recovery and recovery of work participation occurs between 6 and 12 months postoperatively [14, 15].
Methods
Design and procedure
The study was part of the “Longitudinal Leiden Orthopaedics Outcomes of Osteoarthritis Study” (LOAS), an ongoing, multicentre cohort study [16, 17]. Data collection started in 2012 and patients were recruited at the orthopaedic departments of eight Dutch medical centres (one university hospital and seven regional hospitals). Informed consent was obtained from all patients prior to the study in conformity with the Declaration of Helsinki [18]. For the current study we used data collected preoperatively and at 6 and 12 months postoperatively between 2012 and 2018. Ethical approval was obtained from the Medical Ethics Committee of Leiden University Medical Center (registration no. P12.047; Trial ID NTR3348).
Population
General inclusion criteria for the LOAS were a diagnosis of osteoarthritis, age 18 or older, being listed for THA/TKA, and sufficient Dutch-language skills to complete the questionnaires. For the current study we selected a subgroup: patients preoperatively employed, aged 18–64, listed for primary THA or TKA, and who completed the preoperative and postoperative item on paid employment.
Measures
Sociodemographic factors
Data were collected preoperatively for the following sociodemographic factors: age (years), sex, and living status (with/without partner).
Health-related factors
Health-related factors were gathered by inquiring about body mass index (BMI), comorbidities, ASA-classification, self-reported physical functioning, and health-related quality of life. BMI was derived from preoperative self-reported body height and weight. Comorbidities were measured preoperatively using a 19-item chronic conditions questionnaire developed by the Dutch Central Bureau of Statistics [19]. Comorbidities were categorized as musculoskeletal or non-musculoskeletal (yes/no) [16, 20]. Self-reported osteoarthritis related physical functioning was measured both preoperatively and postoperatively with the validated Hip/Knee Osteoarthritis Outcome Score-Physical function Short form (HOOS-PS/KOOS-PS) [21,22,23]. The HOOS-PS consists of five items and the KOOS-PS consists of seven items (scale 0–100, higher scores indicating better perceived functioning). Health-related quality of life was measured preoperatively with the Short Form-12 Mental and Physical Component Summary (SF-12 MCS/SF-12 PCS, scale 0–100, higher scores indicating a better health-related quality of life) [24].
Work-related factors
Work-related factors, preoperatively collected, were self-employment (yes/no), working hours (h), type of tasks (physical/mental/combination), sick leave one month preoperatively due to hip/knee complaints (yes/no), and expected time to RTW (weeks). Actual time to RTW (weeks) was collected postoperatively. Difficulties at work caused by hip/knee complaints (yes/no) were measured both preoperatively and postoperatively.
Preoperative expectations and postoperative fulfilment of expectations towards paid employment
Preoperative expectations towards paid employment were measured using a single question from the validated Hospital for Special Surgery (HSS) hip/knee replacement expectations survey, translated into Dutch [25]. The HSS is an 18-item (THA) or 17-item (TKA) self-administered survey, measuring expectations in the domains of pain, function, activities, and psychological wellbeing. We focused on the “What are your expectations towards paid employment after surgery” item. On a Likert scale, five options were possible: 1 (back to normal), 2 (large improvement), 3 (moderate improvement), 4 (slight improvement), 5 (does not apply). For baseline characteristics of the study population (Table 1), we divided preoperative expectations into “back to normal” (score 1) and “not back to normal” (score 2–4). Patients answering not applicable (score 5) were excluded from the study.
Postoperative fulfilment of expectations towards paid employment was used as primary outcome measure. To measure expectation fulfilment, the preoperative HSS questionnaire was modified for use in the LOAS and was composed of the same 5-point Likert scale. The heading of the questionnaire was the only difference: asking to report the “actual status” of the function/activities. Patients were not reminded of their preoperative responses. Postoperative fulfilment of expectations was measured after 6 and 12 months. Fulfilment of expectations was calculated by subtracting preoperative from postoperative HSS scores (≤ – 1: unfulfilled; 0: fulfilled, ≥ 1: exceeded).
Statistical analyses
Descriptive statistics (mean (SD), n (%)) were used to describe baseline characteristics, for preoperative expectations (“back to normal”, “not back to normal”), separately for THA and TKA patients. Postoperative expectation fulfilment was dichotomized (“unfulfilled” and “fulfilled/exceeded”). The “fulfilled” and “exceeded” groups were combined because the “exceeded” group was very small. Analyses were conducted for fulfilment at both 6 and 12 months postoperatively. The characteristics of patients with unfulfilled and fulfilled expectations were compared using Pearson’s chi-square tests (nominal categorical variables), independent T tests (continuous variables), and chi-square trend tests (ordinal categorical variables; Tables S1 and S2).
To select covariates in the multivariate logistic regression, we performed an univariate test on age, sex, comorbidities, preoperative HOOS-PS/KOOS-PS, postoperative HOOS-PS/KOOS-PS, work tasks, preoperative sick leave and postoperative difficulties at work due to hip or knee complaints (Table S3 and S4). All variables with a p value ≤ 0.15 in the univariate analyses were included in the multivariable regression analyses [26]. Variables were omitted via backward selection, depending on their level of statistical significance (p < 0.05). Preoperative patient expectation was included as control variable. Odds ratios were calculated, including 95% confidence intervals (Tables 3 and 5). All analyses were stratified for THA and TKA. IBM Statistical Package for the Social Sciences (SPSS) version 25.0 was used for analyses.
Results
In total, 1056 working-age patients (n = 582 THA, n = 474 TKA) were eligible. Patients answering “not applicable” to the preoperative (n = 128 THA; n = 88 TKA) or postoperative expectation question were excluded (6 months postoperatively: n = 53 THA; n = 30 TKA; 12 months postoperatively: n = 54 THA; n = 34 TKA). The majority of these excluded patients were male (60%) and performed mainly mental work tasks (50%). Eventually, n = 368 THA and n = 326 TKA patients were included. Figure 1 shows a flowchart of the study enrolment and follow-up. Baseline characteristics of the study sample are presented in Table 1.
Flowchart study enrolment and follow-up. *From n = 29 THA and n = 36 TKA patients data at 6 months postoperatively was missing, but data at 12 months postoperatively was available. THA total hip arthroplasty, TKA total knee arthroplasty, LOAS Longitudinal Leiden Orthopaedics Outcomes of Osteoarthritis Study, NA not applicable
Baseline characteristics of THA patients
The THA group consisted of 49% females, mean age 57 years (SD 7). Preoperatively, 94% (n = 345) expected a “back to normal” and 6% (n = 23) expected a “not back to normal” paid employment.
Baseline characteristics of TKA patients
The TKA group consisted of 56% females, mean age 58 years (SD 5). Preoperatively, 84% (n = 275) expected a “back to normal” and 16% (n = 51) expected a “not back to normal” paid employment.
Expectation fulfilment of THA patients
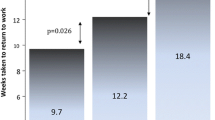
Six months postoperatively, 75% (n = 237) of patients had fulfilled expectations and 3% (n = 7) of them exceeded their expectations, increasing 12 months postoperatively to 83% (n = 239) and 4% (n = 10), respectively. Six months postoperatively, 82% of patients with unfulfilled and 96% of patients with fulfilled expectations actually returned to work, increasing 12 months postoperatively to 88% and 98%, respectively. Preoperatively, mean expected time to RTW was 11 weeks for patients with unfulfilled and 7 weeks for patients with fulfilled expectations. Actual mean time to RTW was 12 weeks for patients with unfulfilled and 9 weeks for patients with fulfilled expectations.
Potential risk factors stratified for fulfilment are shown in Tables S1 and S2. Six months postoperatively, five factors were below the cut-off value in the univariate analyses and were therefore used in the multivariate analyses (preoperative HOOS-PS, postoperative HOOS-PS, work tasks, preoperative sick leave, postoperative difficulties at work due to hip complaints; Table S3). Better postoperative physical functioning (HOOS-PS) scores increased the likelihood of fulfilment at 6 months postoperatively (OR 1.10, 95% CI 1.06–1.14). Physical work tasks (reported in 23%; OR 0.12, 95% CI 0.03–0.44) and postoperative difficulties at work due to hip complaints (reported in 41%; OR 0.10, 95% CI 0.03–0.35) decreased the likelihood of fulfilment (Table 2).
Twelve months postoperatively, seven factors were below the cut-off value in the univariate analyses (age, musculoskeletal comorbidity, preoperative HOOS-PS, postoperative HOOS-PS, work tasks, preoperative sick leave, postoperative difficulties at work due to hip complaints; Table S4). Higher age (OR 1.08, 95% CI 1.02–1.15) and better postoperative physical functioning (OR 1.11, 95% CI 1.07–1.14) increased the likelihood of fulfilment. Physical work tasks (OR 0.15, 95% CI 0.04–0.60) and a combination of work tasks (OR 0.14, 95% CI 0.04–0.46) decreased the likelihood of fulfilment (Table 3). Sensitivity analyses showed that a lower proportion of patients aged ≤ 55 had fulfilled expectations compared to those aged ≥ 56.
Expectation fulfilment of TKA patients
Six months postoperatively, 72% (n = 211) of patients had fulfilled expectations, with 8% (n = 17) exceeding their expectations; this percentage increased to 79% (n = 204) and 9% (n = 18), respectively, at 12 months postoperatively. Six months postoperatively, 81% of patients with unfulfilled and 95% of patients with fulfilled expectations actually returned to work, increasing 12 months postoperatively to 85% and 98%, respectively. Preoperatively, mean expected time to RTW was 11 weeks for patients with unfulfilled and 9 weeks for patients with fulfilled expectations. Actual mean time to RTW was 13 weeks for patients with unfulfilled and 11 weeks for patients with fulfilled expectations.
Potential risk factors stratified for fulfilment are shown in Tables S1 and S2. Six months postoperatively, seven factors were below the cut-off value in the univariate analyses and therefore used in the multivariate analyses (age, musculoskeletal comorbidity, preoperative KOOS-PS, postoperative KOOS-PS, work tasks, preoperative sick leave, postoperative difficulties at work due to knee complaints; Table S3). Higher age (OR 1.08, 95% CI 1.01–1.15) and better postoperative physical functioning (KOOS-PS) scores (OR 1.03, 95% CI 1.01–1.06) increased the likelihood of fulfilment. Preoperative sick leave (reported in 31%; OR 0.33, 95% CI 0.17–0.65) and postoperative difficulties at work due to knee complaints (reported in 56%; OR 0.41, 95% CI 0.17–0.98) decreased the likelihood of fulfilment (Table 2). Sensitivity analyses showed that a lower proportion of patients aged ≤ 55 had fulfilled expectations compared to those aged ≥ 56.
Twelve months postoperatively, six factors were below the cut-off value in the univariate analyses (musculoskeletal comorbidity, preoperative KOOS-PS, postoperative KOOS-PS, work tasks, preoperative sick leave, postoperative difficulties at work due to knee complaints; Table S4). Better postoperative physical functioning (OR 1.11. 95% CI 1.07–1.14) increased the likelihood of fulfilment. Physical work tasks (OR 0.20, 95% CI 0.06–0.69) decreased the likelihood of fulfilment (Table 3).
Discussion
This study investigated factors associated with fulfilment of patient expectations towards paid employment after THA or TKA at 6 and 12 months postoperatively. Six months after THA, 75% of patients had fulfilled expectations, increasing to 83% at 12 months postoperatively. Six months after TKA, 72% of patients had fulfilled expectations, increasing to 79% at 12 months postoperatively. Preoperative factors associated with fulfilment were older age, mental work tasks (compared to physical work tasks), and no sick leave due to knee complaints (only at 6 months postoperatively). Postoperative factors associated with fulfilment were better physical functioning, and no difficulties at work due to hip or knee complaints (only at 6 months postoperatively).
In our study, the majority of patients had high preoperative expectations towards paid employment, which is in line with the results of previous studies among THA and TKA patients [5, 9, 27]. The proportion of fulfilled expectations towards paid employment we found is also in line with previous literature among THA and TKA patients [10, 11]. Patient-specific education might create more realistic expectations on outcome, resulting in satisfaction and better postoperative outcomes of THA/TKA patients, and thus fulfilment of preoperative expectations [9, 28, 29].
We found that older age was associated with fulfilment 6 months after TKA and 12 months after THA. In-depth analyses showed that a lower proportion of patients aged ≤ 55 had fulfilled expectations compared to those aged ≥ 56. Results on the association between age and fulfilment among arthroplasty patients are conflicting [11, 30]. One study among TKA patients did not find an association [11], another study suggested that younger age of only THA patients, but not TKA patients, was associated with general fulfilment [30]. The contradictory results could be attributed to inclusion of all age groups, resulting in a different age distribution and also in a higher average age. Differences in methods (measurement of fulfilment and investigating overall or general fulfilment) and measurements at only 12 months postoperatively could also account for the contradiction.
Our results showing that better postoperative physical functioning after both THA and TKA was associated with fulfilled expectations, were in accordance with studies focusing on overall or general fulfilment after THA or TKA [10, 30].
Our study showed that preoperative sick leave decreased the likelihood of fulfilment after TKA at 6 months postoperatively. Patients who performed mainly physical tasks were less likely to have fulfilled expectations (THA at 6 and 12 months postoperatively, TKA at 12 months postoperatively). Also, both THA and TKA patients with postoperative difficulties at work due to hip or knee complaints were less likely to have fulfilled expectations 6 months postoperatively. These results could not be compared to previous studies about expectation fulfilment, therefore further research is needed to confirm our results. Still, it is known that these factors also influence RTW outcomes after THA and TKA [31,32,33,34,35].
In a previous study on sex differences in expectations after THA and THA we found that both preoperative expectations and their fulfilment was higher in men then in women [36]. In our current study sex was not identified as a risk factor for fulfilment for paid employment. The conflicting results are probably due to the difference in study population, our study only included working-age patients with preoperative paid employment whereas the previous study also included older patients (age > 64) and without preoperative paid employment.
Implications
Patients beliefs and expectations have been linked to RTW among THA and TKA patients [37,38,39]. However, being returned to work does not inevitably mean that patients experience good work functioning. Hence, it is important to also look beyond RTW and focus on fulfilment of expectations towards paid employment and associated factors. Orthopaedic surgeons could use the results in the shared-decision making process for THA/TKA, to preoperatively manage patient expectations, and to assess whether additional RTW guidance is necessary. Further research is needed to unravel fulfilment of expectations towards paid employment. Furthermore, the results show that some factors influencing fulfilment may be modifiable (i.e. work tasks, difficulties at work due to hip or knee complaints) and could be targeted by the occupational physician or the employer. Our results thus suggest that orthopaedic surgeons, occupational physicians and employers may contribute to address those patients prone to unfulfillment.
Strengths and limitations
A strength of this study is its design, with outcome measures at both 6 and 12 months postoperatively and a relatively large sample size. Also, our study population resembles the population in the Dutch Arthroplasty Register (LROI) based on ASA-classification and BMI [6]. The proportion of females in our study was lower compared to the Dutch Arthroplasty Register, which might be the result of fewer females having paid work in general. However, in the LOAS the proportion females is the same as in the Dutch Arthroplasty Register, therefore, generalizability of the results to the Dutch arthroplasty population is another strength.
Study limitations included the self-reported data used in the study. BMI was derived from self-reported body height and weight which may have introduced extra measurement error. The assessment of patient expectations and their fulfilment, which was measured with only one item of the validated HSS questionnaire. However, there is no questionnaire specifically focussing on expectations towards paid employment. The HSS questionnaire was originally developed to assess preoperative expectations [25], yet other studies have used the same approach to determine postoperative fulfilment [10, 12, 30]. The majority of patients who were lost to follow-up were male and performed mainly mental work tasks. Male sex has previously been linked to loss to follow-up [40]. The loss to follow-up of patients with mainly mental work tasks might have diluted our results to some extent. Last, it remains unknown why patients answered “not applicable”, since they all were of working-age and had a paid job preoperatively. The majority of these patients performed mainly mental work tasks (THA 56%; TKA 43%) and a lower proportion was preoperatively on sick leave (THA 9%; TKA 9%). It could be that these patients had no expectations or expected deterioration, or that their osteoarthritis complaints did not affect their work and therefore had no expectations.
Conclusions
This study illustrates that only three out of four THA or TKA patients have fulfilled expectations 6 months after surgery. Older age, mental work tasks, no preoperative sick leave, better postoperative physical functioning, and no postoperative difficulties at work were identified as factors that increased the likelihood of fulfilment of patient expectations towards paid employment after THA or TKA. Further quantitative and qualitative research is necessary to explore which factors influence patient expectation fulfilment towards paid employment, to eventually design and implement effective targeting strategies to appropriately address and support those prone to unfulfillment, and to better match preoperative expectations and postoperative fulfilment after THA or TKA.
Availability of data and materials
The data underlying this article were provided by the LOAS study group with permission. The data will be shared upon reasonable request to the corresponding author, with permission of the LOAS study group.
References
Waddell G, Burton AK (2006) Is work good for your health and well-being. The Stationery Office, London, UK
Van Leemput D, Neirynck J, Berger P, Vandenneucker H (2022) Return to work after primary total knee arthroplasty under the age of 65 years: a systematic review. J Knee Surg 35(11):1249–1259. https://doi.org/10.1055/S-0040-1722626
Hoorntje A, Janssen KY, Bolder SBT et al (2018) The effect of total hip arthroplasty on sports and work participation: a systematic review and meta-analysis. Sports Med 48(7):1695–1726. https://doi.org/10.1007/s40279-018-0924-2
Tilbury C, Schaasberg W, Plevier JW, Fiocco M, Nelissen RG, Vliet Vlieland TP (2014) Return to work after total hip and knee arthroplasty: a systematic review. Rheumatology (Oxford) 53(3):512–525. https://doi.org/10.1093/rheumatology/ket389
Witjes S, van Geenen RC, Koenraadt KL et al (2017) Expectations of younger patients concerning activities after knee arthroplasty: are we asking the right questions? Qual Life Res 26(2):403–417. https://doi.org/10.1007/s11136-016-1380-9
LROI Report 2021 (2021) Information on orthopaedic prosthesis procedures in the Netherlands 2021. www.lroi-report.nl/app/uploads/ 2022/04/PDF-LROI-annual-report-2021.pdf. Accessed 18 July 2022
Singh JA, Yu S, Chen L, Cleveland JD (2019) Rates of total joint replacement in the United States: future projections to 2020–2040 using the national inpatient sample. J Rheumatol 46(9):1134–1140. https://doi.org/10.3899/jrheum.170990
Leitner L, Türk S, Heidinger M et al (2018) Trends and economic impact of hip and knee arthroplasty in central europe: findings from the austrian national database. Sci Rep 8(1):4707. https://doi.org/10.1038/s41598-018-23266-w
Mancuso CA, Jout J, Salvati EA, Sculco TP (2009) Fulfillment of patients’ expectations for total hip arthroplasty. J Bone Jt Surg Am 91(9):2073–2078. https://doi.org/10.2106/JBJS.H.01802
Palazzo C, Jourdan C, Descamps S et al (2014) Determinants of satisfaction 1 year after total hip arthroplasty: the role of expectations fulfilment. BMC Musculoskelet Disord 15:53. https://doi.org/10.1186/1471-2474-15-53
Deakin AH, Smith MA, Wallace DT, Smith EJ, Sarungi M (2019) Fulfilment of preoperative expectations and postoperative patient satisfaction after total knee replacement. A prospective analysis of 200 patients. Knee 26(6):1403–1412. https://doi.org/10.1016/j.knee.2019.07.018
Tilbury C, Haanstra TM, Leichtenberg CS et al (2016) Unfulfilled expectations after total hip and knee arthroplasty surgery: there is a need for better preoperative patient information and education. J Arthroplast 31(10):2139–2145. https://doi.org/10.1016/j.arth.2016.02.061
Soleimani M, Babagoli M, Baghdadi S et al (2023) Return to work following primary total hip arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res 18(1):95. https://doi.org/10.1186/s13018-023-03578-y
Hylkema TH, Brouwer S, Stewart RE et al (2022) Two-year recovery courses of physical and mental impairments, activity limitations, and participation restrictions after total knee arthroplasty among working-age patients. Disabil Rehabil 44(2):291–300. https://doi.org/10.1080/09638288.2020.1766583
Davis AM, Perruccio AV, Ibrahim S et al (2011) The trajectory of recovery and the inter-relationships of symptoms, activity and participation in the first year following total hip and knee replacement. Osteoarthr Cartil 19(12):1413–1421. https://doi.org/10.1016/j.joca.2011.08.007
Harmsen RTE, Haanstra TM, Den Oudsten BL et al (2020) A high proportion of patients have unfulfilled sexual expectations after TKA: a prospective study. Clin Orthop Relat Res 478(9):2004–2016. https://doi.org/10.1097/CORR.0000000000001003
van de Water RB, Leichtenberg CS, Nelissen RGHH et al (2019) Preoperative radiographic osteoarthritis severity modifies the effect of preoperative pain on pain/function after total knee arthroplasty results at 1 and 2 years postoperatively. J Bone Jt Surg Am 101(10):879–887. https://doi.org/10.2106/JBJS.18.00642
World Medical Association (2013) World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310(20):2191–2194. https://doi.org/10.1001/jama.2013.281053
Centraal Bureau voor de Statistiek (CBS) [Central Bureau Statistics The Netherlands] (2010) Zelfgerapporteerde medische consumptie, gezondheid en leefstijl
Leichtenberg CS, Vliet Vlieland TPM, Kroon HM et al (2018) Self-reported knee instability associated with pain, activity limitations, and poorer quality of life before and 1 year after total knee arthroplasty in patients with knee osteoarthritis. J Orthop Res 36(10):2671–2678. https://doi.org/10.1002/jor.24023
Davis AM, Perruccio AV, Canizares M et al (2008) The development of a short measure of physical function for hip OA HOOS-Physical Function Shortform (HOOS-PS): an OARSI/OMERACT initiative. Osteoarthr Cartil 16(5):551–559. https://doi.org/10.1016/j.joca.2007.12.016
Davis AM, Perruccio AV, Canizares M et al (2009) Comparative, validity and responsiveness of the HOOS-PS and KOOS-PS to the WOMAC physical function subscale in total joint replacement for osteoarthritis. Osteoarthr Cartil 17(7):843–847. https://doi.org/10.1016/j.joca.2009.01.005
Perruccio AV, Stefan Lohmander L, Canizares M et al (2008) The development of a short measure of physical function for knee OA KOOS-physical function shortform (KOOS-PS) - an OARSI/OMERACT initiative. Osteoarthr Cartil 16(5):542–550. https://doi.org/10.1016/j.joca.2007.12.014
Ware JE, Kosinki M, Keller SD (1995) How to score SF-12 physical and mental health summary scales. The Health Institute, New England Medical Center, Boston
van den Akker-Scheek I, van Raay JJ, Reininga IH, Bulstra SK, Zijlstra W, Stevens M (2010) Reliability and concurrent validity of the Dutch hip and knee replacement expectations surveys. BMC Musculoskelet Disord 11:242. https://doi.org/10.1186/1471-2474-11-242
Hosmer DW, Lemeshow S, Sturdivant RX (2013) Applied logistic regression, 3rd edn. Wiley. https://doi.org/10.1002/9781118548387
van Zaanen Y, van Geenen RCI, Pahlplatz TMJ et al (2019) Three out of ten working patients expect no clinical improvement of their ability to perform work-related knee-demanding activities after total knee arthroplasty: a multicenter study. J Occup Rehabil 29(3):585–594. https://doi.org/10.1007/s10926-018-9823-5
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63. https://doi.org/10.1007/s11999-009-1119-9
Tolk JJ, Janssen RPA, Haanstra TM, van der Steen MC, Bierma-Zeinstra SMA, Reijman M (2021) The influence of expectation modification in knee arthroplasty on satisfaction of patients: a randomized controlled trial. Bone Jt J 103-B(4):619–626. https://doi.org/10.1302/0301-620X.103B4.BJJ-2020-0629.R3
Scott CE, Bugler KE, Clement ND, MacDonald D, Howie CR, Biant LC (2012) Patient expectations of arthroplasty of the hip and knee. J Bone Jt Surg Br 94(7):974–981. https://doi.org/10.1302/0301-620X.94B7.28219
Kamp T, Brouwer S, Hylkema TH et al (2022) Psychosocial working conditions play an important role in the return-to-work process after total knee and hip arthroplasty. J Occup Rehabil 32(2):295–305. https://doi.org/10.1007/s10926-021-10006-7
Sankar A, Davis AM, Palaganas MP, Beaton DE, Badley EM, Gignac MA (2013) Return to work and workplace activity limitations following total hip or knee replacement. Osteoarthr Cartil 21(10):1485–1493. https://doi.org/10.1016/j.joca.2013.06.005
Kleim BD, Malviya A, Rushton S, Bardgett M, Deehan DJ (2015) Understanding the patient-reported factors determining time taken to return to work after hip and knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(12):3646–3652. https://doi.org/10.1007/s00167-014-3265-1
Kuijer PP, Kievit AJ, Pahlplatz TM et al (2016) Which patients do not return to work after total knee arthroplasty? Rheumatol Int 36(9):1249–1254. https://doi.org/10.1007/s00296-016-3512-5
Leichtenberg CS, Tilbury C, Kuijer P et al (2016) Determinants of return to work 12 months after total hip and knee arthroplasty. Ann R Coll Surg Engl 98(6):387–395. https://doi.org/10.1308/rcsann.2016.0158
Latijnhouwers DAJM, Vlieland TPMV, Marijnissen WJ et al (2023) Sex differences in perceived expectations of the outcome of total hip and knee arthroplasties and their fulfillment: an observational cohort study. Rheumatol Int 43(5):911–922. https://doi.org/10.1007/s00296-022-05240-y
Mj Pahlplatz T, Schafroth MU, Kuijer PP (2017) Patient-related and work-related factors play an important role in return to work after total knee arthroplasty: a systematic review. JISAKOS 2:127–132. https://doi.org/10.1136/jisakos-2016-000088
Hoorntje A, Leichtenberg CS, Koenraadt KLM et al (2018) Not physical activity, but patient beliefs and expectations are associated with return to work after total knee arthroplasty. J Arthroplast 33(4):1094–1100. https://doi.org/10.1016/j.arth.2017.11.032
Al-Hourani K, MacDonald DJ, Turnbull GS, Breusch SJ, Scott CEH (2021) Return to work following total knee and hip arthroplasty: the effect of patient intent and preoperative work status. J Arthroplast 36(2):434–441. https://doi.org/10.1016/j.arth.2020.08.012
Zelle BA, Buttacavoli FA, Shroff JB, Stirton JB (2015) Loss of follow-up in orthopaedic trauma: who is getting lost to follow-up? J Orthop Trauma 29(11):510–515. https://doi.org/10.1097/BOT.0000000000000346
Acknowledgements
We would like to acknowledge the members of the LOAS study group in addition to the authors: H.M.J. van der Linden, Leiden University Medical Center, Leiden; B.L. Kaptein, Leiden University Medical Center, Leiden; S.H.M. Verdegaal, Alrijne Hospital, Leiden/Leiderdorp; P.J. Damen, Waterland Hospital, Purmerend; S.B.W Vehmeijer, Reinier de Graaf Hospital, Delft; W.C.M. Marijnissen, Albert Schweitzer Hospital, Dordrecht; H.H. Kaptijn, LangeLand Hospital, Zoetermeer; R. Onstenk, Groene Hart Hospital, Gouda: all in the Netherlands. Our gratitude goes out to all the patients and colleagues from the participating hospitals for their willingness to collaborate in this project.
Funding
The data used in this work was supported by the Dutch Arthritis Foundation [grant number LLP13]. The study sponsor had no involvement in the interpretation of data, the writing of the manuscript or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
All authors have made substantial contributions to this manuscript: TK, MS, TPMVV, RGHHN, SB, MGJG: conception and design, provision of study materials. TK: collection and assembly of data. TK, MGJG: analysis and interpretation of the data. TK, MS, SB, MGJG: drafting the article. All authors critically revised the work for important intellectual content, approved the version to be submitted and take responsibility of the integrity of the work as a whole, from inception to finished article. Additionally, all authors are in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors report there are no competing interests to declare.
Ethical approval and consent to participate
Informed consent was obtained from all patients prior to the study in conformity with the Declaration of Helsinki. Ethical approval was obtained from the Medical Ethics Committee of Leiden University Medical Center (registration no. P12.047; Trial ID NTR3348).
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An abstract of this study was presented at the NOF congress 2022 on 7–9 September in Vilnius, Lithuania. 8.2. Factors associated with expectation fulfilment towards paid employment after total hip and knee arthroplasty’ (2022) in Online Abstract Book—Nordic Orthopaedic Federation (NOF) Congress, pp. 66–68.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kamp, T., Stevens, M., Vlieland, T.P.M.V. et al. Three out of four working-age patients have fulfilled expectations towards paid employment six months after total hip or knee arthroplasty: a multicentre cohort study. Rheumatol Int 44, 339–347 (2024). https://doi.org/10.1007/s00296-023-05437-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-023-05437-9